A total of 29 participants (21 women, 8 men) were included in the study, with a mean age of 45 ± 10.6 SD years (ranging from 28 to 63). Of these, five were physicians, while the remainder comprised individuals with the potential to seek healthcare services.
Characteristics of participants with the potential to seek health services
It was determined that six participants had not previously received preventive healthcare services related to the prevention of NCDs in primary healthcare institutions. This was assessed through questions regarding their use of primary care services within the past year, as well as their responses to specific items on preventive care utilization (e.g., having undergone cancer screening, or receiving services from a dietitian or mental health professional), However, as they had the potential to seek healthcare services, they were generally categorized as ‘individuals with the potential to seek healthcare services”. To ensure diversity in the sample, participants were purposefully selected based on whether they had utilized preventive services, received care from family physicians, or had not accessed such services at all. Therefore, although all individuals technically have the potential to seek healthcare, in this study, the term “individuals with the potential to seek healthcare services” refers specifically to those who met the inclusion criteria based on their varying degrees of engagement with primary care preventive services.
The individual characteristics of participants with the potential to seek healthcare services are presented in Table 1. The average number of annual visits to healthcare institutions reported by these participants was 3.1. Only one participant reported not having health insurance, while four participants had both public and private health insurance. All participants indicated that they had lived in Istanbul for the longest duration of their lives.
The characteristics of healthcare providers
The individual characteristics of the family physicians are presented in Table 2.
Themes and subthemes
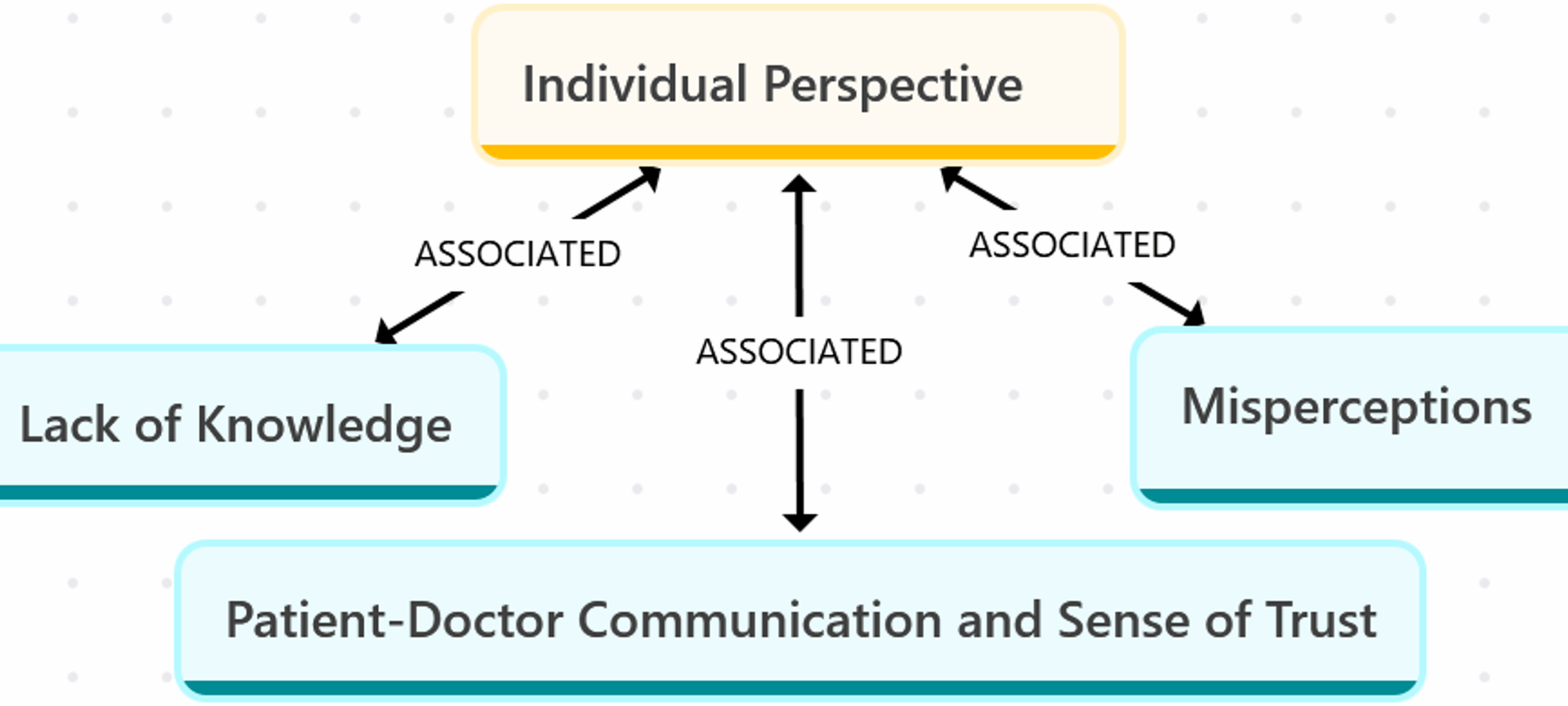
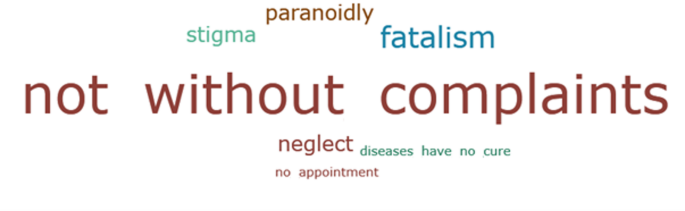
In the final analysis, two themes and six sub-themes were identified (Table 3). In the study, two main themes were identified: Barriers faced by community members and preventive healthcare from the physician’s perspective, along with six sub-themes (Fig. 1) (Fig. 2) (Table 3).
Lack of knowledge
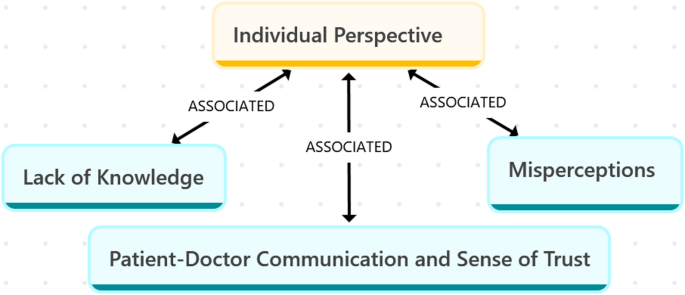
The participants thought that they could not access preventive health services without any justification (Fig. 3).
“…If I’m not in pain, why would I see a doctor? Won’t they ask, ‘What brings you here if nothing’s wrong?’ or think I’m joking? I mean, you’re a doctor… If I come to you and you ask, ‘Do you have any pain?’ and I say, ‘No,’ what am I supposed to say next? This question seems a bit strange to me…” (P20, 49 y, M).
Individuals mostly believed that they were at risk of illness if there was a history of chronic disease in the family, and they would request medical examination.
“…I don’t like going to the doctor very often, but since there’s this issue of cancer in the family, I get my tests done yearly. About 7 months ago, I had an endoscopy and colonoscopy, and I also had an ultrasound, mammogram, and breast ultrasound. So, I go for check-ups occasionally…” (P15, 63 y, F).
Overall, there was a strong belief in the importance of health check-ups for managing diseases. Individuals with cancer diagnoses in their immediate surroundings especially highlighted the significance of early detection in preventing illnesses.
“…to prevent it from turning into more serious illnesses, it’s also important to know what it is. For example, if a cyst is found and it’s growing, the treatment options may vary. Taking preventive measures before it’s too late can lead to different approaches… However, if something is noticed after it has grown, it may require surgery. But early diagnosis leads to early treatment, which is also significant…” (P1, 46 y, F).
Misperceptions
According to most participants, preventive health services were considered to be the ‘check-up services’ provided by private hospitals, and access to these services was associated with a good socioeconomic status. There was also a common perception that the technical capabilities of primary healthcare institutions were insufficient for providing preventive health services.
“…even if it’s not every year, I think if we have semi-check-ups or a full check-up at a fully equipped hospital when the doctor recommends it, our bodies will give us the signals. I know that they don’t provide such services at primary healthcare centers. I wouldn’t even bother to ask! I know they don’t do it because, for example, they check some blood values, but they don’t check for thyroid levels…” (P3, 29 y, F).
“…this check-up isn’t something that everyone can afford, especially for those with low incomes! Some individuals struggle just to buy bread for their families. There are even people who can’t find the money for bus fare to see a doctor, much less go for a check-up!…” (P20, 49 y, M).
The avoidance of diagnosis and stigmatization were among the factors affecting access to preventive health services.
“…If I give a blood sample, will they check my sugar levels or look for other diseases? Later, I thought, never mind; it’s better not to know. I remind myself to stay positive and avoid hearing anything that might disturb me…” (P5, 52 y, F).
“…I said, Come on, we lived in poverty; seeing a dietitian is for rich people…” (P20, 49 y, M).
Patient-doctor communication and sense of trust
According to individuals, family physicians should closely monitor and get to know their patients on a regular basis. Additionally, it was stated that the communication between patients and doctors is important for accessing healthcare services and ensuring treatment adherence.
“…Actually, there is a need for more family physicians… Health should be monitored from an early age. If they can’t establish communication with their patients, they won’t be able to provide proper follow-up. They may glance at a computer screen, but decisions made on a computer in the U.S. don’t necessarily apply here. Communication is fundamental; keep that in mind! We all tend to rush to conclusions…” (P2, 40 y, M).
“…I need to have some level of trust in the doctor; if I don’t, I won’t take the medication they prescribe or go to a place I’m uncertain about. Even if I do go, I probably won’t follow their recommendations. That’s how I feel…” (P15, 63 y, F).
The lack of trust among some participants had led them to seek alternative medicine.
“…I view the whole medication situation as a business; no one really gets completely healed… It’s just about making money! I had no idea I could manage my diabetes, so I opted for cupping therapy and even had treatment for my eyes. For the first time in my life, I was able to sleep well…” (P23, 31 y, M).
Barriers
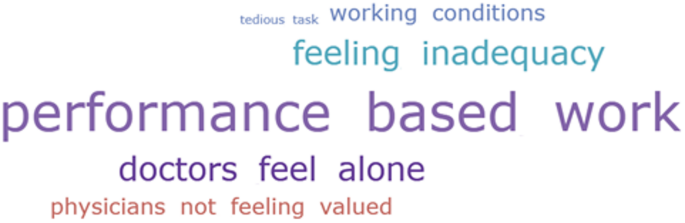
Most family physicians indicated that there are several barriers preventing the optimal implementation of preventive health practices at family health centers (Fig. 4).
“…If the system, for instance, mandates that a doctor must see 70 patients to receive payment, the doctor will prioritize meeting that quota, potentially at the expense of institutional service quality. However, if compensation is assured regardless of patient volume, the doctor is more likely to focus on delivering higher-quality care…” (FP-2, 29 y, M).
“…I observe a substantial difference between my experience as a general practitioner in family medicine and my current role. At that time, due to feeling some educational gaps, I found myself needing to refer patients more frequently. However, my reliance on referrals has now significantly diminished…” (FP-4, 28 y, F).
Additionally, the perception among physicians that they are not trusted has also negatively impacted the effective delivery of services.
“… there is a general lack of awareness regarding the full range of capabilities that family physicians possess, and many family physicians themselves are not fully cognizant of their own potential. Even those who are aware often do not feel adequately skilled or motivated to utilize their competencies effectively. The rising trend of chronic diseases is significant, but physicians’ lack of confidence in their abilities also leads to an underutilization of available resources, as far as I have observed. I believe this is largely a matter of education and awareness…” (FP-3, 54 y, F).
“… if the patient realizes that you are making an effort for their well-being and trusts you, they will return for follow-up appointments. It’s somewhat dependent on the communication between you and the patient…” (FP-4, 28 y, F).
Efforts
According to family physicians, patients emphasized the importance of a holistic approach, perceiving each patient visit as an opportunity for preventive health interventions.
“…For example, today a patient presented for consultation, accompanied by her child. Upon her arrival, I inquired about cervical cancer screening, as she is 36 years old. Following this, I referred her to the nurse for preventive measures and also directed her to the nursing staff for cancer screening procedures…” (FP-1, 32 y, M).
“…We do not consider patients merely in relation to diabetes; instead, we adopt a comprehensive approach. Each individual is evaluated holistically, and we view every periodic visit as an opportunity for assessment and intervention. This perspective guides our approach to patient care…” (FP-3, 54 y, F).
Coordination of care and referral system
One of the family physicians underscored the significance of patient collaboration and inter-institutional coordination in the effective implementation of preventive health services.
“… patients are mostly followed up at state hospitals, where there is frequent turnover of physicians, and there is no consistent system for regular patient monitoring. In our training at the Family Health Center, we benefit from the psychologist and dietitian with whom we work, and we refer patients to them. However, there may not be any feedback from them to us if there are no personal relationships!.” (FP-3, 54y, F).
It was also stated that the absence of a referral system poses challenges in the coordination of patient care.
“… the issue is the lack of an official referral system! There is no network in which various specialties refer to one another, such as one region consulting another region…” (FP-5, 37 y, F).
According to one of the family physicians, there is a need for collaboration with non-health sectors in the context of preventive health perception.
“… chronic diseases cannot be addressed solely at the primary care level. Various stakeholders, including workplaces, urban environments, and municipalities, play a role in this context. In fact, a broad range of entities, such as the media and health policies, are involved.…” (FP-3, 54 y, M).