This study applied advanced geospatial and temporal analytical techniques to assess the provincial distribution and temporal dynamics of GC incidence in Iran from 2014 to 2018, drawing on data from the INPCR. In contrast to earlier research that primarily examined national-level trends or utilized aggregated pathology-based data [22, 23], this investigation enabled the precise computation of ASRs and uncovered marked inter-provincial variations in GC incidence. This detailed resolution is essential for gaining a deeper insight into the geographic heterogeneity of cancer risk, which broader national studies often overlook. The detection of specific high- and low-incidence clusters offers vital guidance for public health strategies, especially regarding the allocation of resources for targeted screening and preventive measures. Such approaches ensure that interventions are customized to meet the unique requirements of high-risk communities [38, 39]. Additionally, the temporal component of the analysis identified varying trends across geographic and demographic segments. While certain areas demonstrated a decrease in incidence, possibly due to the success of public health initiatives, others showed an upward trajectory that demands prompt attention [3, 19]. These spatial inconsistencies in trends indicate that prevention efforts may vary in efficacy across regions, highlighting the importance of localized strategies. The results of this study pinpoint notable spatial and temporal disparities in GC incidence, which could inform hypotheses for subsequent etiological studies or focused screening programs in elevated-risk zones [40].
Moreover, this research advocates for forthcoming studies to integrate additional socioeconomic, environmental, and lifestyle variables to dissect the root causes of these regional differences in GC incidence. Elements like tobacco consumption, diets high in salt, and Helicobacter pylori (H. pylori) infection have been associated with heightened GC risk in various populations and may play a role in the observed geographic patterns. Nevertheless, it is critical to recognize that the ecological correlations presented herein do not imply causation. Thus, we suggest that future investigations utilize individual-level data to more rigorously evaluate the contributions of potential risk factors, especially in the high-incidence provinces delineated in this work. These efforts could yield crucial understandings of the behavioral and environmental elements driving GC and assist in formulating precise interventions for high-burden areas.
Incidence rate
The examination of GC incidence in Iran over 2014–2018 indicated a mean ASR of 16.2 per 100,000, which falls below the 2020 global standard of 17.5 per 100,000 [4]. Relative to other Asian nations with elevated GC rates, Iran’s ASR is considerably lower than Mongolia’s (48.8 per 100,000) [41], and South Korea’s (29.6 per 100,000) [42]. Yet, in the Middle Eastern landscape, Iran’s rate surpasses those of adjacent countries, including Pakistan (4.2 per 100,000), Armenia (11.1 per 100,000), Turkey (12.6 per 100,000), Azerbaijan (12.7 per 100,000), and Iraq (4.8 per 100,000) [4]. Stratified by gender, the ASR stood at 22.2 per 100,000 for males and 10.4 per 100,000 for females. Although Iran’s male rate is less than in high-prevalence countries like Japan (48.1 per 100,000), and the female rate is under Mongolia’s (20.7 per 100,000) [4], both exceed rates in several Western developed nations, such as the United States (overall: 6.9 per 100,000; males: 9, females: 5.2) [10], the United Kingdom (overall: 10.1 per 100,000; males: 14.6, females: 6.4) [43], and Australia (overall: 7.9 per 100,000; males: 10.7, females: 5.3) [44].
These comparisons position Iran’s GC burden as intermediate on a global scale, emphasizing the necessity for deeper exploration into subpopulations facing increased risk. The data also reveal substantial geographic and demographic inequalities within Iran. Provincial analyses showed Ardabil with the highest ASR (34.2 per 100,000 overall; males: 46.2, females: 22.4), outpacing nearby areas like East-Azerbaijan (24.1 per 100,000) and Zanjan (11.8 per 100,000). Ardabil’s rates also exceed those in certain regions of neighboring countries, such as Amasya in Turkey (overall: 14 per 100,000; males: 22.1, females: 7.1) [45], and in Iraq, Erbil (overall: 3.6 per 100,000; males: 3.6, females: 2.6) and Duhok (overall: 2.1 per 100,000; males: 2.1, females: 1.5) [46]. On an international level, Ardabil’s figures are akin to those in rural northwest China (28.5 per 100,000) [47] and high-risk Indian districts like Aizawl (44.2 per 100,000) [48]. yet below South Korea’s Chungnam (34.7 per 100,000) [49] and Mongolia’s UVS region (53.01 per 100,000) [50]. Relative to developed areas, Ardabil’s rates surpass Canadian provinces such as Newfoundland and Labrador (13.7 per 100,000) [51], and metropolitan France (males: 6.3 per 100,000, females: 2.7 per 100,000) [52]. This variability marks Ardabil as a key GC hotspot in Iran.
The sustained high incidence in Ardabil likely arises from a complex interplay of environmental, lifestyle, and genetic factors. Prior research has identified a notable prevalence of gastric cardia cancer here, potentially linked to high H. pylori infection rates, excessive salt consumption, and intake of preserved foods [23, 53]. Local dietary habits, including smoked and preserved meats, may facilitate the creation of carcinogenic N-nitroso compounds, heightening GC risk [54, 55]. Elevated smoking prevalence in Ardabil (males: 33.4%, females: 1.4%) [56], above national levels (males: 19.8–21.7%, females: 0.94–3.6%) [57], further positions tobacco as a key modifiable factor [53]. These insights stress the urgency for targeted research and public health measures to tackle the multifaceted risks in Ardabil.
Gender-specific
Recent evidence underscores a pronounced male predominance in GC incidence in Iran, with a five-year ASR of 107.8 per 100,000 in males versus 50.5 per 100,000 in females, indicating a 2.1-fold disparity. This exceeds ratios in Australia (approximately 2.0) [44] and the United States (approximately 1.7) [10], though slightly below the United Kingdom’s (approximately 2.3) [43]. The gender gap may stem from biological and behavioral influences. Biologically, estrogen’s protective role in premenopausal women could lower GC risk, waning post-menopause, while androgens might enhance carcinogenic pathways in men [58]. Men may also face greater H. pylori susceptibility, a primary GC risk factor [59]. Behaviorally, higher male smoking rates and occupational exposures (e.g., dust, fumes) contribute [23]. Histological variations, with intestinal-type GC more frequent in males and diffuse-type in younger individuals and females, imply gender-specific genetic and epigenetic roles [60]. These observations call for gender-focused prevention and intervention frameworks to address the elevated GC load in Iranian males.
Age groups
In Iran, the average diagnosis age for GC is 66.4 years, somewhat below that in the United States (68 years), Canada (68.4 years), Australia (70 years), and the United Kingdom (73.2 years) [10, 43, 44, 51]. The age pattern features low rates in youth, a sharp increase post-50, and peaks in seniors, aligning with global trends but differing from earlier onsets in high-risk Asian groups like Japan and South Korea. This may relate to H. pylori exposure timing or lifestyle risk buildup variations. While similar to U.S. patterns (rise after 50), Iran’s escalation begins earlier and is steeper than in the United Kingdom and Australia (significant rises 65–85) [10, 43, 44]. In Canada, 75% of diagnoses occur over 60 [51]. and U.K./Nordic studies note inflections at 50–65 [43, 61]. This could link to childhood H. pylori prevalence in Iran [23]. Post-70 plateaus might indicate cohort effects, with younger groups at lower risk. Additional factors include age-related changes like gastric acidity decline, genomic mutations, immune senescence, nutritional deficits, and comorbidities [62]. Acknowledging these trends is vital for crafting screening programs, especially as younger patients often have advanced disease. With rising life expectancy in Iran, addressing age-specific risks is key for health planning.
Temporal trend
From 2014 to 2018, GC incidence in Iran showed stability with slight ASR fluctuations, differing from declines in high-income nations (-2.1% to -1.7% annually). Canada saw a drop from 9.28 to 6.59 per 100,000 (1992–2010, ~ 30% reduction), and the United Kingdom from 23 to 10 per 100,000 (1993–2018) [43], credited to lower H. pylori and tobacco use [17]. Iran’s lack of decline may involve limited screening and 25% clarithromycin resistance in H. pylori [63]. Ardabil’s local screening for over-45s has cut advanced diagnoses via serology and endoscopy [64], but national progress lags. Iran’s lower diagnosis age (66.4 years) versus Western countries suggests early H. pylori cohort effects, proposing pediatric screening in endemic zones [65]. The plateau reflects ongoing risks like H. pylori, poor diets, tobacco, and slower socioeconomic gains limiting food preservation improvements and reductions in nitrates, salt, and processed foods [23].
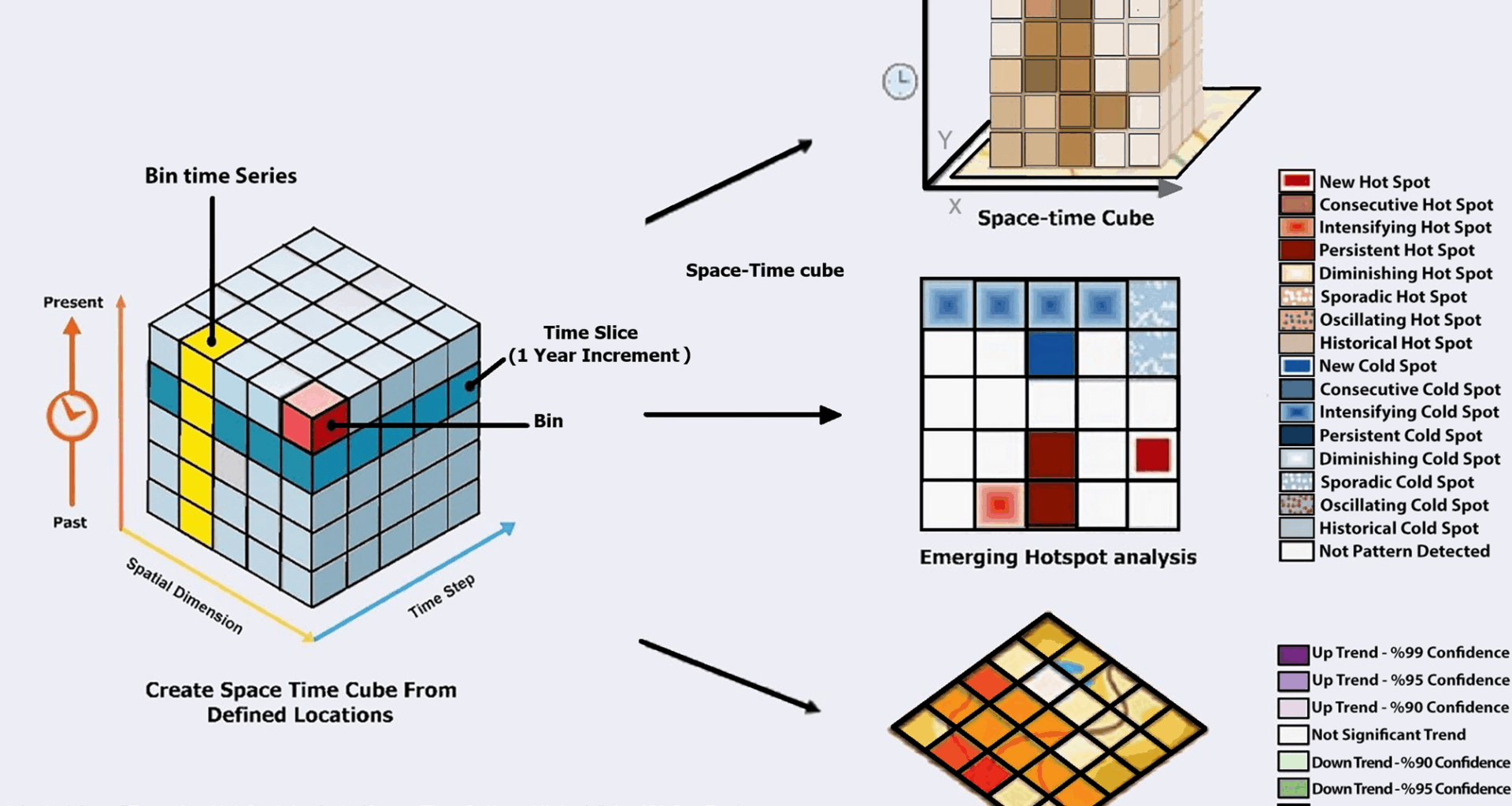
Spatial distribution
GC’s spatial patterns correlate with geographic and environmental factors, as shown by heterogeneous rates globally [19, 20, 66, 67]. These reveal disparities tied to local exposures, lifestyles, and socioecological settings. Iran resides in the gastrointestinal cancer belt, from East Asia through Central Asia to the Middle East, marked by high GC due to endemic H. pylori, salt-rich diets, and genetics [22]. This includes high-risk zones in northeastern China, Kazakhstan, Turkmenistan, and northern Iran, far above Northern Europe, Africa, and North America [68]. Intra-Iran, provincial differences are stark, with peaks in Ardabil and Caspian areas, lows in southern coasts [69]. The north-south gradient likely involves environmental and behavioral interactions. Northern humidity aids H. pylori transmission, though causal links need individual data. Southern diets high in antioxidants and seafood may protect [65]. Global parallels include higher inland rates in China, Spain, and Canada versus coasts [70,71,72]. Clusters pinpoint Ardabil and Caspian as high-risk, aligning with prior reports. Chinese high-risk clusters in Gansu, Henan, Hebei contrast southern lows [70]. Canadian inland like Saskatchewan, Manitoba show highs, maritime lows [67]. These may link to pesticides and groundwater nitrates fostering nitrosation and carcinogenesis [73].
The transboundary nature of these risks, seen in shared high-incidence clusters between northern Iran and Central Asia, calls for regional collaborations to address common drivers. The findings underscore the need for tailored interventions that account for local risk landscapes. In high-incidence regions, strategies could include stricter regulation of agricultural chemicals, improved water quality infrastructure, and public health campaigns aimed at reducing salt intake and tobacco use. Conversely, protective dietary practices observed in southern Iran may inform prevention strategies elsewhere. Future research can prioritize longitudinal studies to clarify the causal pathways linking environmental exposures, genetic factors, and GC incidence, especially in understudied high-risk clusters. Such efforts will strengthen the evidence base for spatially adaptive policies designed to mitigate GC’s disproportionate burden in vulnerable regions.
Limitation
This analysis provides key insights into GC incidence in Iran (2014–2018) but has limitations from INPCR data. The 2014–2018 scope, due to unavailable recent data, may miss current trends. Underestimation and missing provincial records (3.3%) could bias results, with diagnostic infrastructure variations affecting patterns. However, relative differences and methods like Global Moran’s I and Emerging Hot Spot Analysis suggest authentic disparities. Province-specific imputation for 3.9% missing data maintained spatial accuracy but might miss temporal nuances; deemed suitable given low missingness and descriptive focus. The ecological design restricts causality inference and individual risk exploration (e.g., H. pylori, diet, genetics), masking within-province variations. Unmeasured confounders like socioeconomic status, access, and exposures may influence outcomes. INPCR lacks local health unit data, limiting variability analysis. Annual aggregation smooths short-term changes; five-year span may not capture evolving risks. Yet, INPCR’s consistency (completeness ≤ 1.5% variation, no protocol shifts) and standardized CIs bolster reliability. Advanced geospatial methods offer robust GC pattern insights. Future work with individual-level, molecular, clinical, and epidemiological data is needed to unpack drivers and refine interventions.
Recommendation
Drawing from this study’s results, we propose: (1) in-depth epidemiological probes into behavioral and genetic GC determinants for personalized interventions, focusing H. pylori, diet, and predispositions; (2) prioritized endoscopic screening in high-incidence clusters (e.g., Ardabil) for early detection; (3) culturally sensitive campaigns targeting modifiable risks in high-risk areas; (4) bolstering surveillance via provider training, navigation systems, and equitable diagnostics nationwide.