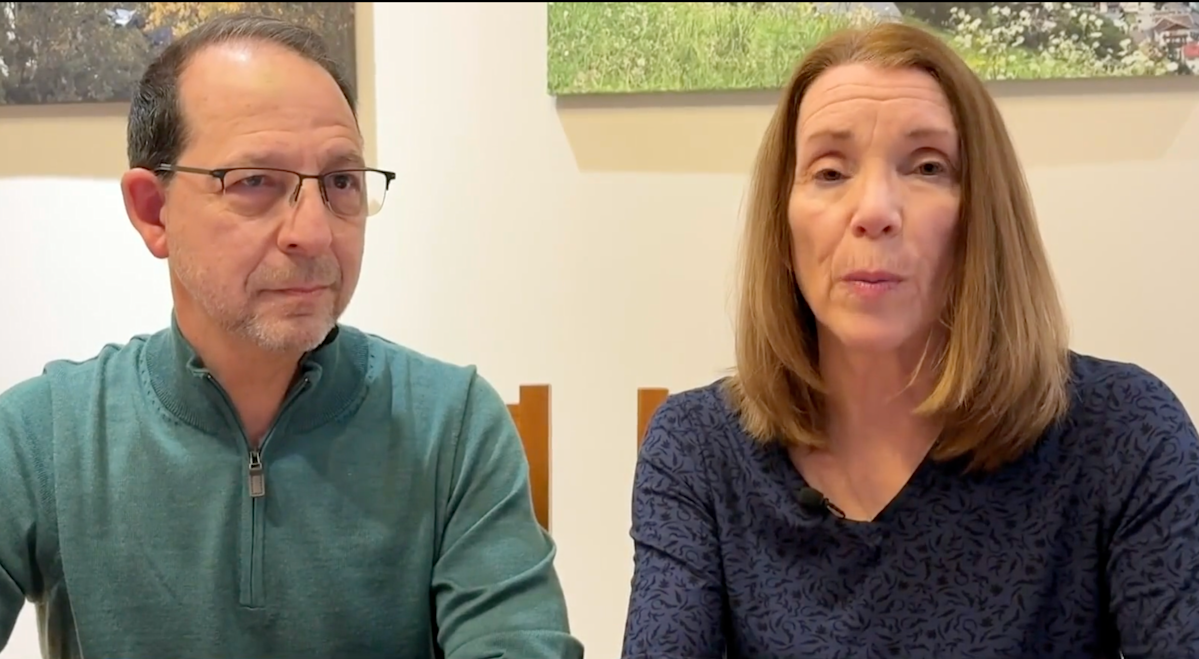
With professional backgrounds in economics and accounting, Barbara Brockway and Matt Padula might seem like they’d be able to have retirement mapped down to the dollar. But one line item proved harder to forecast: health insurance.
After enhanced Affordable Care Act subsidies expired going into 2026, the retired Georgia couple saw their monthly Marketplace premium jump from $1,600 to $3,200, which is nearly $39,000 more for the year (1).
At 62, they’re still years away from Medicare eligibility. And because they “wouldn’t even dream” of going without coverage, they say the higher premiums are forcing them to rethink retirement spending. Brockway told CBS Atlanta they’ll need to cut back on everyday expenses — including discretionary costs like dining out and vacations.
Marketplace subsidies once again phase out at higher income levels. As of 2026, households generally must earn no more than 400% of the federal poverty level to qualify for financial assistance — meaning some middle-income enrollees may now receive little or no subsidy.
Some households who previously benefited from enhanced subsidies are now facing higher premiums. And early enrollment data suggests some consumers may be reconsidering Marketplace coverage altogether.
CMS data shows Marketplace enrollment is already trending lower in early 2026. As of Jan. 12, 2026, about 22.8 million people had signed up for Marketplace coverage, down from 24.16 million at the same point in 2025 — a decline of roughly 1.4 million enrollees year over year (3, 4).
Across all demographics, a KFF survey found that roughly 50% of Americans say it’s a struggle to keep up with healthcare costs. Researchers found these rising costs were enough to make one in three Americans defer coverage. But even among those with health insurance, 4 in 10 say they’re nervous about affording their premiums (5).
It’s not just consumers feeling squeezed — insurers may also be reassessing the Marketplace in some states.
The Urban Institute found that 21 states reported fewer insurers in the Marketplace (6), with Aetna being one of the largest to opt out (7). Researchers speculated that insurers are leaving due to the uncertainty created by the loss of 2026 subsidies and fears that they may have to cover “sicker” customers (6).
Story Continues