Longhitano, E. et al. The hypertensive disorders of pregnancy: a focus on definitions for clinical nephrologists. J. Clin. Med. 11, 3420 (2022).
Chappell, L. C., Cluver, C. A., Kingdom, J. & Tong, S. Pre-eclampsia. Lancet 398, 341–354 (2021).
Magee, L. A., Nicolaides, K. H. & von Dadelszen, P. Preeclampsia. N. Engl. J. Med. 386, 1817–1832 (2022).
Garovic, V. D. et al. Incidence and long-term outcomes of hypertensive disorders of pregnancy. J. Am. Coll. Cardiol. 75, 2323–2334 (2020).
Vikse, B. E., Irgens, L. M., Leivestad, T., Skjaerven, R. & Iversen, B. M. Preeclampsia and the risk of end-stage renal disease. N. Engl. J. Med. 359, 800–809 (2008).
Barrett, P. M. et al. Adverse pregnancy outcomes and long-term maternal kidney disease: a systematic review and meta-analysis. JAMA Netw. Open 3, e1920964 (2020).
Covella, B. et al. A systematic review and meta-analysis indicates long-term risk of chronic and end-stage kidney disease after preeclampsia. Kidney Int. 96, 711–727 (2019).
Garovic, V. D. & Piccoli, G. B. A kidney-centric view of pre-eclampsia through the kidney-placental bidirectional lens. Kidney Int. 104, 213–217 (2023).
Kattah, A. G. et al. Preeclampsia and ESRD: the role of shared risk factors. Am. J. Kidney Dis. 69, 498–505 (2017).
Cabiddu, G. et al. Pre-eclampsia is a valuable opportunity to diagnose chronic kidney disease: a multicentre study. Nephrol. Dial. Transpl. 37, 1488–1498 (2022).
Ibarra-Hernandez, M. et al. Acute kidney injury in pregnancy and the role of underlying CKD: a point of view from Mexico. J. Nephrol. 30, 773–780 (2017).
van Oostwaard, M. F. et al. Recurrence of hypertensive disorders of pregnancy: an individual patient data metaanalysis. Am. J. Obstet. Gynecol. 212, 624.e1–624.e17 (2015).
Dimitriadis, E. et al. Pre-eclampsia. Nat. Rev. Dis. Primers 9, 8 (2023).
Piccoli, G. B. et al. A best practice position statement on the role of the nephrologist in the prevention and follow-up of preeclampsia: the Italian study group on kidney and pregnancy. J. Nephrol. 30, 307–317 (2017).
Piccoli, G. B. et al. Women and kidney disease: reflections on World Kidney Day 2018. Kidney Int. 93, 278–283 (2018).
Innes, K. E., Marshall, J. A., Byers, T. E. & Calonge, N. A woman’s own birth weight and gestational age predict her later risk of developing preeclampsia, a precursor of chronic disease. Epidemiology 10, 153–160 (1999).
Luyckx, V. A. et al. A developmental approach to the prevention of hypertension and kidney disease: a report from the low birth weight and nephron number working group. Lancet 390, 424–428 (2017).
Homer, C. S., Brown, M. A., Mangos, G. & Davis, G. K. Non-proteinuric pre-eclampsia: a novel risk indicator in women with gestational hypertension. J. Hypertens. 26, 295–302 (2008).
[No authors listed] Gestational hypertension and preeclampsia: ACOG practice bulletin, number 222. Obstet. Gynecol. 135, e237–e260 (2020).
Magee, L. A. et al. The 2021 International Society for the Study of Hypertension in Pregnancy Classification, Diagnosis & Management recommendations for international practice. Pregnancy Hypertens. 27, 148–169 (2022).
[No authors listed] ACOG practice bulletin no. 202: gestational hypertension and preeclampsia. Obstet. Gynecol. 133, 1 (2019).
Society of Obstetric Medicine of Australia and New Zealand. Hypertension in Pregnancy Guideline 2023 (SOMANZ, 2024).
Metoki, H. et al. Hypertensive disorders of pregnancy: definition, management, and out-of-office blood pressure measurement. Hypertens. Res. 45, 1298–1309 (2022).
Verlohren, S. et al. Clinical interpretation and implementation of the sFlt-1/PlGF ratio in the prediction, diagnosis and management of preeclampsia. Pregnancy Hypertens. 27, 42–50 (2022).
Rolfo, A. et al. Chronic kidney disease may be differentially diagnosed from preeclampsia by serum biomarkers. Kidney Int. 83, 177–181 (2013).
Cabiddu, G. et al. A best practice position statement on pregnancy in chronic kidney disease: the Italian Study Group on Kidney and Pregnancy. J. Nephrol. 29, 277–303 (2016).
Wiles, K. et al. Clinical practice guideline on pregnancy and renal disease. BMC Nephrol. 20, 401 (2019).
Modzelewski, J. et al. Atypical preeclampsia before 20 weeks of gestation — a systematic review. Int. J. Mol. Sci. 24, 3752 (2023).
Magee, L. A. et al. Less-tight versus tight control of hypertension in pregnancy. N. Engl. J. Med. 372, 407–417 (2015).
Tita, A. T. et al. Treatment for mild chronic hypertension during pregnancy. N. Engl. J. Med. 386, 1781–1792 (2022).
Brewer, J. et al. Posterior reversible encephalopathy syndrome in 46 of 47 patients with eclampsia. Am. J. Obstet. Gynecol. 208, 468.e1–468.e6 (2013).
Hinchey, J. et al. A reversible posterior leukoencephalopathy syndrome. N. Engl. J. Med. 334, 494–500 (1996).
Garovic, V. D. et al. Hypertension in pregnancy: diagnosis, blood pressure goals, and pharmacotherapy: a scientific statement from the American Heart Association. Hypertension 79, e21–e41 (2022).
Santos, J., Schenone, M. H. & Garovic, V. D. Early identification of individuals at risk for hypertensive disorders of pregnancy. JAMA Netw. Open 6, e2334858 (2023).
Ananth, C. V., Keyes, K. M. & Wapner, R. J. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ 347, f6564 (2013).
Levine, R. J. et al. Trial of calcium to prevent preeclampsia. N. Engl. J. Med. 337, 69–76 (1997).
Say, L. et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob. Health 2, e323–e333 (2014).
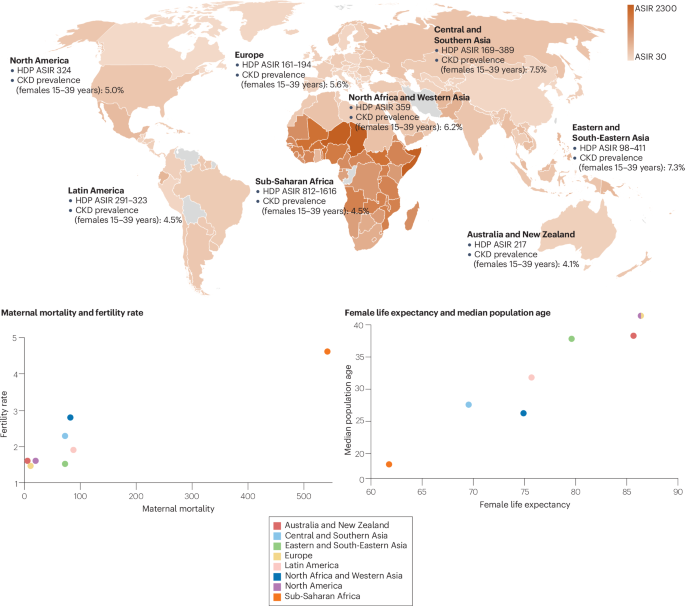
Wang, W. et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population-based study. BMC Pregnancy Childbirth 21, 364 (2021).
Bello, A. K. et al. An update on the global disparities in kidney disease burden and care across world countries and regions. Lancet Glob. Health 12, e382–e395 (2024).
Lopez, D. S., Hernandez Vargas, J. A., Urina-Jassir, M., Urina-Triana, M. & Franco, O. H. Reducing the gap of chronic kidney disease in low- and middle-income countries: what is missing? Lancet Reg. Health Am. 28, 100625 (2023).
Stanifer, J. W., Muiru, A., Jafar, T. H. & Patel, U. D. Chronic kidney disease in low- and middle-income countries. Nephrol. Dial. Transpl. 31, 868–874 (2016).
Torreggiani, M. et al. Unmet needs for CKD care: from the general population to the CKD clinics — how many patients are we missing? Clin. Kidney J. 14, 2246–2254 (2021).
Williams, D. & Davison, J. Chronic kidney disease in pregnancy. BMJ 336, 211–215 (2008).
Vrijlandt, W. A. L. et al. Prevalence of chronic kidney disease in women of reproductive age and observed birth rates. J. Nephrol. 36, 1341–1347 (2023).
United Nations Department of Economic and Social Affairs. World Population Prospects 2022: Summary of Results (UNDESA, 2022).
World Health Organization. Trends in Maternal Mortality 2000 to 2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division (WHO, 2023).
Wheeler, S. M., Myers, S. O., Swamy, G. K. & Myers, E. R. Estimated prevalence of risk factors for preeclampsia among individuals giving birth in the US in 2019. JAMA Netw. Open 5, e2142343 (2022).
Hannan, M. et al. Risk factors for CKD progression: overview of findings from the CRIC study. Clin. J. Am. Soc. Nephrol. 16, 648–659 (2021).
Dilmaghani, D., Nath, K. A. & Garovic, V. D. Increasing maternal mortality in the United States: looking beneath and beyond the numbers. Mayo Clin. Proc. 99, 873–877 (2024).
Daly, A. L. et al. Risk factors associated with hypertensive disorders of pregnancy within an urban indigenous population in south western Sydney. Intern. Med. J. 48, 269–275 (2018).
Austin, C. The impact of social determinants of health of Australian indigenous women on access and engagement in maternal child health services. J. Adv. Nurs. 79, 1815–1829 (2023).
Kendall, S., Lighton, S., Sherwood, J., Baldry, E. & Sullivan, E. A. Incarcerated aboriginal women’s experiences of accessing healthcare and the limitations of the ‘equal treatment’ principle. Int. J. Equity Health 19, 48 (2020).
Hoy, W. E., Hughson, M. D., Singh, G. R., Douglas-Denton, R. & Bertram, J. F. Reduced nephron number and glomerulomegaly in Australian aborigines: a group at high risk for renal disease and hypertension. Kidney Int. 70, 104–110 (2006).
Hoy, W. E., Mott, S. A. & Mc Donald, S. P. An expanded nationwide view of chronic kidney disease in aboriginal Australians. Nephrology 21, 916–922 (2016).
Sorensen, C. & Garcia-Trabanino, R. A new era of climate medicine — addressing heat-triggered renal disease. N. Engl. J. Med. 381, 693–696 (2019).
Gebremedhin, A. T., Nyadanu, S. D., Hanigan, I. C. & Pereira, G. Maternal exposure to bioclimatic stress and hypertensive disorders of pregnancy in Western Australia: identifying potential critical windows of susceptibility. Env. Sci. Pollut. Res. Int. 31, 52279–52292 (2024).
Rao, I. R. et al. Chronic kidney disease of unknown aetiology: a comprehensive review of a global public health problem. Trop. Med. Int. Health 28, 588–600 (2023).
Khan, A. E. et al. Salinity in drinking water and the risk of (pre)eclampsia and gestational hypertension in coastal Bangladesh: a case-control study. PLoS ONE 9, e108715 (2014).
Mondal, R., Banik, P. C., Faruque, M., Mashreky, S. R. & Ali, L. Association of exposure to salinity in groundwater with chronic kidney disease among diabetic population in Bangladesh. PLoS ONE 18, e0284126 (2023).
Scheelbeek, P. F., Khan, A. E., Mojumder, S., Elliott, P. & Vineis, P. Drinking water sodium and elevated blood pressure of healthy pregnant women in salinity-affected coastal areas. Hypertension 68, 464–470 (2016).
Demissie, M., Molla, G., Tayachew, A. & Getachew, F. Risk factors of preeclampsia among pregnant women admitted at labor ward of public hospitals, low income country of Ethiopia; case control study. Pregnancy Hypertens. 27, 36–41 (2022).
Beyuo, T. K. et al. Impact of antenatal care on severe maternal and neonatal outcomes in pregnancies complicated by preeclampsia and eclampsia in Ghana. Pregnancy Hypertens. 33, 46–51 (2023).
Nava, J. et al. Successful pregnancy in a CKD patient on a low-protein, supplemented diet: an opportunity to reflect on CKD and pregnancy in Mexico, an emerging country. J. Nephrol. 30, 877–882 (2017).
Orozco-Guillien, A. O. et al. Quality or quantity of proteins in the diet for CKD patients: does “Junk Food” make a difference? lessons from a high-risk pregnancy. Kidney Blood Press. Res. 46, 1–10 (2021).
Tyrmi, J. S. et al. Genetic risk factors associated with preeclampsia and hypertensive disorders of pregnancy. JAMA Cardiol. 8, 674–683 (2023).
Reidy, K. J. et al. Fetal-not maternal-APOL1 genotype associated with risk for preeclampsia in those with African ancestry. Am. J. Hum. Genet. 103, 367–376 (2018).
Dizon-Townson, D. et al. Impact of smoking during pregnancy on functional coagulation testing. Am. J. Perinatol. 29, 225–230 (2012).
Loisel, D. A. et al. The maternal HLA-G 1597ΔC null mutation is associated with increased risk of pre-eclampsia and reduced HLA-G expression during pregnancy in African-American women. Mol. Hum. Reprod. 19, 144–152 (2013).
Conklin, M. B. et al. Understanding health disparities in preeclampsia: a literature review. Am. J. Perinatol. 41, e1291–e1300 (2024).
Levine, R. J. et al. Circulating angiogenic factors and the risk of preeclampsia. N. Engl. J. Med. 350, 672–683 (2004).
Maynard, S. E. et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Invest. 111, 649–658 (2003).
Thadhani, R. et al. Circulating angiogenic factor levels in hypertensive disorders of pregnancy. NEJM Evid. 1, EVIDoa2200161 (2022).
US Food and Drug Administration. FDA roundup: May 19, 2023. FDA https://www.fda.gov/news-events/press-announcements/fda-roundup-may-19-2023 (2023).
Dupont, V. et al. Impaired renal reserve contributes to preeclampsia via the kynurenine and soluble fms-like tyrosine kinase 1 pathway. J. Clin. Invest. 132, e158346 (2022).
Broekhuizen, M., Danser, A. H. J., Reiss, I. K. M. & Merkus, D. The function of the kynurenine pathway in the placenta: a novel pharmacotherapeutic target? Int. J. Environ. Res. Public Health 18, 11545 (2021).
Yagel, S. et al. Expert review: preeclampsia type I and type II. Am. J. Obstet. Gynecol. MFM 5, 101203 (2023).
Kidney Disease: Improving Global Outcomes Working Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S117–S314 (2024).
Garovic, V. D. et al. Urinary podocyte excretion as a marker for preeclampsia. Am. J. Obstet. Gynecol. 196, 320.e1–320.e7 (2007).
Jim, B. et al. Podocyturia as a diagnostic marker for preeclampsia amongst high-risk pregnant patients. J. Pregnancy 2012, 984630 (2012).
Jim, B. et al. A comparison of podocyturia, albuminuria and nephrinuria in predicting the development of preeclampsia: a prospective study. PLoS ONE 9, e101445 (2014).
Nakamura, T. et al. Urinary podocytes for the assessment of disease activity in lupus nephritis. Am. J. Med. Sci. 320, 112–116 (2000).
Fisher, K. A., Luger, A., Spargo, B. H. & Lindheimer, M. D. Hypertension in pregnancy: clinical-pathological correlations and remote prognosis. Medicine 60, 267–276 (1981).
Gilani, S. I. et al. Urinary extracellular vesicles of podocyte origin and renal injury in preeclampsia. J. Am. Soc. Nephrol. 28, 3363–3372 (2017).
Weissgerber, T. L., Milic, N. M., Milin-Lazovic, J. S. & Garovic, V. D. Impaired flow-mediated dilation before, during, and after preeclampsia: a systematic review and meta-analysis. Hypertension 67, 415–423 (2016).
Vikse, B. E., Hallan, S., Bostad, L., Leivestad, T. & Iversen, B. M. Previous preeclampsia and risk for progression of biopsy-verified kidney disease to end-stage renal disease. Nephrol. Dial. Transpl. 25, 3289–3296 (2010).
Oliverio, A. L. et al. Renal complications in pregnancy preceding glomerulonephropathy diagnosis. Kidney Int. Rep. 4, 159–162 (2019).
Cabiddu, G. et al. History of preeclampsia in patients undergoing a kidney biopsy: a biphasic, multiple-hit pathogenic hypothesis. Kidney Int. Rep. 7, 547–557 (2022).
Conti-Ramsden, F. I. et al. Pregnancy-related acute kidney injury in preeclampsia: risk factors and renal outcomes. Hypertension 74, 1144–1151 (2019).
Gaber, L. W., Spargo, B. H. & Lindheimer, M. D. Renal pathology in pre-eclampsia. Baillieres Clin. Obstet. Gynaecol. 8, 443–468 (1994).
Kincaid-Smith, P. The renal lesion of preeclampsia revisited. Am. J. Kidney Dis. 17, 144–148 (1991).
Stillman, I. E. & Karumanchi, S. A. The glomerular injury of preeclampsia. J. Am. Soc. Nephrol. 18, 2281–2284 (2007).
Meibody, F. et al. Post-partum acute kidney injury: sorting placental and non-placental thrombotic microangiopathies using the trajectory of biomarkers. Nephrol. Dial. Transpl. 35, 1538–1546 (2020).
Villie, P. et al. Why kidneys fail post-partum: a tubulocentric viewpoint. J. Nephrol. 31, 645–651 (2018).
Rodriguez-Benitez, P. et al. Maternal-perinatal variables in patients with severe preeclampsia who develop acute kidney injury. J. Clin. Med. 10, 5629 (2021).
Sahay, M., Dogra, L., Ismal, K. & Vali, S. Pregnancy-related acute kidney injury in public hospital in South India: changing trends. J. Assoc. Physicians India 70, 11–12 (2022).
Trakarnvanich, T., Ngamvichchukorn, T. & Susantitaphong, P. Incidence of acute kidney injury during pregnancy and its prognostic value for adverse clinical outcomes: a systematic review and meta-analysis. Medicine 101, e29563 (2022).
Shalaby, A. S. & Shemies, R. S. Pregnancy-related acute kidney injury in the African continent: where do we stand? A systematic review. J. Nephrol. 35, 2175–2189 (2022).
Karimi, Z., Malekmakan, L. & Farshadi, M. The prevalence of pregnancy-related acute renal failure in Asia: a systematic review. Saudi J. Kidney Dis. Transpl. 28, 1–8 (2017).
Prakash, J. et al. Acute renal failure in pregnancy in a developing country: twenty years of experience. Ren. Fail. 28, 309–313 (2006).
Berhe, E. et al. Characteristics and outcome of pregnancy-related acute kidney injury in a teaching hospital in a low-resource setting: a five-year retrospective review. BMC Nephrol. 25, 182 (2024).
Shah, S. et al. Pregnancy-related acute kidney injury in the United States: clinical outcomes and health care utilization. Am. J. Nephrol. 51, 216–226 (2020).
Meazaw, M. W., Chojenta, C., Muluneh, M. D. & Loxton, D. Systematic and meta-analysis of factors associated with preeclampsia and eclampsia in sub-Saharan Africa. PLoS ONE 15, e0237600 (2020).
Filali Khattabi, Z. et al. Chronic kidney disease in preeclamptic patients: not found unless searched for-is a nephrology evaluation useful after an episode of preeclampsia? J. Nephrol. 32, 977–987 (2019).
Ibarra-Hernandez, M. et al. Challenges in managing pregnancy in underserved women with chronic kidney disease. Am. J. Nephrol. 49, 386–396 (2019).
Hall, D. R. & Conti-Ramsden, F. Acute kidney injury in pregnancy including renal disease diagnosed in pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 57, 47–59 (2019).
Facca, T. A. et al. Pregnancy as an early stress test for cardiovascular and kidney disease diagnosis. Pregnancy Hypertens. 12, 169–173 (2018).
Kaul, A. et al. Pregnancy check point for diagnosis of CKD in developing countries. J. Obstet. Gynaecol. India 68, 440–446 (2018).
Rivera, J. C. H. et al. Delayed initiation of hemodialysis in pregnant women with chronic kidney disease: logistical problems impact clinical outcomes. an experience from an emerging country. J. Clin. Med. 8, 475 (2019).
National Institute for Health Care and Excellence. Hypertension in Pregnancy: Follow-up Care and Postnatal Review (NICE, 2023).
National Institute for Health Care and Excellence. Hypertension in Pregnancy: Diagnosis and Management (NICE, 2023).
Smart, N. A., Dieberg, G., Ladhani, M. & Titus, T. Early referral to specialist nephrology services for preventing the progression to end-stage kidney disease. Cochrane Database Syst. Rev. 18, CD007333 (2014).
Huisman, R. M. The deadly risk of late referral. Nephrol. Dial. Transpl. 19, 2175–2180 (2004).
Al Khalaf, S. et al. Chronic kidney disease and adverse pregnancy outcomes: a systematic review and meta-analysis. Am. J. Obstet. Gynecol. 226, 656–670.e32 (2022).
Jeyaraman, D. et al. Adverse pregnancy outcomes in pregnant women with chronic kidney disease: a systematic review and meta-analysis. BJOG 131, 1331–1340 (2024).
Marek-Iannucci, S. et al. Association of chronic kidney dysfunction and preeclampsia: insights of the nationwide inpatient sample. Am. J. Obstet. Gynecol. MFM 5, 100928 (2023).
Piccoli, G. B. et al. Any reduction in maternal kidney mass makes a difference during pregnancy in gestational and fetal outcome. Kidney Int. 105, 865–876 (2024).
Piccoli, G. B. et al. Risk of adverse pregnancy outcomes in women with CKD. J. Am. Soc. Nephrol. 26, 2011–2022 (2015).
Tangren, J. S. et al. Metabolic and hypertensive complications of pregnancy in women with nephrolithiasis. Clin. J. Am. Soc. Nephrol. 13, 612–619 (2018).
Tangren, J. S. et al. Pregnancy outcomes after clinical recovery from AKI. J. Am. Soc. Nephrol. 28, 1566–1574 (2017).
Tangren, J. S. et al. Risk of preeclampsia and pregnancy complications in women with a history of acute kidney injury. Hypertension 72, 451–459 (2018).
Pippias, M. et al. Pregnancy after living kidney donation, a systematic review of the available evidence, and a review of the current guidance. Am. J. Transpl. 22, 2360–2380 (2022).
He, Y. et al. Pregnancy in patients with stage 3–5 CKD: maternal and fetal outcomes. Pregnancy Hypertens. 29, 86–91 (2022).
Wiles, K. et al. The impact of chronic kidney disease Stages 3–5 on pregnancy outcomes. Nephrol. Dial. Transpl. 36, 2008–2017 (2021).
Imbasciati, E. et al. Pregnancy in CKD stages 3 to 5: fetal and maternal outcomes. Am. J. Kidney Dis. 49, 753–762 (2007).
Piccoli, G. B. What is superimposed preeclampsia (and does it actually exist)? Kidney Int. Rep. 4, 759–762 (2019).
Wiles, K. et al. Placental and endothelial biomarkers for the prediction of superimposed pre-eclampsia in chronic kidney disease. Pregnancy Hypertens. 24, 58–64 (2021).
Bramham, K. et al. Predisposition to superimposed preeclampsia in women with chronic hypertension: endothelial, renal, cardiac, and placental factors in a prospective longitudinal cohort. Hypertens. Pregnancy 39, 326–335 (2020).
Akbari, A. et al. Circulating angiogenic factors in a pregnant woman on intensive hemodialysis: a case report. Can. J. Kidney Health Dis. 3, 7 (2016).
Shanmugalingam, R., Cole-Clark, A., Lowrie, E., Hennessy, A. & Makris, A. Clinical use of angiogenic factors in managing a pregnant woman on hemodialysis to term. Kidney Int. Rep. 6, 1449–1453 (2021).
Morisawa, H. et al. Difficulty of predicting early-onset super-imposed preeclampsia in pregnant women with hemodialysis due to diabetic nephropathy by serum levels of sFlt-1, PlGF, and sEng. CEN Case Rep. 9, 101–105 (2020).
Gosselink, M. E. et al. A nationwide Dutch cohort study shows relatively good pregnancy outcomes after kidney transplantation and finds risk factors for adverse outcomes. Kidney Int. 102, 866–875 (2022).
Hewawasam, E. et al. Determinants of perinatal outcomes in dialyzed and transplanted women in Australia. Kidney Int. Rep. 7, 1318–1331 (2022).
Shah, S. et al. Pregnancy outcomes in women with kidney transplant: metaanalysis and systematic review. BMC Nephrol. 20, 24 (2019).
Lu, J. et al. Preeclampsia after kidney transplantation: rates and association with graft survival and function. Clin. J. Am. Soc. Nephrol. 18, 920–929 (2023).
Dines, V., D’Costa, M., Fidler, M. & Kattah, A. The role of kidney biopsy in diagnosis of preeclampsia in kidney transplant patients. Hypertens. Pregnancy 39, 418–422 (2020).
Majak, G. B. et al. Preeclampsia in kidney transplanted women; outcomes and a simple prognostic risk score system. PLoS ONE 12, e0173420 (2017).
Vannevel, V. et al. Preeclampsia and long-term renal function in women who underwent kidney transplantation. Obstet. Gynecol. 131, 57–62 (2018).
Park, S. et al. Pregnancy in women with immunoglobulin A nephropathy: are obstetrical complications associated with renal prognosis? Nephrol. Dial. Transpl. 33, 459–465 (2018).
Luyckx, V. A. & Brenner, B. M. Clinical consequences of developmental programming of low nephron number. Anat. Rec. 303, 2613–2631 (2020).
Li, F. et al. Adverse pregnancy outcomes among mothers with hypertensive disorders in pregnancy: a meta-analysis of cohort studies. Pregnancy Hypertens. 24, 107–117 (2021).
Wu, C. S. et al. Health of children born to mothers who had preeclampsia: a population-based cohort study. Am. J. Obstet. Gynecol. 201, 269.e1–269.e10 (2009).
Koulouraki, S. et al. Short- and long-term outcomes of preeclampsia in offspring: review of the literature. Children 10, 826 (2023).
Turbeville, H. R. & Sasser, J. M. Preeclampsia beyond pregnancy: long-term consequences for mother and child. Am. J. Physiol. Renal Physiol. 318, F1315–F1326 (2020).
Ratsep, M. T. et al. Impact of preeclampsia on cognitive function in the offspring. Behav. Brain Res. 302, 175–181 (2016).
Kokori, E. et al. Maternal and fetal neurocognitive outcomes in preeclampsia and eclampsia; a narrative review of current evidence. Eur. J. Med. Res. 29, 470 (2024).
Bokslag, A., van Weissenbruch, M., Mol, B. W. & de Groot, C. J. Preeclampsia; short and long-term consequences for mother and neonate. Early Hum. Dev. 102, 47–50 (2016).
Chappell, L. C. et al. Planned early delivery or expectant management for late preterm pre-eclampsia (PHOENIX): a randomised controlled trial. Lancet 394, 1181–1190 (2019).
Wang, Y. et al. Aspirin for the prevention of preeclampsia: a systematic review and meta-analysis of randomized controlled studies. Front. Cardiovasc. Med. 9, 936560 (2022).
Roberge, S. et al. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am. J. Obstet. Gynecol. 216, 110–120 e116 (2017).
North, R. A., Ferrier, C., Gamble, G., Fairley, K. F. & Kincaid-Smith, P. Prevention of preeclampsia with heparin and antiplatelet drugs in women with renal disease. Aust. N. Z. J. Obstet. Gynaecol. 35, 357–362 (1995).
de Vries, J. I. et al. Low-molecular-weight heparin added to aspirin in the prevention of recurrent early-onset pre-eclampsia in women with inheritable thrombophilia: the FRUIT-RCT. J. Thromb. Haemost. 10, 64–72 (2012).
van Hoorn, M. E. et al. Low-molecular-weight heparin and aspirin in the prevention of recurrent early-onset pre-eclampsia in women with antiphospholipid antibodies: the FRUIT-RCT. Eur. J. Obstet. Gynecol. Reprod. Biol. 197, 168–173 (2016).
Martinelli, I. et al. Heparin in pregnant women with previous placenta-mediated pregnancy complications: a prospective, randomized, multicenter, controlled clinical trial. Blood 119, 3269–3275 (2012).
Haddad, B. et al. Enoxaparin and aspirin compared with aspirin alone to prevent placenta-mediated pregnancy complications: a randomized controlled trial. Obstet. Gynecol. 128, 1053–1063 (2016).
Wang, X. & Gao, H. Prevention of preeclampsia in high-risk patients with low-molecular-weight heparin: a meta-analysis. J. Matern. Fetal Neonatal Med. 33, 2202–2208 (2020).
McLaughlin, K., Scholten, R. R., Parker, J. D., Ferrazzi, E. & Kingdom, J. C. P. Low molecular weight heparin for the prevention of severe preeclampsia: where next? Br. J. Clin. Pharmacol. 84, 673–678 (2018).
Cruz-Lemini, M., Vazquez, J. C., Ullmo, J. & Llurba, E. Low-molecular-weight heparin for prevention of preeclampsia and other placenta-mediated complications: a systematic review and meta-analysis. Am. J. Obstet. Gynecol. 226, S1126–S1144.e17 (2022).
Dwarkanath, P. et al. Two randomized trials of low-dose calcium supplementation in pregnancy. N. Engl. J. Med. 390, 143–153 (2024).
Woo Kinshella, M. L. et al. Calcium for pre-eclampsia prevention: a systematic review and network meta-analysis to guide personalised antenatal care. BJOG 129, 1833–1843 (2022).
Evenepoel, P. et al. Recommended calcium intake in adults and children with chronic kidney disease — a European consensus statement. Nephrol. Dial. Transpl. 39, 341–366 (2024).
Aguilar, A. et al. Pathophysiology of bone disease in chronic kidney disease: from basics to renal osteodystrophy and osteoporosis. Front. Physiol. 14, 1177829 (2023).
World Health Organisation. WHO Recommendation: Calcium Supplementation during Pregnancy for the Prevention of Pre-eclampsia and its Complications (WHO, 2018).
Hofmeyr, G. J., Lawrie, T. A., Atallah, A. N. & Torloni, M. R. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst. Rev. 10, CD001059 (2018).
Bhowmik, B. et al. Maternal BMI and nutritional status in early pregnancy and its impact on neonatal outcomes at birth in Bangladesh. BMC Pregnancy Childbirth 19, 413 (2019).
World Health organization. WHO Antenatal Care Recommendations for a Positive Pregnancy Experience — Nutritional Interventions Update: Vitamin D Supplements during Pregnancy (WHO, 2020).
Palacios, C., Kostiuk, L. L., Cuthbert, A. & Weeks, J. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 7, CD008873 (2024).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 1911–1930 (2011).
Vadillo-Ortega, F. et al. Effect of supplementation during pregnancy with L-arginine and antioxidant vitamins in medical food on pre-eclampsia in high risk population: randomised controlled trial. BMJ 342, d2901 (2011).
Taliento, C. et al. Effect of physical activity during pregnancy on the risk of hypertension disorders and gestational diabetes: evidence generated by new RCTs and systematic reviews. J. Clin. Med. 13, 2198 (2024).
European Commission. Dietary recommendations for protein intake for pregnant and lactating women. EC https://knowledge4policy.ec.europa.eu/health-promotion-knowledge-gateway/dietary-protein-dietary-intake-pregnant-4_en (2021).
Ikizler, T. A. et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am. J. Kidney Dis. 76, S1–S107 (2020).
Institute of Medicine of the National Academies. Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids (National Academies, 2005).
Perry, A., Stephanou, A. & Rayman, M. P. Dietary factors that affect the risk of pre-eclampsia. BMJ Nutr. Prev. Health 5, 118–133 (2022).
Raghavan, R. et al. Dietary patterns before and during pregnancy and birth outcomes: a systematic review. Am. J. Clin. Nutr. 109, 729S–756S (2019).
Brantsaeter, A. L. et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J. Nutr. 139, 1162–1168 (2009).
Hall, K. D. et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 30, 226 (2019).
Attini, R. et al. Plant-based diets improve maternal-fetal outcomes in CKD pregnancies. Nutrients 14, 4203 (2022).
Piccoli, G. B. et al. Vegetarian supplemented low-protein diets. A safe option for pregnant CKD patients: report of 12 pregnancies in 11 patients. Nephrol. Dial. Transpl. 26, 196–205 (2011).
Piccoli, G. B. et al. Association of low-protein supplemented diets with fetal growth in pregnant women with CKD. Clin. J. Am. Soc. Nephrol. 9, 864–873 (2014).
Vilar-Compte, M. et al. Urban poverty and nutrition challenges associated with accessibility to a healthy diet: a global systematic literature review. Int. J. Equity Health 20, 40 (2021).
Syngelaki, A. et al. Metformin versus placebo in obese pregnant women without diabetes mellitus. N. Engl. J. Med. 374, 434–443 (2016).
Alqudah, A. et al. Risk of pre-eclampsia in women taking metformin: a systematic review and meta-analysis. Diabet. Med. 35, 160–172 (2018).
Costantine, M. M. et al. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am. J. Obstet. Gynecol. 214, 720.e1–720.e17 (2016).
Costantine, M. M. et al. A randomized pilot clinical trial of pravastatin versus placebo in pregnant patients at high risk of preeclampsia. Am. J. Obstet. Gynecol. 225, 666.e1–666.e15 (2021).
Akbar, M. I. A. et al. INOVASIA study: a multicenter randomized clinical trial of pravastatin to prevent preeclampsia in high-risk patients. Am. J. Perinatol. 41, 1203–1211 (2024).
Ahmed, A. et al. Pravastatin for early-onset pre-eclampsia: a randomised, blinded, placebo-controlled trial. BJOG 127, 478–488 (2020).
Rozas-Villanueva, M. F., Casanello, P. & Retamal, M. A. Role of ROS/RNS in preeclampsia: are connexins the missing piece? Int. J. Mol. Sci. 21, 4698 (2020).
Brownfoot, F. C. et al. Effects of simvastatin, rosuvastatin and pravastatin on soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sENG) secretion from human umbilical vein endothelial cells, primary trophoblast cells and placenta. BMC Pregnancy Childbirth 16, 117 (2016).
Meijerink, L. et al. Statins in pre-eclampsia or fetal growth restriction: a systematic review and meta-analysis on maternal blood pressure and fetal growth across species. BJOG 130, 577–585 (2023).
Kattah, A. et al. Complement C5 inhibition as a novel therapeutic approach in severe pre-eclampsia. Mayo Clin. Proc. 97, 1580–1583 (2022).
Thadhani, R. et al. Pilot study of extracorporeal removal of soluble fms-like tyrosine kinase 1 in preeclampsia. Circulation 124, 940–950 (2011).
Gilbert, J. S. et al. Recombinant vascular endothelial growth factor 121 infusion lowers blood pressure and improves renal function in rats with placental ischemia-induced hypertension. Hypertension 55, 380–385 (2010).
Hamano, T. Women with a history of preeclampsia should be monitored for the onset and progression of chronic kidney disease. Nat. Clin. Pract. Nephrol. 5, 8–9 (2009).
Piccoli, G. B. et al. The ABCs of post-preeclampsia outpatient nephrology care: the Le Mans strategy. J. Nephrol. 37, 2481–2489 (2024).
Inversetti, A. et al. Update on long-term cardiovascular risk after pre-eclampsia: a systematic review and meta-analysis. Eur. Heart J. Qual. Care Clin. Outcomes 10, 4–13 (2024).
Staff, A. C., Costa, M. L., Dechend, R., Jacobsen, D. P. & Sugulle, M. Hypertensive disorders of pregnancy and long-term maternal cardiovascular risk: bridging epidemiological knowledge into personalized postpartum care and follow-up. Pregnancy Hypertens. 36, 101127 (2024).
Daubert, M. A. et al. Early postpartum blood pressure screening is associated with increased detection of cardiovascular risk factors in women with hypertensive disorders of pregnancy. Am. Heart J. 273, 130–139 (2024).
Ackerman-Banks, C. M. et al. Seizing the window of opportunity within 1 year postpartum: early cardiovascular screening. J. Am. Heart Assoc. 11, e024443 (2022).
Conti-Ramsden, F., Bramham, K. & de Marvao, A. Long-term cardiovascular disease after pre-eclampsia: time to move from epidemiology to action. Eur. Heart J. Qual. Care Clin. Outcomes 10, 1–3 (2024).
Wu, P. et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 10, e003497 (2017).
Lo, C. C. W. et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta-analysis. J. Am. Heart Assoc. 9, e013991 (2020).
Tannor, E. K., Nlandu, Y. M., Elrggal, M. E., Chika, O. U. & Nzana, V. Kidney health for all — bridging the gap to better kidney care in Africa. Afr. J. Nephrol. 25, 108–115 (2022).
Talle, M. A. et al. Status of cardiac arrhythmia services in Africa in 2018: a PASCAR sudden cardiac death task force report. Cardiovasc. J. Afr. 29, 115–121 (2018).
Gonçalves, M. A. A., Morais, H., Oliveira, G. M. M. D. & Mesquita, C. T. Challenges and perspectives for cardiology in the developing world: joint views from Africa and Latin America. Int. J. Cardiovasc. Sci. 37, e20240002 (2024).
Anumudu, S. J. & Fadem, S. Z. in Nephrology Worldwide (eds Moura-Neto, J. A., Divino-Filho, J. C. & Ronco, C.) 173–186 (Springer, 2021).
Bellasi, A. et al. in Nephrology Worldwide (eds Moura-Neto, J. A., Divino-Filho, J. C. & Ronco, C.) 557–568 (Springer, 2021).
European Society of Cardiology. Cardiologists (total) (per million people). ESC https://eatlas.escardio.org/Data/Cardiovascular-healthcare-delivery/Cardiological-specialists/chr_card_1m_r-cardiologists-total-per-million-people (2024).
Canaud, B. & Choukroun, G. in Nephrology Worldwide (eds Moura-Neto, J. A., Divino-Filho, J. C. & Ronco, C.) 521–541 (Springer, 2021).
European Society of Cardiology. French Society of Cardiology. ESC https://www.escardio.org/The-ESC/Member-National-Cardiac-Societies/French-Society-of-Cardiology (2024).
Schulz, C. et al. Characteristics of outpatients referred for a first consultation with a nephrologist: impact of different guidelines. J. Nephrol. 35, 1375–1385 (2022).
Jesudason, S. Implementing referral systems for nephrology services: real world practice versus guidelines. J. Nephrol. 35, 1369–1370 (2022).
Li, K. et al. Use of kidney failure risk equation as a tool to evaluate referrals from primary care to specialist nephrology care. Intern. Med. J. 54, 1126–1135 (2024).
Francis, A. et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat. Rev. Nephrol. 20, 473–485 (2024).
Carrero, J. J., Hecking, M., Chesnaye, N. C. & Jager, K. J. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat. Rev. Nephrol. 14, 151–164 (2018).
Li, L. et al. Trophoblast-targeted nanomedicine modulates placental sFLT1 for preeclampsia treatment. Front. Bioeng. Biotechnol. 8, 64 (2020).
Turanov, A. A. et al. RNAi modulation of placental sFLT1 for the treatment of preeclampsia. Nat. Biotechnol. 36, 1164–1173 (2018).
PRNewswire. Comanche Biopharma receives US FDA fast track designation for CBP-4888 for the treatment of sFlt-1 mediated pre-term preeclampsia. PRNewswire https://www.prnewswire.com/news-releases/comanche-biopharma-drug-receives-fda-fast-track-designation-301908285.html (2023).
Wang, Y. et al. Heparin-mediated extracorporeal low density lipoprotein precipitation as a possible therapeutic approach in preeclampsia. Transfus. Apher. Sci. 35, 103–110 (2006).
Winkler, K. et al. Treatment of very preterm preeclampsia via heparin-mediated extracorporeal LDL-precipitation (H.E.L.P.) apheresis: the Freiburg preeclampsia H.E.L.P.-apheresis study. Pregnancy Hypertens. 12, 136–143 (2018).
Nakakita, B. et al. Case of soluble fms-like tyrosine kinase 1 apheresis in severe pre-eclampsia developed at 15 weeks’ gestation. J. Obstet. Gynaecol. Res. 41, 1661–1663 (2015).
Gubensek, J. et al. Treatment of preeclampsia at extremely preterm gestation with therapeutic plasma exchange. Clin. Nephrol. 96, 101–106 (2021).
Thadhani, R. et al. Removal of soluble Fms-like tyrosine kinase-1 by dextran sulfate apheresis in preeclampsia. J. Am. Soc. Nephrol. 27, 903–913 (2016).
Haddad, B. et al. LDL-apheresis to decrease sFlt-1 during early severe preeclampsia: report of two cases from a discontinued phase II trial. Eur. J. Obstet. Gynecol. Reprod. Biol. 231, 70–74 (2018).
Logue, O. C., Mahdi, F., Chapman, H., George, E. M. & Bidwell, G. L. 3rd A maternally sequestered, biopolymer-stabilized vascular endothelial growth factor (VEGF) chimera for treatment of preeclampsia. J. Am. Heart Assoc. 6, e007216 (2017).
Waller, J. P., Howell, J. A., Peterson, H., George, E. M. & Bidwell, G. L. 3rd Elastin-like polypeptide: VEGF-B fusion protein for treatment of preeclampsia. Hypertension 78, 1888–1901 (2021).
Engel, J. E. et al. Recovery of renal function following kidney-specific VEGF therapy in experimental renovascular disease. Am. J. Nephrol. 51, 891–902 (2020).
Kadife, E. et al. Hydroxychloroquine reduces soluble Flt-1 secretion from human cytotrophoblast, but does not mitigate markers of endothelial dysfunction in vitro. PLoS ONE 17, e0271560 (2022).
de Moreuil, C., Alavi, Z. & Pasquier, E. Hydroxychloroquine may be beneficial in preeclampsia and recurrent miscarriage. Br. J. Clin. Pharmacol. 86, 39–49 (2020).
Pierik, E. et al. Dysregulation of complement activation and placental dysfunction: a potential target to treat preeclampsia? Front. Immunol. 10, 3098 (2019).
Morales, E. et al. Eculizumab in early-stage pregnancy. Kidney Int. Rep. 5, 2383–2387 (2020).
Neri, I., Jasonni, V. M., Gori, G. F., Blasi, I. & Facchinetti, F. Effect of L-arginine on blood pressure in pregnancy-induced hypertension: a randomized placebo-controlled trial. J. Matern. Fetal Neonatal Med. 19, 277–281 (2006).
Winer, N. et al. Oral citrulline supplementation in pregnancies with preeclampsia: a multicenter, randomized, double-blind clinical trial. Am. J. Clin. Nutr. 121, 488–496 (2025).
Saleh, L. et al. Low soluble Fms-like tyrosine kinase-1, endoglin, and endothelin-1 levels in women with confirmed or suspected preeclampsia using proton pump inhibitors. Hypertension 70, 594–600 (2017).
Cluver, C. A. et al. Esomeprazole to treat women with preterm preeclampsia: a randomized placebo controlled trial. Am. J. Obstet. Gynecol. 219, 388.e1–388.e17 (2018).
Kobayashi, T. et al. Treatment of severe preeclampsia with antithrombin concentrate: results of a prospective feasibility study. Semin. Thromb. Hemost. 29, 645–652 (2003).
Maki, M. et al. Antithrombin therapy for severe preeclampsia: results of a double-blind, randomized, placebo-controlled trial. BI51.017 study group. Thromb. Haemost. 84, 583–590 (2000).
Paidas, M. J. et al. Prospective, randomized, double-blind, placebo-controlled evaluation of the pharmacokinetics, safety and efficacy of recombinant antithrombin versus placebo in preterm preeclampsia. Am. J. Obstet. Gynecol. 223, 739.e1–739.e13 (2020).
Chen, J., Huai, J. & Yang, H. Low-molecular-weight heparin for the prevention of preeclampsia in high-risk pregnancies without thrombophilia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 24, 68 (2024).
Socha, M. W., Chmielewski, J., Pietrus, M. & Wartega, M. Endogenous digitalis-like factors as a key molecule in the pathophysiology of pregnancy-induced hypertension and a potential therapeutic target in preeclampsia. Int. J. Mol. Sci. 24, 12743 (2023).
GBD 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950-2021, with forecasts to 2100: a comprehensive demographic analysis for the Global burden of disease study 2021. Lancet 403, 2057–2099 (2024).
Brouwers, L. et al. Recurrence of pre-eclampsia and the risk of future hypertension and cardiovascular disease: a systematic review and meta-analysis. BJOG 125, 1642–1654 (2018).