Mensah, G. A. et al. Global burden of cardiovascular diseases and risks, 1990–2022. J. Am. Coll. Cardiol. 82 (25), 2350–2473 (2023).
WHO. SDG Target 3.4 Non-communicable diseases and mental health [Available from: https://www.who.int/data/gho/data/themes/topics/sdg-target-3_4-noncommunicable-diseases-and-mental-health.
Nouri, F. et al. Temporal trends of the incidence of ischemic heart disease in Iran over 15 years: A comprehensive report from a Multi-Centric Hospital-Based registry. Clin. Epidemiol. 12, 847–856 (2020).
Global burden and strength of evidence for. 88 Risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403 (10440), 2162–2203 (2024).
Francula-Zaninovic, S. & Nola, I. A. Management of measurable variable cardiovascular disease’ risk factors. Curr. Cardiol. Rev. 14 (3), 153–163 (2018).
MohammadEbrahimi, S., Dehghan, M. & Kiani, B. Cardiovascular health in perspective: a comprehensive five-year geodatabase of hospitalizations and environmental factors in Mashhad, Iran. BMC Res. Notes. 18 (1), 12 (2025).
Dastoorpoor, M. et al. Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci. Total Environ. 652, 1318–1330 (2019).
Dehghan, A., Khanjani, N., Bahrampour, A., Goudarzi, G. & Yunesian, M. Short-term effects of ambient (outdoor) air pollution on cardiovascular death in Tehran, Iran – a time series study. Toxin Reviews. 39 (2), 167–179 (2020).
Sajadi, H. S., Yahyaei, F., Ehsani-Chimeh, E. & Majdzadeh, R. The human cost of economic sanctions and strategies for Building health system resilience: A scoping review of studies in Iran. Int. J. Health Plann. Manage. 38 (5), 1142–1160 (2023).
Dugani, S. B., Moran, A. E., Bonow, R. O. & Gaziano, T. A. Ischemic Heart Disease: Cost-Effective Acute Management and Secondary Prevention. In: Prabhakaran D, Anand S, Gaziano TA, Mbanya JC, Wu Y, Nugent R, editors. Cardiovascular, Respiratory, and Related Disorders. Washington (DC): The International Bank for Reconstruction and Development / The World Bank © 2017 International Bank for Reconstruction and Development / The World Bank.; (2017).
Global incidence. prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403 (10440), 2133–2161 (2024).
Singh, A. K., Jyoti, B., Kumar, S. & Lenka, S. K. Assessment of global sustainable development, environmental sustainability, economic development and social development index in selected economies. Int. J. Sustainable Dev. Plann. 16 (1), 123–138 (2021).
IHME. Global Burden of Disease Study 2021. Causes of Death and Nonfatal Causes Mapped to ICD Codes 2024 [GBD (2021). Available from: https://ghdx.healthdata.org/record/ihme-data/gbd-2021-cause-icd-code-mappings.
Foreman, K. J., Lozano, R., Lopez, A. D. & Murray, C. J. Modeling causes of death: an integrated approach using codem. Popul. Health Metr. 10, 1 (2012).
Devleesschauwer, B. et al. DALY calculation in practice: a Stepwise approach. Int. J. Public. Health. 59 (3), 571–574 (2014).
Prabhakaran, D., Jeemon, P. & Roy, A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation 133 (16), 1605–1620 (2016).
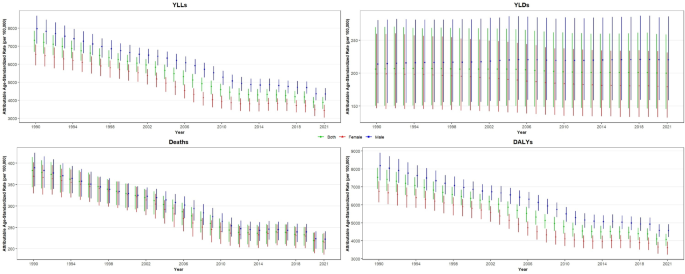
Koolaji, S. et al. A 30-year trend of ischemic heart disease burden in a developing country; a systematic analysis of the global burden of disease study 2019 in Iran. Int. J. Cardiol. 379, 127–133 (2023).
Wilson, L., Bhatnagar, P. & Townsend, N. Comparing trends in mortality from cardiovascular disease and cancer in the united Kingdom, 1983–2013: joinpoint regression analysis. Popul. Health Metrics. 15, 1–9 (2017).
Sadeghi, M., Haghdoost, A. A., Bahrampour, A. & Dehghani, M. Modeling the burden of cardiovascular diseases in Iran from 2005 to 2025: the impact of demographic changes. Iran. J. Public. Health. 46 (4), 506 (2017).
Mathers, C. D. & Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 3 (11), e442 (2006).
Kiani, S., Bayanzadeh, M., Tavallaee, M. & Hogg, R. S. The Iranian population is graying: are we ready? Arch. Iran. Med. 13 (4), 333–339 (2010).
Hosseini-Esfahani, F., Mousavi Nasl Khameneh, A., Mirmiran, P., Ghanbarian, A. & Azizi, F. Trends in risk factors for cardiovascular disease among Iranian adolescents: the Tehran lipid and glucose study, 1999–2008. J. Epidemiol. 21 (5), 319–328 (2011).
Akbarialiabad, H., Rastegar, A. & Bastani, B. How sanctions have impacted Iranian healthcare sector: A brief review. Arch. Iran. Med. 24 (1), 58–63 (2021).
Malekpour, M. R. et al. The burden of metabolic risk factors in North Africa and the middle East, 1990–2019: findings from the global burden of disease study. EClinicalMedicine 60, 102022 (2023).
Lababidi, H. et al. The global burden of premature cardiovascular disease, 1990–2019. Int. J. Cardiol. Cardiovasc. Risk Prev. 19, 200212 (2023).
Colafella, K. M. M. & Denton, K. M. Sex-specific differences in hypertension and associated cardiovascular disease. Nat. Rev. Nephrol. 14 (3), 185–201 (2018).
Connelly, P. J. et al. The importance of gender to understand sex differences in cardiovascular disease. Can. J. Cardiol. 37 (5), 699–710 (2021).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76 (25), 2982–3021 (2020).
Farzadfar, F. et al. National and subnational mortality effects of metabolic risk factors and smoking in Iran: a comparative risk assessment. Popul. Health Metr. 9 (1), 55 (2011).
Keykhaei, M. et al. Population attributable fraction estimates of cardiovascular diseases in different blood pressure levels in a large-scale cross-sectional study: a focus on prevention strategies and treatment coverage. Blood Press. Monit. 28 (1), 1–10 (2023).
Oori, M. J. et al. Prevalence of HTN in Iran: Meta-analysis of published studies in 2004–2018. Curr. Hypertens. Rev. 15 (2), 113–122 (2019).
Sepanlou, S. G. et al. Levels and trends of hypertension at National and subnational scale in Iran from 1990 to 2016: A systematic review and pooled analysis. Arch. Iran. Med. 24 (4), 306–316 (2021).
Peykari, N. et al. National action plan for non-communicable diseases prevention and control in Iran; a response to emerging epidemic. J. Diabetes Metab. Disord. 16, 3 (2017).
Azadnajafabad, S. et al. Population attributable fraction estimates of cardiovascular diseases in different levels of plasma total cholesterol in a large-scale cross-sectional study: a focus on prevention strategies and treatment coverage. J. Diabetes Metab. Disord. 19 (2), 1453–1463 (2020).
Faraji, O., Etemad, K., Akbari Sari, A. & Ravaghi, H. Policies and programs for prevention and control of diabetes in Iran: A document analysis. Glob J. Health Sci. 7 (6), 187–197 (2015).
Health system performance. In Iran: a systematic analysis for the global burden of disease study 2019. Lancet 399 (10335), 1625–1645 (2022).
Djalalinia, S. et al. Patterns of obesity and overweight in the Iranian population: findings of steps 2016. Front. Endocrinol. (Lausanne). 11, 42 (2020).
Gholami, A. et al. Identifying the pattern of unhealthy dietary habits among an Iranian population: A latent class analysis. Med. J. Islam Repub. Iran. 32, 69 (2018).
Heydari, G., Heidari, F., Yousefifard, M. & Hosseini, M. Smoking and diet in healthy adults: a cross-sectional study in Tehran, Iran, 2010. Iran. J. Public. Health. 43 (4), 485–491 (2014).
Yazdi Feyzabadi, V. et al. Factors associated with unhealthy snacks consumption among adolescents in Iran’s schools. Int. J. Health Policy Manag. 6 (9), 519–528 (2017).
Rezaei, S. et al. Salt intake among Iranian population: the first National report on salt intake in Iran. J. Hypertens. 36 (12), 2380–2389 (2018).
Mohammadi, E. et al. Epidemiologic pattern of cancers in Iran; current knowledge and future perspective. J. Diabetes Metab. Disord. 20 (1), 825–829 (2021).
Nejadghaderi, S. A. et al. Physical activity pattern in Iran: findings from STEPS 2021. Front. Public. Health. 10, 1036219 (2022).
Yarahmadi, S., Etemad, K., Hazaveh, A. M. & Azhang, N. Urbanization and non-communicable risk factors in the capital City of 6 big provinces of Iran. Iran. J. Public. Health. 42 (Supple1), 113–118 (2013).
Meysamie, A. et al. Pattern of tobacco use among the Iranian adult population: results of the National survey of risk factors of Non-Communicable diseases (SuRFNCD-2007). Tob. Control. 19 (2), 125–128 (2010).
Abbasi-Kangevari, M. et al. Tobacco consumption patterns among Iranian adults: a National and sub-national update from the STEPS survey 2021. Sci. Rep. 13 (1), 10272 (2023).
Abbasi-Kangavari, M. et al. Current inequities in smoking prevalence on district level in Iran: A systematic analysis on the STEPS survey. J. Res. Health Sci. 22 (1), e00540 (2021).
Levy, D. T., Yuan, Z., Luo, Y. & Mays, D. Seven years of progress in tobacco control: an evaluation of the effect of nations meeting the highest level MPOWER measures between 2007 and 2014. Tob. Control. 27 (1), 50–57 (2018).
Alimohammadi, M. et al. Review on the implementation of the Islamic Republic of Iran about tobacco control, based on MPOWER, in the framework convention on tobacco control by the world health organization. Addict. Health. 9 (3), 183–189 (2017).
Taghizadeh, F., Mokhtarani, B. & Rahmanian, N. Air pollution in Iran: the current status and potential solutions. Environ. Monit. Assess. 195 (6), 737 (2023).
Hadianfar, A., Küchenhoff, H., MohammadEbrahimi, S. & Saki, A. A novel Spatial heteroscedastic generalized additive distributed lag model for the Spatiotemporal relation between PM2.5and cardiovascular hospitalization. Sci. Rep. 14 (1), 29346 (2024).
Abbasi-Kangevari, M. et al. Effect of air pollution on disease burden, mortality, and life expectancy in North Africa and the middle East: a systematic analysis for the global burden of disease study 2019. Lancet Planet. Health. 7 (5), e358–e69 (2023).
Adesina, J. et al. Contrasting indoor and ambient particulate matter concentrations and thermal comfort in coal and non-coal burning households at South Africa highveld. Sci. Total Environ. 699, 134403 (2020).
Watts, N. et al. The 2020 report of the Lancet countdown on health and climate change: responding to converging crises. Lancet 397 (10269), 129–170 (2021).
Mahamad, M. M. A. et al. Influence of Lifestyle Changes on Cardiovascular Diseases in Saudi Ara bia: A Systematic Literature Review. Cureus. (2023).
Z, M., Sara, J., Mohammad, A. M., C, A. A. & Abdullah, M. AAR. Burden of disease, injuries, and risk factors in the Kingdom of Saudi Arabia, 1990–2010. Prev. Chronic Dis. (2014).
C, S. T., Majid, E. B. S. A. K. A. & Rajaa, A. A. A-R, et al. The burden of disease in Saudi Arabia 1990–2017: results from the glob al burden of disease study 2017. Lancet Planet. Health (2020).
Rami, H. R. AB, H H, N L, M K, R R. The epidemiology and economic burden of obesity and related cardiometa Bolic disorders in the united Arab Emirates: A systematic review and Q ualitative synthesis. J. Obes. (2018).
R, A. A. M, S K, S F, P S, J P, et al. The impact of dietary habits and metabolic risk factors on cardiovascu Lar and diabetes mortality in countries of the middle East and North A frica in 2010: a comparative risk assessment analysis. BMJ Open. (2015).
Puska, P. & Jaini, P. The North Karelia project: prevention of cardiovascular disease in Finland through Population-Based lifestyle interventions. Am. J. Lifestyle Med. 14 (5), 495–499 (2020).
Okayama, A. et al. Dietary sodium-to-potassium ratio as a risk factor for stroke, cardiovascular disease and all-cause mortality in Japan: the NIPPON DATA80 cohort study. BMJ Open. 6 (7), e011632 (2016).
He, F. J., Pombo-Rodrigues, S. & MacGregor, G. A. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 4 (4), e004549 (2014).
Walls, H. L., Peeters, A., Reid, C. M., Liew, D. & McNeil, J. J. Predicting the effectiveness of prevention: a role for epidemiological modeling. J. Prim. Prev. 29 (4), 295–305 (2008).