Tham, Y.-C. et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121, 2081–2090 (2014).
Quigley, H. A. & Broman, A. T. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol. 90, 262–267 (2006).
Sun, Y. et al. Time trends, associations and prevalence of blindness and vision loss due to glaucoma: an analysis of observational data from the Global Burden of Disease Study 2017. BMJ Open 12, e053805 (2022).
Stein, J. D., Khawaja, A. P. & Weizer, J. S. Glaucoma in adults—screening, diagnosis, and management: a review. JAMA 325, 164–174 (2021).
Artes, P. H. & Chauhan, B. C. Longitudinal changes in the visual field and optic disc in glaucoma. Prog. Retin Eye Res. 24, 333–354 (2005).
Crabb, D. P., Smith, N. D., Glen, F. C., Burton, R. & Garway-Heath, D. F. How does glaucoma look?: patient perception of visual field loss. Ophthalmology 120, 1120–1126 (2013).
Kellman, P. J. & Shipley, T. F. A theory of visual interpolation in object perception. Cogn. Psychol. 23, 141–221 (1991).
Morgan, M. J. & Watt, R. J. Mechanisms of interpolation in human spatial vision. Nature 299, 553–555 (1982).
Nelson-Quigg, J. M., Cello, K. & Johnson, C. A. Predicting binocular visual field sensitivity from monocular visual field results. Investig. Ophthalmol. Vis. Sci. 41, 2212–2221 (2000).
Hu, S., Smith, N. D., Saunders, L. J. & Crabb, D. P. Patterns of binocular visual field loss derived from large-scale patient data from glaucoma clinics. Ophthalmology 122, 2399–2406 (2015).
Teng, B. et al. Inter-eye association of visual field defects in glaucoma and its clinical utility. Transl. Vis. Sci. Technol. 9, 22 (2020).
Shaikh, Y., Yu, F. & Coleman, A. L. Burden of undetected and untreated glaucoma in the United States. Am. J. Ophthalmol. 158, 1121–1129 (2014).
Chua, J. et al. Prevalence, risk factors, and visual features of undiagnosed glaucoma: the Singapore Epidemiology of Eye Diseases Study. JAMA Ophthalmol. 133, 938–946 (2015).
Rudnicka, A. R., Mt-Isa, S., Owen, C. G., Cook, D. G. & Ashby, D. Variations in primary open-angle glaucoma prevalence by age, gender, and race: a Bayesian meta-analysis. Investig. Ophthalmol. Vis. Sci. 47, 4254–4261 (2006).
Friedman, D. S., Jampel, H. D., Munoz, B. & West, S. K. The prevalence of open-angle glaucoma among blacks and whites 73 years and older: the Salisbury Eye Evaluation Glaucoma Study. Arch. Ophthalmol. 124, 1625–1630 (2006).
Hoevenaars, J. G. M. M., Schouten, J. S. A. G., Van Den Borne, B., Beckers, H. J. M. & Webers, C. A. B. Socioeconomic differences in glaucoma patients’ knowledge, need for information and expectations of treatments. Acta Ophthalmol. Scand. 84, 84–91 (2006).
Shweikh, Y. et al. Measures of socioeconomic status and self-reported glaucoma in the UK Biobank cohort. Eye 29, 1360–1367 (2015).
Sukumar, S., Spencer, F., Fenerty, C., Harper, R. & Henson, D. The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye 23, 1038–1044 (2009).
Musa, I., Bansal, S. & Kaleem, M. A. Barriers to care in the treatment of glaucoma: socioeconomic elements that impact the diagnosis, treatment, and outcomes in glaucoma patients. Curr. Ophthalmol. Rep. 10, 85–90 (2022).
Soh, Z. et al. The global extent of undetected glaucoma in adults. Ophthalmology 128, 1393–1404 (2021).
Halawa, O. A. et al. Racial and socioeconomic differences in eye care utilization among medicare beneficiaries with glaucoma. Ophthalmology 129, 397–405 (2022).
Halawa, O. A. et al. Race and ethnicity differences in disease severity and visual field progression among glaucoma patients. Am. J. Ophthalmol. 242, 69–76 (2022).
Kang, Jae H. et al. Cohort study of race/ethnicity and incident primary open-angle glaucoma characterized by autonomously determined visual field loss patterns. Transl. Vis. Sci. Technol. 11, 1–11 (2022).
Asaoka, R. et al. Using deep learning and transfer learning to accurately diagnose early-onset glaucoma from macular optical coherence tomography images. Am. J. Ophthalmol. 198, 136–145 (2019).
Ran, A. R. et al. Detection of glaucomatous optic neuropathy with spectral-domain optical coherence tomography: a retrospective training and validation deep-learning analysis. Lancet Digit. Health 1, e172–e182 (2019).
Medeiros, F. A., Jammal, A. A. & Mariottoni, E. B. Detection of progressive glaucomatous optic nerve damage on fundus photographs with deep learning. Ophthalmol. 128, 383–392 (2021).
Chen, X. et al. Automatic feature learning for glaucoma detection based on deep learning. In International Conference on Medical Image Computing and Computer-Assisted Intervention 669–677 (Springer International Publishing, 2015).
Li, Z. et al. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on color fundus photographs. Ophthalmology 125, 1199–1206 (2018).
Bojikian, K. D., Lee, C. S. & Lee, A. Y. Finding glaucoma in color fundus photographs using deep learning. JAMA Ophthalmol. 137, 1361–1362 (2019).
Kihara, Y. et al. Policy-driven, multimodal deep learning for predicting visual fields from the optic disc and OCT imaging. Ophthalmology 129, 781–791 (2022).
Christopher, M. et al. Deep learning approaches predict glaucomatous visual field damage from OCT optic nerve head En face images and retinal nerve fiber layer thickness maps. Ophthalmology 127, 346–356 (2020).
Quadrianto, N., Sharmanska, V. & Thomas, O. Discovering fair representations in the data domain. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition 8227–8236 (IEEE, 2019).
Xu, H., Liu, X., Li, Y., Jain, A. & Tang, J. To be robust or to be fair: Towards fairness in adversarial training. In International Conference on Machine Learning. 11492–11501 (PMLR, 2021).
Yang, J., Soltan, A. A. S., Eyre, D. W., Yang, Y. & Clifton, D. A. An adversarial training framework for mitigating algorithmic biases in clinical machine learning. NPJ Digit. Med. 6, 55 (2023).
Colby, S. L. & Ortman, J. M. Projections of the Size and Composition of the US Population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25-1143. (US Census Bureau, 2015).
Tan, M., & Le, Q. Efficientnet: Rethinking model scaling for convolutional neural networks. In International conference on machine learning. 6105-6114 (PMLR, 2019).
He, K., X. Zhang, S. Ren & J. Sun. Deep residual learning for image recognition. in IEEE Conference on Computer Vision and Pattern Recognition 770–778 (IEEE, 2016).
Zhou, Y. et al. A foundation model for generalizable disease detection from retinal images. Nature 622, 156–163 (2023).
Ji, S., Xu, W., Yang, M. & Yu, K. 3D convolutional neural networks for human action recognition. IEEE Trans. Pattern Anal. Mach. Intell. 35, 221–231 (2013).
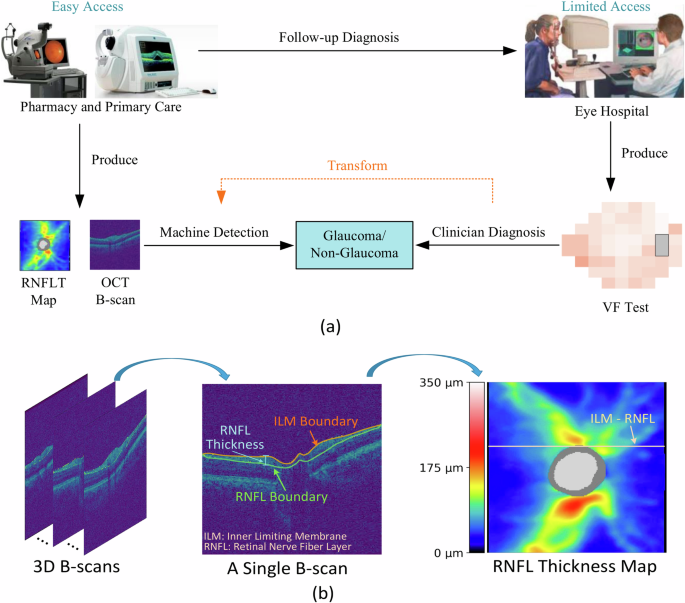
Huang, X. et al. GRAPE: a multi-modal dataset of longitudinal follow-up visual field and fundus images for glaucoma management. Sci. Data 10, 520 (2023).
Christopher, M. et al. Effects of study population, labeling and training on glaucoma detection using deep learning algorithms. Transl. Vis. Sci. Technol. 9, 27 (2020).
Shi, Min. et al. Artifact-tolerant clustering-guided contrastive embedding learning for ophthalmic images in glaucoma. IEEE J. Biomed. and Health Informatics. 27, 4329–4340 (2023).
Min, S. et al. Artifact correction in retinal nerve fiber layer thickness maps using deep learning and its clinical utility in glaucoma. Transl. Vis. Sci. Technol. 12, 12 (2023).
Wang, M. et al. Characterization of central visual field loss in end-stage glaucoma by unsupervised artificial intelligence. JAMA Ophthalmol. 138, 190 (2020).
Wang, M. et al. An artificial intelligence approach to assess spatial patterns of retinal nerve fiber layer thickness maps in glaucoma. Transl. Vis. Sci. Technol. 9, 41 (2020).
McInnes, L., Healy, J., Saul, N. & Großberger, L. UMAP: uniform manifold approximation and projection. J. Open Source Softw. 3, 861 (2018).
Dosovitskiy, A. et al. An image is worth 16×16 words: transformers for image recognition at scale. In International Conference on Learning Representations. (ICLR, 2020).