Petäjä EM, Yki-Järvinen H. Definitions of normal liver fat and the association of insulin sensitivity with acquired and genetic NAFLD-A systematic review. Int J Mol Sci. 2016. https://doi.org/10.3390/ijms17050633.
Cobbina E, Akhlaghi F. Non-alcoholic fatty liver disease (NAFLD) – pathogenesis, classification, and effect on drug metabolizing enzymes and transporters. Drug Metab Rev. 2017;49(2):197–211. https://doi.org/10.1080/03602532.2017.1293683.
Rinella ME, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Ann Hepatol. 2024;29(1): 101133. https://doi.org/10.1016/j.aohep.2023.101133.
Eslam M, George J. MASLD: now is the time to capitalize on the momentum. J Hepatol. 2021;74(5):1262–3. https://doi.org/10.1016/j.jhep.2021.02.002.
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–9. https://doi.org/10.1016/j.jhep.2020.03.039.
Adams LA, Angulo P. Recent concepts in non-alcoholic fatty liver disease. Diabet Med. Sep 2005;22(9):1129–33. https://doi.org/10.1111/j.1464-5491.2005.01748.x.
Eslam M, Sanyal AJ, George J. MASLD: A Consensus-Driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology May. 2020;158(7):1999–e20141. https://doi.org/10.1053/j.gastro.2019.11.312.
Younossi Z, Tacke F, Arrese M, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019;69(6):2672–82. https://doi.org/10.1002/hep.30251.
Masoodi M, Gastaldelli A, Hyötyläinen T, et al. Metabolomics and lipidomics in NAFLD: biomarkers and non-invasive diagnostic tests. Nat Rev Gastroenterol Hepatol. 2021;18(12):835–56. https://doi.org/10.1038/s41575-021-00502-9.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with Long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology Aug. 2015;149(2):389–e9710. https://doi.org/10.1053/j.gastro.2015.04.043.
Kruithof EK. Plasminogen activator inhibitors–a review. Enzyme. 1988;40(2–3):113–21. https://doi.org/10.1159/000469153.
Levine JA, Oleaga C, Eren M, et al. Role of PAI-1 in hepatic steatosis and dyslipidemia. Sci Rep. 2021;11(1): 430. https://doi.org/10.1038/s41598-020-79948-x.
Alessi MC, Juhan-Vague I. PAI-1 and the metabolic syndrome: links, causes, and consequences. Arterioscler Thromb Vasc Biol. 2006;26(10):2200–7. https://doi.org/10.1161/01.Atv.0000242905.41404.68.
Kaji H. Adipose Tissue-Derived plasminogen activator Inhibitor-1 function and regulation. Compr Physiol Sep. 2016;15(4):1873–96. https://doi.org/10.1002/cphy.c160004.
Jin R, Krasinskas A, Le NA, Konomi JV, Holzberg J, Romero R, et al. Association between plasminogen activator inhibitor-1 and severity of liver injury and cardiovascular risk in children with non-alcoholic fatty liver disease. Pediatr Obes. 2018;13(1):23–9. https://doi.org/10.1111/ijpo.12183.
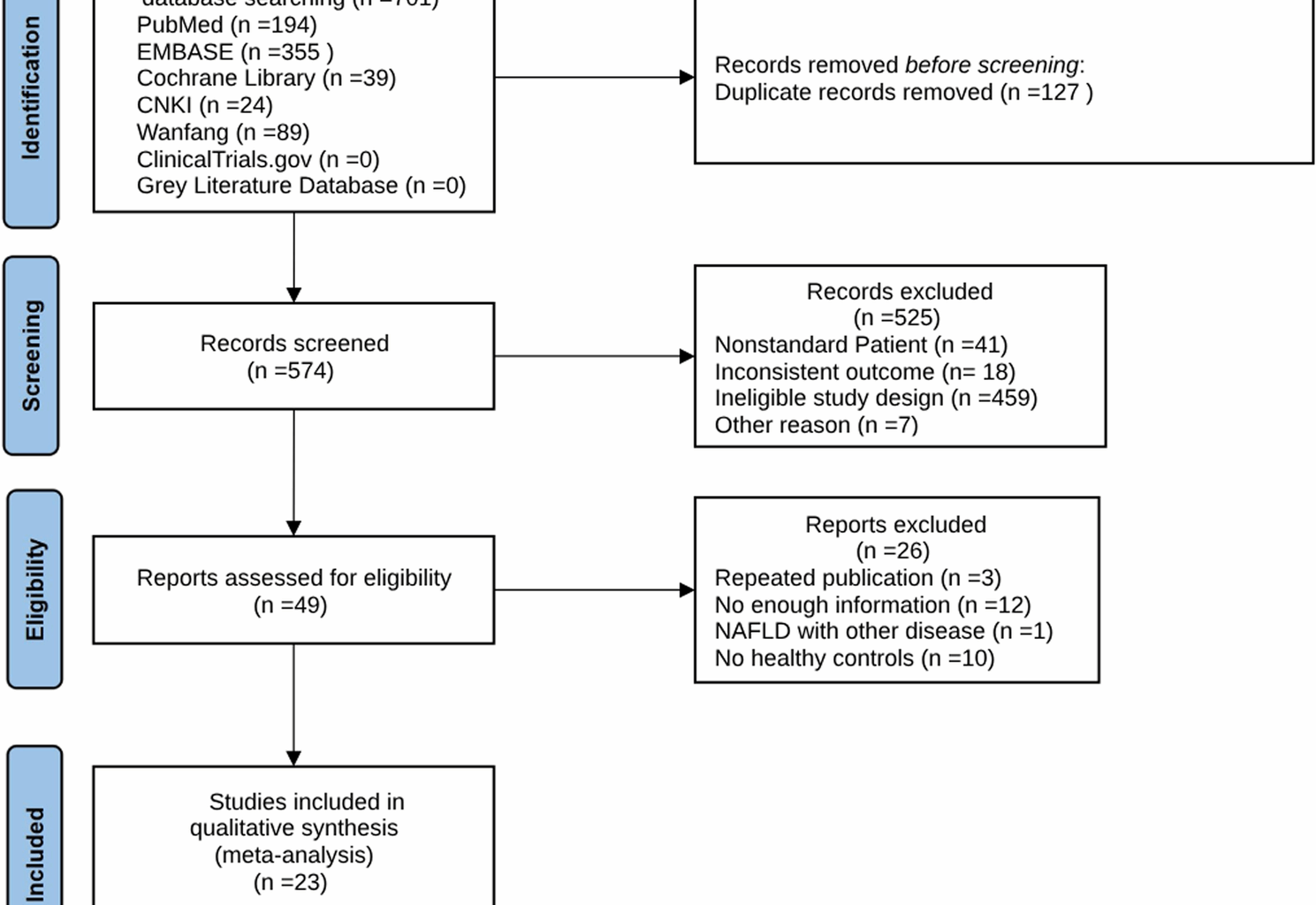
Higgins JPT, Thomas J, Chandler J, (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.5. Cochrane. 2024. www.training.cochrane.org/handbook. Accessed 24 August 2024.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MASLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40(9):2082–9. https://doi.org/10.1111/liv.14548.
Stang A. Critical evaluation of the Newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–805. https://doi.org/10.1177/0962280216669183.
Schmidt FL, Oh IS, Hayes TL. Fixed- versus random-effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol. 2009;62(Pt 1):97–128. https://doi.org/10.1348/000711007×255327.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Younossi ZM. Non-alcoholic fatty liver disease – a global public health perspective. J Hepatol. 2019;70(3):531–44. https://doi.org/10.1016/j.jhep.2018.10.033.
Abdel-Razik A, Mousa N, Shabana W, Yassen AH, Abdelsalam M, Wahba MM, et al. De Novo portal vein thrombosis in Non-Cirrhotic Non-Alcoholic fatty liver disease: A 9-Year prospective cohort study. Front Med (Lausanne). 2021;8:650818. https://doi.org/10.3389/fmed.2021.650818.
Alvares-da-Silva MR, de Oliveira CP, Stefano JT, Barbeiro HV, Barbeiro D, Soriano FG, et al. Pro-atherosclerotic markers and cardiovascular risk factors one year after liver transplantation. World J Gastroenterol. 2014;20(26):8667–73. https://doi.org/10.3748/wjg.v20.i26.8667.
Bai XP, Yang YL, Gao M, Li X, Zhao BZ. The influence of serum triglycerides on plasminogen activator inhibitor-1 and adiponectin in patients with nonalcoholic fatty liver disease. Chin J Gastroenterol Hepatol. 2014;23(04):435–7.
Bilgir O, Bilgir F, Bozkaya G, Calan M. Changes in the levels of endothelium-derived coagulation parameters in nonalcoholic fatty liver disease. Blood Coagul Fibrinolysis. 2014;25(2):151–5. https://doi.org/10.1097/mbc.0000000000000009.
Cao Y, Li L. Relationship of non-alcoholic steatohepatitis with arterial endothelial function and atherosclerosis. Chin J Hepatol. 2014;22(3):205–8. https://doi.org/10.3760/cma.j.issn.1007-3418.2014.03.012.
Chang ML, Hsu CM, Tseng JH, Tsou YK, Chen SC, Shiau SS, et al. Plasminogen activator inhibitor-1 is independently associated with non-alcoholic fatty liver disease whereas leptin and adiponectin vary between genders. J Gastroenterol Hepatol. 2015;30(2):329–36. https://doi.org/10.1111/jgh.12705.
Chen HY, Zhu SW, Wu WJ, Bu RF. Effect of serum triglyceride on PAI-1 and APN levels in patients with nonalcoholic fatty liver disease. Mod Diagn Treat. 2015;26(15):3375–7.
Deng YQ, Fan XF, Li JP. Fibrinolytic status in nonalcoholic fatty liver patients with different glucose tolerance levels. Zhejiang J Integr Traditional Chin Western Med. 2005(09):547–8.
Deng YQ, Fan XF, Li YD. Relationship between phlegm-stasis syndrome and fibrinolytic status in patients with non-alcoholic fatty liver. Chin J Integr Tradit Western Med. 2005;25(1):22–4.
Fang LM, Shen NY, Ma QH, Chen KL, Liu D. Changes and significance of plasminogen activator inhibitor-1 level in nonalcoholic fatty liver disease. Chin J Practical Med. 2010;37(13):74–5. https://doi.org/10.3760/cma.j.issn.1674-4756.2010.13.036.
Jiang X, Sun M. Changes and clinical significance of serum PAI-1 in nonalcoholic fatty liver disease. Chin J Lab Diagn. 2020;24(06):953–5.
Kargili A, Cipil H, Karakurt F, Kasapoglu B, Koca C, Aydin M, et al. Hemostatic alterations in fatty liver disease. Blood Coagul Fibrinolysis. 2010;21(4):325–7. https://doi.org/10.1097/mbc.0b013e328337b3f8.
Li Y, Liu L, Wang B, Wang J, Chen D. Simple steatosis is a more relevant source of serum inflammatory markers than omental adipose tissue. Clin Res Hepatol Gastroenterol. 2014;38(1):46–54. https://doi.org/10.1016/j.clinre.2013.08.006.
Nier A, Huber Y, Labenz C, Michel M, Bergheim I, Schattenberg JM. Adipokines and endotoxemia correlate with hepatic steatosis in non-alcoholic fatty liver disease (NAFLD). Nutrients. 2020. https://doi.org/10.3390/nu12030699.
Targher G, Bertolini L, Rodella S, Lippi G, Franchini M, Zoppini G, et al. NASH predicts plasma inflammatory biomarkers independently of visceral fat in men. Obesity. 2008;16(6):1394–9. https://doi.org/10.1038/oby.2008.64.
Thuy S, Ladurner R, Volynets V, Wagner S, Strahl S, Königsrainer A, et al. Nonalcoholic fatty liver disease in humans is associated with increased plasma endotoxin and plasminogen activator inhibitor 1 concentrations and with fructose intake. J Nutr. 2008;138(8):1452–5. https://doi.org/10.1093/jn/138.8.1452.
Tian S, Liu HL, Zhong XQ. Diagnostic significance of serum plasminogen activator inhibitor-1 level for nonalcoholic fatty liver disease. Mod J Integr Traditional Chin Western Med. 2020;29(06):585–8.
Volynets V, Küper MA, Strahl S, Maier IB, Spruss A, Wagnerberger S, et al. Nutrition, intestinal permeability, and blood ethanol levels are altered in patients with nonalcoholic fatty liver disease (NAFLD). Dig Dis Sci. 2012;57(7):1932–41. https://doi.org/10.1007/s10620-012-2112-9.
Yang YQ, Zhang Y, Kou SJ, Dong L. Study on the relationship between fatty liver severity and oxidative stress,saa, CRP and cerebral arteriosclerosis in fatty liver patients. Chin J Integr Med. 2022;32(6):520–4. https://doi.org/10.3969/j.issn.1005-0264.2022.06.012.
Xu L, Ding XY, Weng YS, Miu M, Yuan JY. Changes in the coagulation fibrinolysis system in nonalcoholic fatty liver disease. Chin J Rural Med Pharm. 2011;18(11):59–60. https://doi.org/10.19542/j.cnki.1006-5180.2011.11.044.
Wang C, Yan J, Zhang S, Xie Y, Nie Y, Chen Z, et al. Screening new blood indicators for Non-alcoholic fatty liver disease (NAFLD) diagnosis of Chinese based on machine learning. Front Med (Lausanne). 2022;9:771219. PubMed PMID: 35755070; PubMed Central PMCID: PMCPMC9218755.
Yener S, Akarsu M, Demir T, Akinci B, Sagol O, Bayraktar F, et al. Plasminogen activator inhibitor-1 and thrombin activatable fibrinolysis inhibitor levels in non-alcoholic steatohepatitis. J Endocrinol Invest. 2007;30(10):810–9. https://doi.org/10.1007/bf03349221.
Zhu JZ, Zhu HT, Dai YN, Li CX, Fang ZY, Zhao DJ, et al. Serum periostin is a potential biomarker for non-alcoholic fatty liver disease: a case-control study. Endocrine. 2016;51(1):91–100. https://doi.org/10.1007/s12020-015-0735-2.
Cariou B, Byrne CD, Loomba R, Sanyal AJ. Nonalcoholic fatty liver disease as a metabolic disease in humans: A literature review. Diabetes Obes Metab. 2021;23(5):1069–83. https://doi.org/10.1007/s12020-015-0735-2.
Fassio E, Alvarez E, Domínguez N, Landeira G, Longo C. Natural history of nonalcoholic steatohepatitis: a longitudinal study of repeat liver biopsies. Hepatology. 2004;40(4):820–6. https://doi.org/10.1002/hep.20410.
Chakravarthy MV, Neuschwander-Tetri BA. The metabolic basis of nonalcoholic steatohepatitis. Endocrinology, Diabetes & Metabolism. 2020;3(4): e00112. https://doi.org/10.1002/edm2.112.
Cusi K, Chang Z, Harrison S, Lomonaco R, Bril F, Orsak B, et al. Limited value of plasma cytokeratin-18 as a biomarker for NASH and fibrosis in patients with non-alcoholic fatty liver disease. J Hepatol. 2014;60(1):167–74. https://doi.org/10.1016/j.jhep.2013.07.042.
Hu J, Ke Y, Wu F, Liu S, Ji C, Zhu X, et al. Circulating Irisin levels in patients with nonalcoholic fatty liver disease: A systematic review and Meta-Analysis. Gastroenterol Res Pract. 2020;2020:8818191. https://doi.org/10.1155/2020/8818191.
Polyzos SA, Aronis KN, Kountouras J, Raptis DD, Vasiloglou MF, Mantzoros CS. Circulating leptin in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Diabetologia. 2016;59(1):30–43. https://doi.org/10.1007/s00125-015-3769-3.
Agren A, Jörneskog G, Elgue G, Henriksson P, Wallen H, Wiman B. Increased incorporation of antiplasmin into the fibrin network in patients with type 1 diabetes. Diabetes Care. 2014;37(7):2007–14. https://doi.org/10.2337/dc13-1776.
Du XL, Edelstein D, Rossetti L, Fantus IG, Goldberg H, Ziyadeh F, et al. Hyperglycemia-induced mitochondrial superoxide overproduction activates the hexosamine pathway and induces plasminogen activator inhibitor-1 expression by increasing Sp1 glycosylation. Proc Natl Acad Sci USA. 2000;97(22):12222–6. https://doi.org/10.1073/pnas.97.22.12222.
Chen YQ, Su M, Walia RR, Hao Q, Covington JW, Vaughan DE. Sp1 sites mediate activation of the plasminogen activator inhibitor-1 promoter by glucose in vascular smooth muscle cells. J Biol Chem. 1998;273(14):8225–31.
Beier JI, Arteel GE. Alcoholic liver disease and the potential role of plasminogen activator inhibitor-1 and fibrin metabolism. Exp Biol Med (Maywood). 2012;237(1):1–9. https://doi.org/10.1074/jbc.273.14.8225.
Beier JI, Luyendyk JP, Guo L, von Montfort C, Staunton DE, Arteel GE. Fibrin accumulation plays a critical role in the sensitization to lipopolysaccharide-induced liver injury caused by ethanol in mice. Hepatology. 2009;49(5):1545–53. https://doi.org/10.1002/hep.22847.
Alsharoh H, Ismaiel A, Leucuta DC, Popa SL, Dumitrascu DL. Plasminogen activator inhibitor-1 levels in non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Gastrointestin Liver Dis. 2022;31(2):206–14. https://doi.org/10.15403/jgld-4091.
Simon TG, Trejo MEP, McClelland R, Bradley R, Blaha MJ, Zeb I, et al. Circulating interleukin-6 is a biomarker for coronary atherosclerosis in nonalcoholic fatty liver disease: results from the multi-ethnic study of atherosclerosis. Int J Cardiol. 2018;259:198–204. https://doi.org/10.1016/j.ijcard.2018.01.046.
Ajmera V, Perito ER, Bass NM, Terrault NA, Yates KP, Gill R, et al. Novel plasma biomarkers associated with liver disease severity in adults with nonalcoholic fatty liver disease. Hepatology. 2017;65(1):65–77. https://doi.org/10.1002/hep.28776.
Sookoian S, Castaño GO, Burgueño AL, Rosselli MS, Gianotti TF, Mallardi P, et al. Circulating levels and hepatic expression of molecular mediators of atherosclerosis in nonalcoholic fatty liver disease. Atherosclerosis. 2010;209(2):585–91. https://doi.org/10.1016/j.atherosclerosis.2009.10.011.
Campbell PT, VanWagner LB, Colangelo LA, Lewis CE, Henkel A, Ajmera VH, et al. Association between plasminogen activator inhibitor-1 in young adulthood and nonalcoholic fatty liver disease in midlife: CARDIA. Liver Int. 2020;40(5):1111–20. https://doi.org/10.1111/liv.14417.
Pan JJ, Fallon MB. Gender and Racial differences in nonalcoholic fatty liver disease. World J Hepatol. 2014;6(5):274–83. https://doi.org/10.4254/wjh.v6.i5.274.
Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40(12):1461–5. https://doi.org/10.1038/ng.257.
Zoratti R. A review on ethnic differences in plasma triglycerides and high-density-lipoprotein cholesterol: is the lipid pattern the key factor for the low coronary heart disease rate in people of African origin? Eur J Epidemiol. 1998;14(1):9–21. https://doi.org/10.1023/a:1007492202045.
Lomonaco R, Ortiz-Lopez C, Orsak B, Finch J, Webb A, Bril F, et al. Role of ethnicity in overweight and obese patients with nonalcoholic steatohepatitis. Hepatology. 2011;54(3):837–45. https://doi.org/10.1002/hep.24483.
Souza M, et al. Representation of sex, race and ethnicity in MASH randomised controlled trials: A systematic review and Meta-Analysis. Liver Int. 2025;45(4):e70029. https://doi.org/10.1111/liv.70029.
Crudele L, et al. Fatty liver index (FLI) is the best score to predict MASLD with 50% lower cut-off value in women than in men. Biol Sex Differ. 2024;15(1):43. https://doi.org/10.1186/s13293-024-00617-z.
Lonardo A, et al. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019;70(4):1457–69. https://doi.org/10.1002/hep.30626.
Tague BW. Germ-line transformation of Arabidopsis lasiocarpa. Transgenic Res. 2001;10(3):259–67. https://doi.org/10.1023/a:1016633617908.
Holzberg JR, Jin R, Le NA, Ziegler TR, Brunt EM, McClain CJ, et al. Plasminogen activator Inhibitor-1 predicts quantity of hepatic steatosis independent of insulin resistance and body weight. J Pediatr Gastroenterol Nutr. 2016;62(6):819–23. https://doi.org/10.1097/mpg.0000000000001096.