This study provides a comprehensive assessment of past and future heat-related mortality in Portugal’s Alentejo region. Using a robust case time series approach, we present the first analysis of mortality risks and impacts at both regional and subregional levels, accounting for fine-scale epidemiological variations across territories. This approach minimizes exposure misclassification and reduces bias. In addition, by capturing the complex non-linear and delayed effects of temperature exposure on mortality and controlling for both time-static inter-municipal and time-dynamic intra-municipal confounders, we enhanced the precision and accuracy of our estimates [25, 26].
Our findings reveal an exponential risk of mortality after exceeding the optimum mean temperature (MMT = 19ºC), with risk peaking on the exposure day and persisting for up to five days at elevated temperatures. This pattern is qualitatively consistent with previous research in several regions and cities, including the Lisbon metropolitan area, Portugal [45], multiple Mediterranean cities [22], and Hulunbuir in China [46]. However, our region-specific MMT and associated mortality risks at proximate temperatures, differ from a broader European analysis [14], which included data from Alentejo between 1998 and 2012. In this study, a 5–24% risk increase was reported at daily mean temperatures of approximately 26ºC and 29ºC relative to an optimum temperature of approximately 23.5ºC. In contrast, we observed an increase from 8 to 45% at temperatures of 24.7ºC and 28.7ºC. These disparities likely result from our refined, municipality-level, model-driven MMT estimation, contrasting with the broader regional aggregations, which are more prone to biases. The subperiod analyses further support this issue, by excluding disparities resulting from data reflecting temporal shifts in the MMT. The most recent interval (1998–2015) closely aligns with the European analysis, with its specific MMT consistent with that of earlier subperiods (1980–1997) and the overall period. This contrasts with São Paulo, Brazil, where a 1.7ºC rise in MMT and a decrease in heat-related risks were reported between 2000 and 2018 [10]. While no significant correlation was found between MMT and annual mean temperature, some association between risks and annual extreme heat was observed across different population groups. It was hypothesised that both climatic and non-climatic adaptation, such as improved health care coverage and healthier lifestyles, contributed to this trend. In our study, while no long-term decrease in heat sensitivity was observed via changes in the MMT, lower mortality risks in the most recent subperiod suggest some degree of adaptation, though this was not statistically significant. Additional factors potentially contributing to the Alentejo population’s adaptative response might include increased awareness of heat-related health impacts and the rise in residential air conditioning, a key behavioral strategy for reducing heat strain [8,9,10].
On the other hand, our seasonal analysis does not show any substantial shift in MMT, though risk magnitudes increase in late summer without reaching statistical significance. Another study [47], assuming decadal acclimatisation, reported an increase in heat-related risk and deaths in Prague, Czech Republic, over the last two decades, attributed to both climatic factors and poor adaptation, such as the lack of heat-health warning systems. Considering our results and the upward trajectory in heat-related mortality – approximately in 5,296.4 deaths in Alentejo, between 1980 and 2015 – this may indicate a poor overall adaptation to increasing temperatures and more frequent hot days across the extended summer. The effectiveness of the current early warning system may be contributing to this scenario. In Alentejo, where the population is presumed to have greater heat tolerance (physiological acclimatisation), red alerts are triggered at 35ºC in May-June (vs. 32ºC in other regions), and at 38ºC in July-September (vs. 35ºC). However, our findings did not show evidence of short-term adaptation over the summer, as observed elsewhere [38]. Instead, the higher risks during summer peak suggest a limited capacity for adaptation to more frequent and/or intense heat. Moreover, the number of days with observed-forecasted temperatures excludes the acute effects of single-day exposures and any delayed effects. While exceptional heatwaves, such as the 2003 event that accounted for 35.68% of all deaths in Alentejo, underscore the gravity of prolonged extreme events, the most significant impact of heat often occurs on single hot days or during periods with moderately high, but frequent, temperatures [48]. Such pattern may have implications for the effectiveness of health prevention plans focused on extreme and prolonged temperatures. For example, in Spain, provinces that implemented more actions from their plan saw stronger reductions in mortality attributable to extreme heat, but not to moderate temperatures [49]. Therefore, the current regional assumptions and criteria may be overly aspirational, potentially overlooking significant negative effects. While acknowledging the potential ineffectiveness of frequent warnings due to desensitisation or disregard [50], notifications should be issued in a timely manner, before the onset of critical heat events, rather than on the event itself [51], as practiced in some European countries [52]. Complementary strategies, such as psychoeducation, may play a vital role in raising awareness and preparedness [19] for ongoing and more moderate hazards.
In addition, the specificity of trigger thresholds is critical for enhancing the confidence and efficacy of the prevention systems. This involves greater understanding of the exposure-response curve, which should further be integrated with forecasted and monitored atmospheric indicators [3, 5,6,7, 19, 20]. While we acknowledge the contribution of the íCARO-alert-index in monitoring potential mortality excess during warmer or heatwave periods, it is important to note that it relies on a linear regression model with a simple lag structure and dynamic maximum temperature thresholds, assuming within-summer population adaptation to heat [18]. These factors may introduce biases and underestimate mortality effects compared to more flexible methods like the DLNM [20, 38, 53] employed in our study.
In our thorough risk evaluation, the daily mean temperature emerged as a practical metric, capturing the impact of two crucial daily thresholds [3]. The reduced thermal amplitude caused by increased minimum temperatures exacerbates heat stress, limiting the body’s ability to recover from daytime exposure. Thus, daily mean temperature might provide a more accurate reflection of overall heat exposure than either maximum or minimum temperatures [48], while also offering improved interpretability for effective decision-making. This study revealed increased risks above the regional optimum temperature across all subregions, although no significant inter-regional variability was observed. While indicating comparable heat vulnerabilities, Alentejo Litoral showed a slightly steeper association slope, which may reflect differential acclimatisation processes. The maritime influence on the climate in this area, where populations in cooler regions often exhibit lower heat tolerance compared to those accustomed to warmer climates [13, 54, 55], could contribute to this pattern. However, the highest risks do not necessarily correspond to the highest net impact, as it depends on the frequency and intensity of nonoptimal exposures. Consequently, Alto Alentejo reported the highest mortality burden, accounting for 3.57% of all deaths in the subregion between 1980 and 2015. Further investigation is warranted to explore heterogeneities related to health aspects (e.g., prevalence of chronic conditions), population characteristics (e.g., age composition, population density), atmospheric-related variables (e.g., humidity levels, wind speed), topographical and environmental factors (e.g., vegetation indexes, urban vs. rural settings), socioeconomic indicators (e.g., income levels, educational attainment, deprivation indices) and infrastructural conditions (e.g., housing quality, air conditioning availability, access to healthcare) [26, 56].
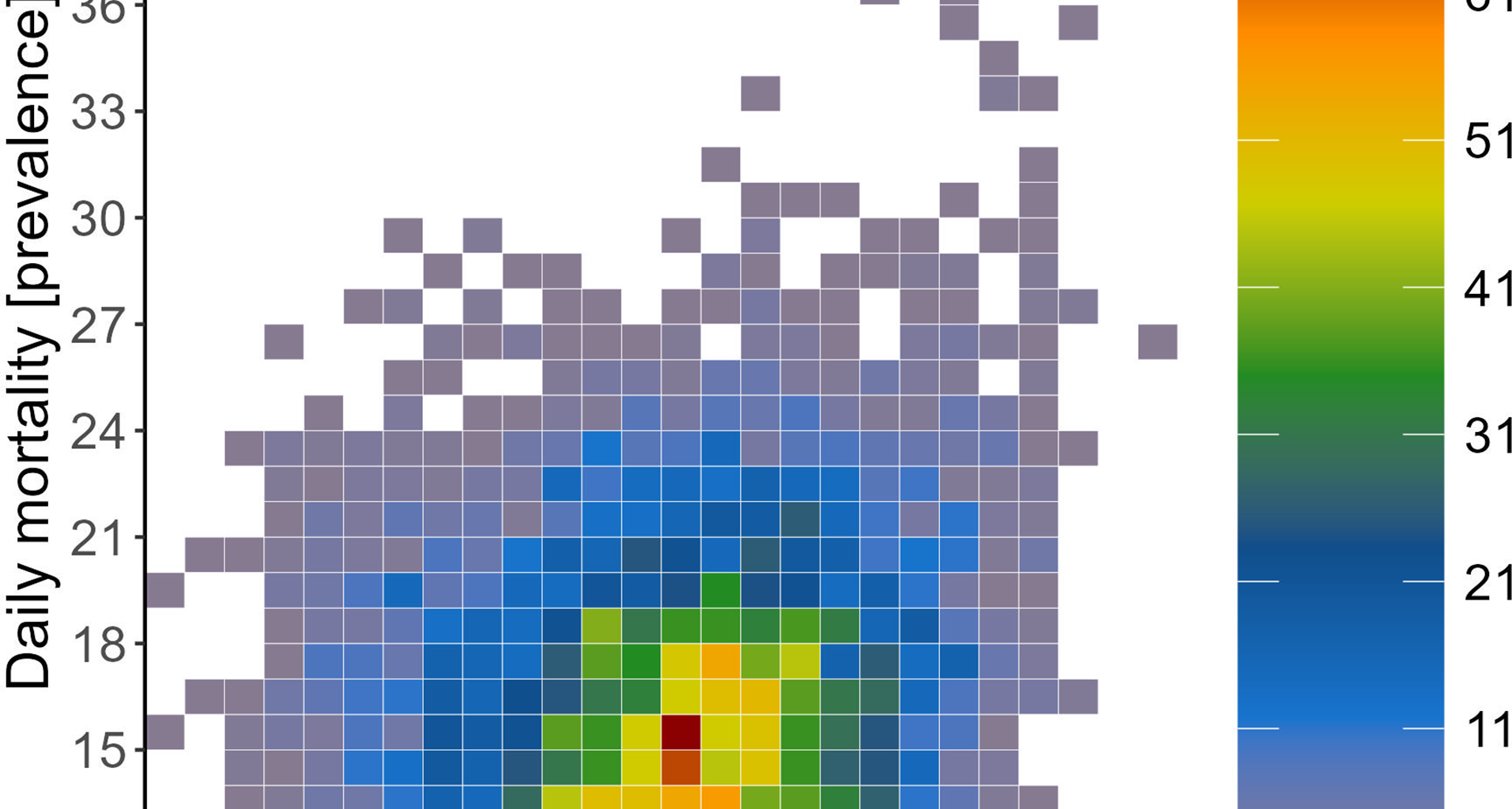
Projections suggest a marked increase in the future burden of heat-related mortality in Alentejo and its subregions over the coming decades. Under the higher emission scenario (RCP8.5), regional heat-related mortality is expected to more than quadruple by the end of the century (2081–2100), reaching a relative excess of 15.88% compared to the 3.64% estimated for the past two decades. Under the lower emissions pathway (RCP4.5), the long-term hazard could be reduced by more than 50%, lowering the relative excess to 6.61%. Similar qualitative findings were reported in a multi-country-city study [53], where hotter climates, such as southern Europe, showed a heightened impact in both scenarios. In contrast to our results, the European study [14] projected a s smaller shift of 4–5% by 2070–2099, relative to 1976–2005, for the Alentejo under the worst-case scenario. These discrepancies likely stem from differences in simulated climatologies, as well as variations in spatial scopes, datasets, and methodologies. While all studies employed the same bias correction method, our approach differed by utilising the outputs of RCMs instead of GCMs. Regional models are expected to add climatic detail, reduce biases and adjust climate change signals of the driving global models [57], hence contributing to the specificity of our analysis. Given the consistent and escalating heat impacts projected across all subregions until 2100 – with both scenarios showing similar magnitudes until 2040 – generalised and immediate implementation of adaptative policies and actions is crucial to mitigate the pervasive effects of heat.
Alongside the major strengths of the current study, there are some limitations that warrant acknowledgment. First, our analysis did not account for effect modifiers or environmental time-varying confounders, like air pollution and humidity. As the effects of climate change become more pronounced, the common co-occurrence of extreme temperature events in conjunction with elevated pollution levels is expected to rise, and meta-analytical evidence suggests that higher levels of PM10 and ozone elevate the heat-related all-cause and non-accidental mortality [58]. Moreover, some studies indicate that dry-hot events may pose a higher risk of mortality than wet-hot events [59], though the synergetic effects remain controversial [60].
Additionally, we did not examine the temperature-mortality associations by levels of particular clinical and demographic factors. One study [15], for example, reported strongest effects related to respiratory and cardiovascular mortality. However, as the implied level of data disaggregation would prevent the provider from releasing the data, we could not disentangle this type of vulnerability. Despite this limitation, we increased the specificity and interpretability of our findings by excluding external causes (e.g., suicides) and mental and behavioural disorders which might have a multifactorial etiology [61, 62], rather than a direct sensitivity to temperature. This exclusion, however, means that our results may not generalize to mental health conditions. Consistent differential susceptibility to heat-induced harm is also found in the elderly population [8, 15, 46, 56, 63]. More than 80% of the included deaths in our dataset occurred among individuals older than 65 years. Therefore, conducting specific analyses for this subgroup may not substantially alter the results. Furthermore, age stratification could have restricted our ability to provide stable and precise estimates. While this is a limitation, the predominance of older adults in our study population underscores their vulnerability to the adverse effects of heat. On the other hand, the ageing trajectory in Alentejo amplifies concerns, as the ageing index for the region has risen from 161.9% in 2001 to 214.9% by 2022 [64]. Such demographic shifts could also exacerbate the projected mortality burden [8, 63, 65, 66]. However, like previous studies [14, 36, 67, 68], we did not account for potential demographic shifts or ongoing adaptations to heat. As a result, our projections may be underestimated in some respects and overestimated in others. Future research could benefit from integrating region-specific population projections and potential acclimatization adjustments with the latest advancements in climate modelling, such as the CMIP6 models featured in IPCC’s AR6 [69]. These models incorporate new emissions and concentration pathways (RCPs), combined with different socioeconomic futures—known as Shared Socioeconomic Pathways (SSPs)—and account for various climate policy-driven mitigation responses throughout the 21st century [2]. Incorporating such updates, especially when extended to regional climate simulations and integrated with global warming thresholds (e.g., + 1.5 °C, + 2.0 °C, + 3.0 °C above pre-industrial levels) [70], could enhance the accuracy of regional projections, and increase confidence in projected changes, while aligning with global policy targets.
Finally, our approach does not account for the inherent uncertainty in the functional trend used to extrapolate exposure-response curves beyond the observed temperatures [36]. This leaves a portion of the epidemiological uncertainty in the projected impacts unaccounted for, adding to the substantial uncertainty arising from the imprecision in observed temperature-mortality associations and climatic projections. This complexity underscores the challenges in accurately assessing the full impact of climate change on heat-related health outcomes. Despite these limitations, our results clear demonstrate the effects of both mitigated and unmitigated scenarios on heat-related premature deaths through the end of the century.