Over the last three decades, there has been a rise in the number and complexity of armed conflicts and related forced displacement, with the additional, often simultaneous, impact of disasters and climate change1. These further degrade health and eco-systems in fragile and conflict-affected settings contribute to environmental degradation and toxic waste production, stifling the potential for antimicrobial resistance (AMR) detection, mitigation and control2. These include negative impacts on water and sanitation3, diagnosis and surveillance, infection prevention and control and antimicrobial stewardship, all essential components of AMR control. Such degraded environmental conditions, rising temperatures and changing disease patterns due to climate change and natural disasters can fuel social and political tensions that can lead to conflicts. Alongside this, the humanitarian system is grappling with multiple crises amid funding shortfalls to key areas e.g. WASH4, vaccination5, enhancing healthcare service capacity, impacting on protracted crises, which, in turn, affect the ability of health systems and responses to address AMR effectively. As of 2024, 33 countries globally are affected by armed conflict and 110 million people are forcibly displaced globally (33.5 million as refugees (UNHCR/UNRWA) and 72.5 million are internally displaced people (IDPs)), numbers which are growing every year1. Arguably, these factors are increasing in scale and complexity and require high-level political support, global commitment and institutional investment to tackle them through evidence-based decision-making and tailored policies to address AMR in these settings. They also necessitate ground-up, contextualised evidence and sustainable approaches to address local concerns meaningfully.
Addressing AMR in settings affected by armed conflict and disasters requires targeted, evidence-driven, ground-up approaches which tackle the myriad drivers of AMR within these environments. For example, the breakdown of water and sanitation systems may lead to increased risks of infections, e.g. diarrhoeal illnesses, skin conditions, which can lead to over prescribing of antibiotics or inability to appropriately clean wounds, leading to further infections. Poor access to antibiotics through poor healthcare access or interrupted supply chains may lead to AMR through inappropriate use or overuse, particularly where there are poorly enforced policies or in acute armed conflicts where such measures are not respected. Such factors are compounded where there is inadequate or lack of diagnostic infrastructure for detection and epidemiological surveillance and limited capacity to interrupt to halt the spread through improved infection control2,6 Additionally, the voices of affected communities—service users and providers—must be centred in these discussions as they arguably hold both knowledge of the local contextual drivers and are integral to the solutions7,8. Engaging these communities enables a deeper understanding of the issues and helps in crafting customised solutions that effectively tackle local contributing factors. For example, if access to healthcare in general, and essential antimicrobials in particular, for refugees and migrants, is interrupted, it may contribute to behaviours which may lead to overuse, misuse, hoarding of antimicrobials or omission, which could lead to harm9. In other settings, the response to humanitarian crisis e.g. mobile clinics with a lack of diagnostics support, can potentially contribute to antimicrobial overprescribing or ineffective antibiotic choices. Additionally, there can be widespread concerns about counterfeit, substandard or poor-quality antibiotics with inadequate governance or quality control further exacerbating the issue.
Evidence from affected populations can also inform the responsibilities of wider transdisciplinary collaborators—including health practitioners, engineers, water, sanitation and hygiene (WASH/WATSAN) specialists, anthropologists, environmentalists, sociologists, politicians, and economists, among others—to prevent and tackle AMR in the particular contexts in which they exist10. This includes those who have been forcibly displaced into tented settlements, urban or peri-urban informal settlements and slums or who are living among host communities. This approach must also recognise the interconnectedness of human-animal-environment within the One Health framework in armed conflict settings, ensuring a comprehensive strategy against AMR11.
In the much anticipated zero draft12 of the political declaration on AMR, we see the initial framings, which aim to solidify AMR’s place in the global agenda in the lead-up to the United Nations High-Level Meeting (UNHLM) in September 2024. In the first iteration, while there is a commendable focus on access, there was a notable omission of the specific challenges areas affected by armed conflict or complex humanitarian crises face. Additionally, in the final political declaration, global targets put forward lack sufficient data to substantiate their effectiveness, relevance, and transformative potential in humanitarian settings. Failing to address the unique ecosystems of armed conflict and humanitarian crisis through tailored, transdisciplinary collaborations that extend beyond human health will fail to tackle AMR in these settings13. Beyond this, it is vital to explore the direct and indirect impacts of armed conflict and their role in unmasking or catalysing the emergence of AMR through various contributing factors.
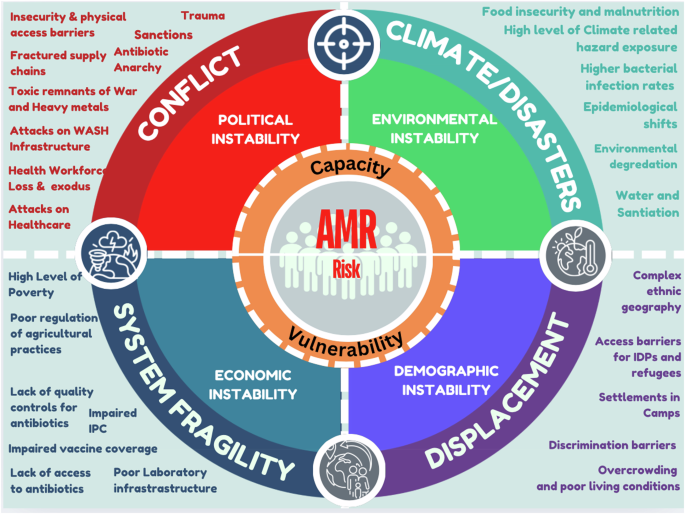
It is in this space that the breakdown of health care and essential infrastructure, including water and sanitation infrastructure, electricity and roads, coupled the loss or exodus of health workers, alongside ongoing violence and insecurity, can impede top-down approaches, such as policies and regulations relevant to AMR14. Health system governance in these areas is also disrupted, leading to poor enforcement of antimicrobial policies, weak infection control practices, substandard antimicrobials and their injudicious use in human, environmental and agricultural practices10. For example, poor stewardship of antimicrobial use in animal husbandry or dairy, poor animal welfare, improper carcass disposal and related environmental or water contamination can all exacerbate AMR or propagate its entry into the human food chain11. Additionally, surveillance is also hampered by inadequate microbiology capacity, data capture and reporting mechanisms, impacting on availability of essential data with proper regulatory and ethical oversight. As a result, the generation and consequences of AMR cannot be fully understood from one specific epistemological viewpoint, as they are inextricably linked to broader access challenges and their determinants, which is particularly evident in these settings. The interplay of such factors is summarised in Fig. 1.