Insurance rate requests increase by double digits
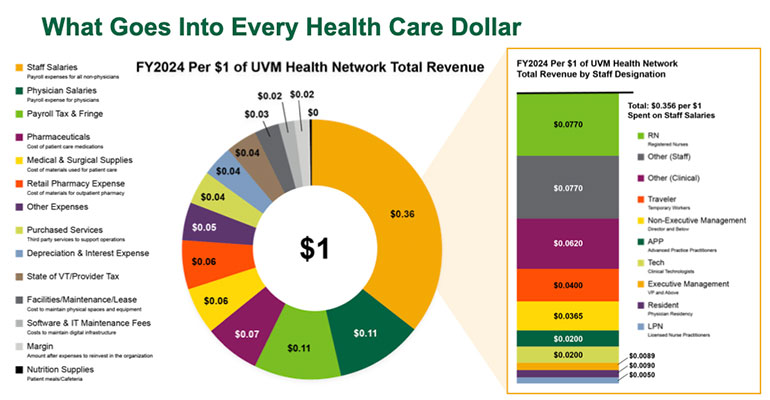
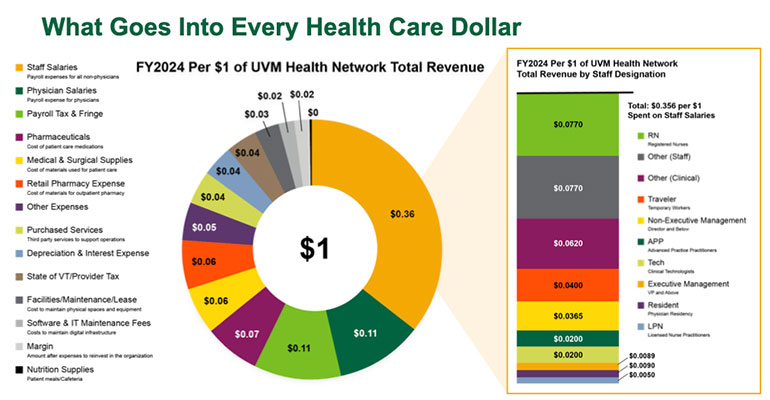
Photo: Graphic courtesy UVMHN
by Timothy McQuiston, Vermont Business Magazine
Blue Cross Vermont President and CEO Don George has once again expressed concern about the financial stability of his company and the health insurance industry. He also emphasized the financial vulnerability of the broader health care system, a view shared across the board.

Photo: Don George, president and CEO at Blue Cross and Blue Shield of Vermont. Courtesy photo.
While finding a financial solution remains challenging, various initiatives are underway. Gov. Phil Scott recognized the issue in May but indicated that his administration is currently prioritizing housing, education reform and overall economic affordability.
“We have other challenges we must address,“ Scott said.
The governor suggested that discussions about health care parallel those on education reform, predicting consolidation within the existing system. He clarified he wasn’t advocating for hospital closures but urged a reassessment of current practices, stating that it’s unrealistic for every hospital to offer all services.
“We can’t be everything to all people,“ Scott said. “We are not exactly growing in population. We’re not growing in the right areas. We need a younger, healthier population to backfill what people are paying into the system.“
He emphasized that resolving the issue would require collective efforts across all sectors, indicating there’s no single solution, but rather a matter of basic arithmetic.
“Having said that, I think we have to look at some of the bigger hospitals and find efficiencies of scale there in order to right this ship,“ he said.
Still, there are several health care bills making their way through the system or already signed into law by the governor. See below.
Last summer, the Green Mountain Care Board released the comprehensive Oliver Wyman report, which analyzed the state’s hospitals. The report confirmed the severe financial difficulties facing the hospital system, concluding that most hospitals would likely operate at a deficit within a few years.
Although the report did not explicitly suggest closing any hospitals, it cautioned that economic pressures might lead to the closure of smaller facilities, specifically mentioning Grace Cottage in Townshend, Gifford Medical Center in Randolph, Springfield Hospital and North Country Hospital in Newport.
The report advocated for strategic reorganization of Vermont’s hospital system, emphasizing specialization to decrease redundancies and expenses.
Hospitals have asserted they are actively fulfilling their communities’ health needs and warned that service reductions would negatively impact community health. They contend that the broader health care financial system is flawed, not just the hospitals themselves, a point widely acknowledged.
Unsustainable finances are impacting hospitals, clinics and doctors’ offices alike, despite Vermont’s high health care costs nationally. Insurance reimbursement rates are reportedly insufficient to cover expenses.
Insurers argue their member premiums are too low and are seeking rate increases. Hospitals believe the Green Mountain Care Board’s regulatory oversight limits their revenue generation capacity.
Businesses that finance substantial portions of premiums are struggling to keep up. Consequently, patients face rising insurance and out-of-pocket costs for treatment and medications, potentially encountering difficulties in securing timely access to providers.
Vermont is currently experiencing a shortage of health care providers. Efforts to attract doctors have been unsuccessful due to comparable or higher pay opportunities in other regions, where living expenses are often lower. Consequently, hospitals heavily depend on costly traveling nurses due to the lack of available in-state nurses.
Furthermore, Blue Cross Blue Shield of Vermont reported a loss exceeding $62 million in 2024, attributed to a health care expense increase of over 15% from the previous year. This follows previous losses of $24 million in 2023, $46 million in 2022 and $17 million in 2021.
According to Blue Cross VT, this marks the fourth consecutive year that patient claim expenses have surpassed premium income. The company provides coverage for more than 230,000 Vermonters.
BCBS is once again requesting significant rate increases for next year.
On May 12, the Green Mountain Care Board received the 2026 individual and small-group health insurance premium rate filings requests. Blue Cross and Blue Shield of Vermont is requesting a 23.3% increase in the individual market and a 13.7% increase in the small-group market. MVP Health Plan is requesting increases of 6.2% and 7.5%, respectively.
This marks the start of a multimonth public review process led by the GMCB, which includes input from actuaries, carriers, the Healthcare Advocate, the Department of Financial Regulation and the public. Final decisions are expected in August.
Proposed rates may change during this review, possibly due to federal-level changes. The individual market rates, for example, reflect increases due to the anticipated expiration of federal enhanced premium tax credits on Dec. 31, unless Congress acts. This expiration could lead to higher net premium increases for individuals.
The high cost of health care and drugs, and the variability of federal policy, affects more than just Vermont. However, there is consensus that these issues are particularly acute in Vermont.
“It is no secret that Vermont’s health care system is in crisis,“ U.S. Senator Bernie Sanders, I-Vt., said at a news conference in Burlington in May. “While Vermont is not alone in these struggles, the sad reality is that our state is struggling more than most.“

Photo: Senator Bernie Sanders held a press conference on May 19 at the Leahy Burlington International Airport to discuss the healthcare crisis. Speakers included State Sen. Virginia “Ginny” Lyons (far right), State Rep. Alyssa Black (left), and to her left Owen Foster, Chair of the Green Mountain Care Board. VermontBiz photo.
For decades, Sanders has proposed a “Medicare for All“ single-payer insurance plan in response to these ongoing challenges.
“Unfortunately, the federal government is not coming to fix this crisis,“ Sanders said. “Instead, President Trump and my Republican colleagues in Washington want to make things far worse by slashing Medicaid and tax credits that lower premiums for Vermonters.“
The president’s proposal would cut Medicaid and the Affordable Care Act by $715 billion, he added.
Vermonters’ access to health care is at risk due to “extraordinarily“ high hospital and drug prices, according to Sanders. He pointed out that Vermont has the second-oldest population in the US, leading to fewer people on commercial insurance.
Additionally, Vermont ranks 43rd nationally in nursing staff, primarily due to low pay and a significant health care worker shortage. Sanders emphasized that a Medicare for All plan would particularly benefit small-business owners by relieving them of the burden of providing employee health insurance coverage.
“I commend both the Vermont House and Senate for standing up to small but powerful parts of our health care industry and taking up legislation to address the challenges we face,“ Sanders said. “We must listen to the working families who can no longer afford their health care premium, the small-business owners who can no longer afford to provide health care coverage for their workers, and the nurses who are working in understaffed facilities for low wages. We simply cannot delay acting to address this crisis.“
The University of Vermont Health Network stated it shares Sanders’ priorities and is actively working to implement them. This work includes an $11 million investment in non-UVMHN primary care; a focus on getting more than 8,000 new patients into primary care at UVMHN practices this fiscal year; successfully decreasing reliance on travelers and recruiting and retaining nursing staff; and a robust workforce development program providing many new opportunities for our staff to advance in their careers or train the next generation of nurses.“
“As a safety net provider for patients with Medicaid, as well as patients with Medicare, patients struggling to afford commercial insurance, and those who are uninsured, UVM Health Network agrees that the status quo isn’t working for Vermonters,“ system officials said in a statement. “Change that makes health care work better for our patients, our people and communities will require tough decisions from all stakeholders.
“We recognize the urgency of this moment,“ the statement continued, “and are taking action, beginning with a series of cuts and commitments aimed at improving sustainability and affordability for Vermonters totaling $158 million so far, and we are committed to the fight to protect Medicaid for the hundreds of thousands of people in our region whose lives depend on it.“
The UVMHN system includes the UVM Medical Center in Burlington, Central Vermont Medical Center in Berlin and Porter Medical Center in Middlebury, as well as other provider offices and clinics, hospice care and three hospitals in upstate New York.
While the implementation of comprehensive health care reform like Medicare for All, or models similar to those in Europe, might not occur in the near future, Vermont leaders are actively addressing the current health care crisis. On May 15, Scott signed S.27 into law, a proposal by state Treasurer Mike Pieciak aimed at eliminating up to $100 million in medical debt for middle- and working-class Vermonters and removing medical debt from credit scores. This bill, passed unanimously by the Legislature, requires no new taxes or fees.
“I want to thank the governor and the Legislature for supporting this important investment in a healthier, more secure future for our state,“ Pieciak said.
Democratic state Sen. Ginny Lyons, chair of the Senate Committee on Health and Welfare, said the one-time program is a timely response to the growing cost of care in Vermont.
“As health care costs outpace what most Vermonters can afford, S.27 is a smart, one-time investment that will deliver immediate relief,“ Lyons said. “This bill offers a hand up to those who need it most, helping them move forward with their lives without medical debt holding them back.“
State Rep. Alyssa Black, chair of the House Committee on Health Care, said S.27 passed with unanimous support for a reason.
“We’re all one health emergency away from a lifetime of financial ruin,“ she said. “This bill is an important step in ensuring that when someone is sick or injured, their focus can remain on their health, not their finances.“
Medical debt, the leading cause of bankruptcy in the U.S., affects over 60,000 Vermonters. This debt is often unavoidable due to the lack of upfront cost transparency and the necessity of care.
Medical debt discourages individuals from seeking necessary care, resulting in poorer health outcomes, higher future health care costs and lost work time. A 2021 Vermont Department of Health survey revealed that 85,000 Vermonters delayed or avoided care due to concerns about medical debt.
Michael Del Trecco, president and CEO of the Vermont Association of Hospitals and Health Systems, emphasized that medical debt impacts not only patients but the entire Vermont health care system.
“Medical debt can deter Vermonters from getting the care they need, even after the debt is no longer being pursued by collectors,“ Del Trecco said. “This often leads to affordability issues for Vermonters and more expensive care across the delivery system. At a time when our health care system is under immense strain, S.27 helps break this harmful cycle — supporting better health outcomes and the long-term stability of care in our state.“
Although the governor signed the bill, he expressed reservations. He acknowledged the efforts of the state treasurer and legislators to provide medical debt relief but noted that much of the debt had already been written off by providers and factored into higher rates for ratepayers.
He also cautioned that the program could expand amid Vermont’s health care and affordability crises, raising concerns about future funding. Additionally, he worried that the program might discourage debt repayment due to a perception that the state would cover it.
“I very much appreciate the intent and immediate benefits of S.27 to Vermonters,“ Scott said. “But we will need to manage this program effectively and pair it with real reforms.“
Vermonters qualify for debt relief if their debts are in “terminal bad debt status“ or they meet one of the following financial conditions: their household income is at or below 400% of the federal poverty level ($60,240 for an individual, $124,800 for a family of four), or their medical debt equals or exceeds 5% of their household income.
The program uses a one-time $1 million investment from funds previously appropriated to the treasurer’s office to buy down outstanding state bonds. Using this funding source, S.27 will not increase fees or taxes for Vermonters.
States like Rhode Island have adopted similar initiatives, successfully eliminating medical debt for their most vulnerable residents.
Pieciak emphasized that, while S.27 is an important step toward addressing Vermont’s high health care costs, more work is needed to fix Vermont’s broken health care system.
“Vermonters already pay some of the highest health care costs in the country, and year after year, they’re asked to pay more — even as access to care becomes less certain,“ Pieciak said. “To ensure Vermonters can access the care they need — when they need it — without going bankrupt, we must invest in bold, long-term solutions that make our health care system more affordable, accessible and high quality for all.“
Other Legislative Bills
The Legislature has been working on other measures as well. Given that there has been little opposition from the administration, it appears these will be signed into law.
340B Protection Bill: While H.266 maintains its 340B protections, the bill has also evolved to address the Blue Cross Blue Shield of Vermont financial crisis. BCBSVT cited Vermont’s high drug prices and its prohibition on white bagging (where patient medication is dispensed by a specialty pharmacy and shipped to the health care provider for administration) as key factors. Following testimony on white bagging’s quality and safety issues, the House Committee on Health Care proposed maintaining the prohibition but capping outpatient infusion therapies at 120% of the average sales price. BCBSVT estimates this will yield approximately $46 million. The bill language released last month exempts critical access hospitals. Capping drug prices will substantially impact other hospitals, and the committee was scheduled to hear further testimony. Section 340B of the Public Health Services Act requires Medicaid-participating pharmaceutical manufacturers to sell outpatient drugs at discounted prices to health care organizations serving a higher proportion of uninsured and low-income patients.
Health Care Reform Bill: The House passed S.126 last month, which allocates resources for the Agency of Human Services for transformation planning and creates three positions for the Green Mountain Care Board to implement reference-based pricing in 2027. The bill is now with the Senate.
Green Mountain Care Board Expansion of Powers: The Senate approved H.482, granting the Green Mountain Care Board expanded authority. This includes adjusting rates for specific hospitals in the event of Blue Cross Blue Shield of Vermont’s near insolvency and modifying hospital reimbursements for budget target deviations during the year. The bill also empowers the Green Mountain Care Board to appoint an independent monitor, funded by the hospital, if a hospital provides materially misrepresented information or demonstrates material noncompliance with its budget. Governor Scott signed into law June 5, 2025.
Don George Retiring
Health care transformation, whatever form it may take, will not go forward with Don George. The long-serving Blue Cross Vermont CEO announced in February that he would be stepping down at the end of this year.
He also sent letters to legislators underscoring the need for substantial action.
“In January, I shared the significant financial challenges facing Blue Cross and Blue Shield of Vermont and the related, larger issues undermining the sustainability of Vermont’s health care system. I outlined how the ongoing and unrelenting multiyear cost surge — driven by escalating prices for hospital services and extraordinary markups in prescription medications — depletes our member reserves, driving up premiums for our members and impeding affordability. I also asked you to join us in advocating for cost constraints and systemwide reform that’s long overdue.“
“We want to express our appreciation to our regulators, legislators, government and health care partners across the state for their willingness to advance difficult but meaningful changes for our health system. We are encouraged by discussions among leaders across our state and confident in our collective conviction to lower costs and fight for affordability for all Vermonters.“
Since January, Blue Cross VT has continued to stabilize its organization through immediate and long-term actions, George said.
These include:
Establishing in coordination with the Vermont Department of Financial Regulation a comprehensive capital recovery plan to ensure BCBSVT’s long-term stability.
Expanding the value of BCBSVT’s Blue Cross Blue Shield of Michigan affiliation, a key enabler of the organization’s mission to make health care work better for all Vermonters.
Reducing financial risk in Vermont Blue Advantage, BCBSVT’s Medicare Advantage plan.
Limiting BCBSVT’s already-lean administrative expenses.
Actively supporting legislation to protect BCBSVT members and safeguard its position within the insured marketplace.
Continuing to offer the highest quality health plans and customer service to BCBSVT members.
Proposing and supporting broader systemic changes in BCBSVT’s health care system. Company data shows that BCBSVT must constrain the prices of health care services and prescribed medications. As a result, Blue Cross VT urged the Green Mountain Care Board to implement hospital/payer-specific revenue caps — an important step toward affordability.
Agreement Between the GMCB and UVMHN
The recent settlement between the UVM Health Network and the Green Mountain Care Board offered compromise and a chance to reset. However, the agreement does not change the trajectory of healthcare spending.
The $12 million promised to Blue Cross VT to resolve 2022 and 2023 overcharges is an important step, however, these funds are not nearly enough to offset BCBSVT’s $62.1 million loss in 2024 or the cumulative millions over the past three years. More deliberate, long-term actions are required to limit pricing, curb unnecessary utilization, and ensure long-term stability of our organization and our health system.
Prioritizing Vermonters
“Vermont’s healthcare affordability crisis is far from over, and the escalating urgency and shared responsibility of cost containment remains. None of us can do it alone,” George said.
“Together, we face a long road ahead – one that demands systemic transformation. We must be honest about the magnitude of our problems and the pressures they place on families, our health system, and our economy. We also must take responsibility for our individual roles in our state’s healthcare affordability crisis, as well as our obligation to address that issue, and to do so now. Vermonters and Vermont employers and organizations urgently need relief. Only through difficult decisions, meaningful change, and the unwavering commitment of all Vermont healthcare leaders can we ensure a future of reliable and affordable care for Vermonters.”