Study participantsStudy design
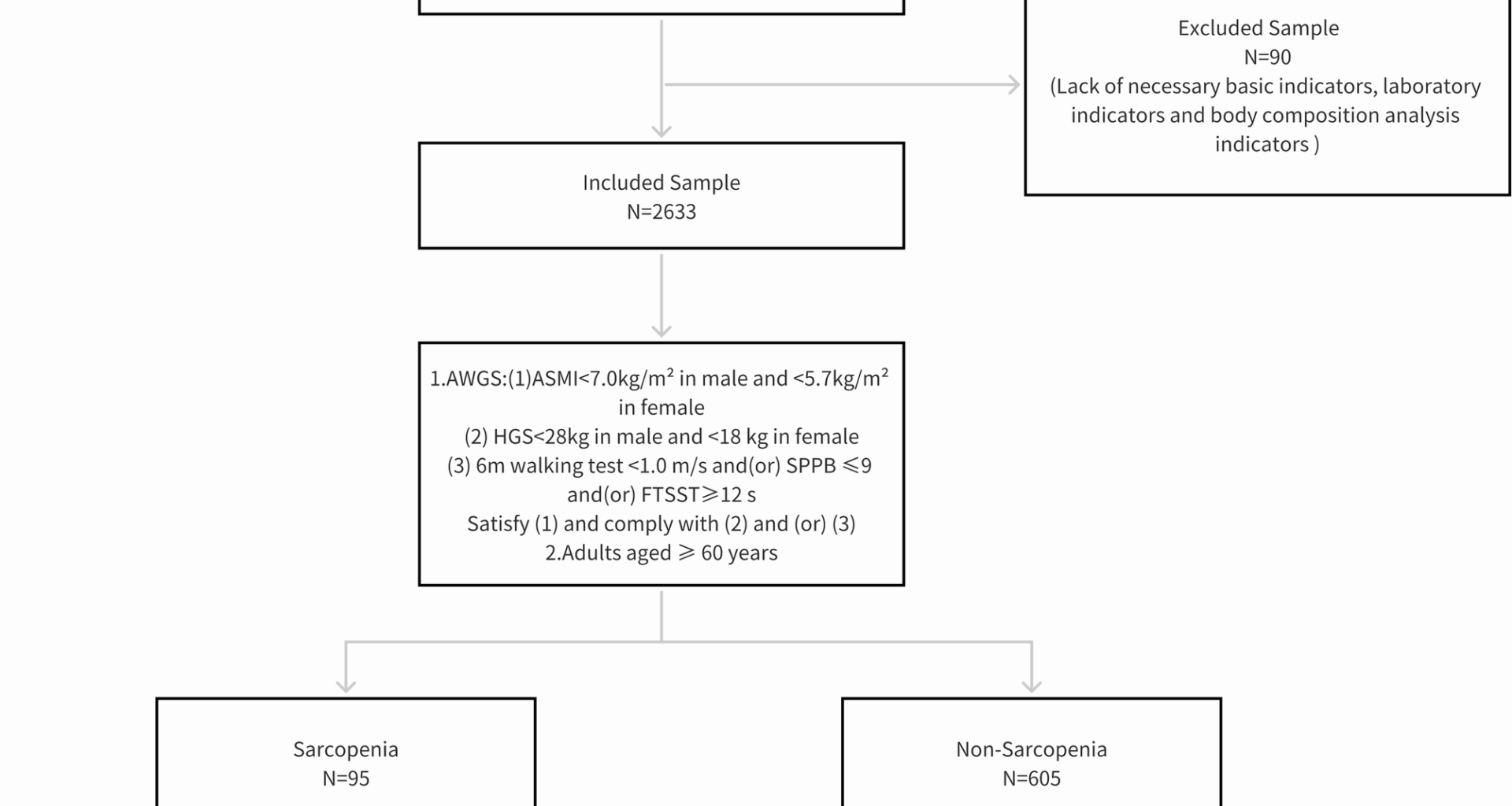
Participants for this cross-sectional study were chosen among the attendees at a physical examination center in Shanghai using convenience sampling from July to December 2023. In order to protect patient privacy, detailed personal information of all patients in this study, including name, address, date of birth, and hospital record number, was anonymised. All patient-identifiable information was deleted or encrypted to comply with the rules of Ethics Committee of the East China Sanatorium in Shanghai and the principles of the Declaration of Helsinki. The reporting of this study conforms to STROBE guidelines [22].
Inclusion criteria
Age ≥ 60 years, permanent resident in Shanghai (residence duration, ≥ 6 months), and able to cooperate with the examinations. All study participants provided informed consent, and the study was approved by the ethics committee (LLSC [2023]004).
Exclusion criteria
The lack of necessary basic indicators, such as sex, age, height, and weight; the lack of necessary laboratory indicators and body composition analysis indicators; and serious cardiovascular, cerebrovascular, lung, kidney, and other diseases.
Data collectionParticipant information and general demographic data
Electronic questionnaires were administered by professionally trained personnel of the physical examination center to analyze the physical examination participants based on standardized procedures, including sex, age, marital status, educational level, occupation, residence, smoking history, drinking history, and previous medical history.
Anthropometric and hemodynamic parametersHeight
The participants removed their shoes and socks, faced the examiner, and stood on the height measuring instrument with bare feet and their backs against the uprights. Two consecutive measurements and average values were taken. The measurement data are accurate to 0.01 cm.
Body weight
The participants were in a fasted state, wore thin clothes, removed their shoes and socks, stood at the center of the weighing machine with bare feet, and relaxed the whole body, and the data were recorded after stabilization. Two consecutive measurements were taken, and the values were averaged. The measurement was accurate to 0.01 kg.
Waist-to-hip ratio (WHR)
The participant stands naturally, with eyes straight ahead, abdomen relaxed, arms folded in front of the chest, and feet together. The tape measure was placed horizontally at 0.5–1 cm of the participant’s navel, the value was read and measured twice consecutively, the average was determined and set to be accurate at 0.01 cm, and the waist circumference (WC) was measured. The participant’s arms naturally drop, and their hands are folded in front of their chest. The tester stood in front of the participant, measured the tape measure horizontally along the pubic symphysis in front and the most prominent point of the gluteus maximus in back, read the value, measured twice successively, took the average value, set the value to be accurate at 0.01 cm, and measured the hip circumference (HC). WHR was obtained by calculating the WC-to-HC ratio.
Blood pressure
The participants sat still for 5 min before their blood pressure was measured. A qualified automatic desk sphygmomanometer was used to measure the blood pressure of the right-upper limb. The palm was above and at the same level as the heart. The cuff was tied to the elbow with 2–3 cm strips, and the tightness could accommodate one finger. Blood pressure was measured three times consecutively, and the systolic blood pressure (SBP) and diastolic blood pressure (DBP) were obtained by averaging. Hypertension was defined according to the World Health Organization (WHO) criteria as: an average SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg.
Laboratory indicators
Participants fasted for 10–12 h starting at 8 PM the previous day and had their elbow venous blood drawn the next morning. The median cubital vein is preferred, followed by the cephalic vein and the basilic vein. The specific vein used for each participant was documented, and the sample handling and storage conditions were ensured to comply with professional standards. The following biochemical markers were measured:
Glycated hemoglobin (HbA1c).
White blood cell count (WBC).
Triglycerides (TG).
Total cholesterol (TC).
Low-density lipoprotein (LDL).
High-density lipoprotein (HDL).
Serum creatinine (Scr).
Uric acid (UA).
Albumin (ALB).
Albumin/Globulin Ratio (A/G).
All laboratory test samples were tested in Huadong Sanatorium Medical Laboratory Center within 24 h after sampling, and all test operations were in line with professional standards.
Body composition measurement
An Inbody multifrequency body composition instrument (InBody 270, BioSpace Co., Korea) with an operating frequency of 250 kHz was used. The body composition was measured using bioelectrical impedance analysis (BIA). Participants stood on the measuring instrument with thin clothes, without shoes or socks, with legs slightly apart, and with the front of their foot and back heel aligned with the bottom of the footprint electrode. Both hands held the left and right handles, the thumb was placed on the side electrode, the remaining four fingers were in contact with the handle electrode, and the arms were slightly extended. The investigator input the required information of the participant using a voice prompt, pressed the start button to start the detection, and kept the position unchanged until the measuring instrument prompted the end of the test. Segmental fat content, muscle mass, and limb SMM were measured at 20,000 and 500 kHz frequencies and 5, 50, and 250 kHz reactance frequencies [23]. Due to the clinical relevance to sarcopenia,detection indicators included in this study: visceral fat area (VFA), SMM, ASM, ASMI. ASM was estimated based on the sum of lean mass from both arms and legs, as reported by the BIA device. ASMI was then calculated as ASM divided by height squared (kg/m²), i.e., ASMI = ASM (kg) / height² (m²).
Muscle strength and function
A grip strength meter was used to measure muscle strength through grip strength. Before the measurement, the grip strength device can be adjusted according to the size of the participant’s hand to ensure that the second knuckle of the index finger remains vertical during the test, and jewelry such as rings and bracelets on the hand should be removed to avoid injury and affect the test result. During the measurement, participants were instructed to stand with their feet slightly apart, and those who could not stand were allowed to sit or lie down. Their upper arms were pressed against the torso, the elbows were bent at 90°, and the handle was squeezed with maximum strength. Both hands were measured twice, and the maximum value of the four measurements was taken as the grip strength value (in kg), and the specific value was set to be accurate at 0.1 kg. The muscle function was measured by 6-m walking speed, and the time required to walk 6 m from a standing position at normal speed was recorded with an electronic timer.
Diagnostic criteria
The diagnostic criteria recommended by the AWGS in 2019 were as follows: (1) when using BIA, ASMI of 2 in males and ASMI of 2 in females is the standard; (2) grip strength of 24]. Obesity is defined as the percentage of body fat (PBF) recommended by the World Health Organization (WHO). PBF of ≥ 25% in males and ≥ 35% in females are considered obese [25]. Participants with both sarcopenia and obesity were defined as having SO.
Statistical analysis
The IBM SPSS Statistics version 22.0 was used for statistical analysis. Categorical variables are expressed as numbers and percentages (n [%]), and continuous variables are expressed as the mean ± standard deviation. Differences between sarcopenia and non-sarcopenia groups in demographic and biochemical indicators were assessed using independent-samples t-tests for continuous variables and Pearson’s chi-squared tests for categorical variables. Prevalence rates of sarcopenia and SO across sex and age groups were compared using the chi-squared test. Sex-specific comparisons of sarcopenic participants were conducted using independent-samples t-tests to better understand demographic patterns and potential risk stratification of sarcopenia and SO, we performed subgroup analyses based on sex (male vs. female). These stratifications help identify vulnerable populations and inform targeted prevention strategies. Univariate logistic regression analyses were conducted to examine associations between sarcopenia and individual covariates, including age, sex, BMI, PBF, and biochemical indicators. Multivariate logistic regression was performed by including covariates based on both univariate analysis and previously reported associations with sarcopenia in the literature, to identify independent predictors. Missing data were evaluated prior to analysis. Variables with more than 30% missing values were excluded. For participants with over 20% missing data, cases were removed from the analysis. If missing data accounted for less than 3% of the total dataset, multiple imputation using chained equations was applied. P