Our comprehensive analysis of the GBD 2021 data elucidates significant temporal and spatial patterns in the global burden of LOCC from 1990 to 2021, with projections extending to 2036. The study revealed substantial disease burden metrics, with 421,577 incident cases, 208,379 deaths, and 5,874,070 DALYs documented in 2021. These findings demonstrate the persistent public health challenge posed by LOCC, characterized by marked heterogeneity across geographical regions and demographic groups. The observed longitudinal increases in LOCC incidence, mortality, and DALYs since 1990 reflect complex interactions between demographic transitions, evolving lifestyle patterns, and the expanding prevalence of established risk factors, including tobacco consumption, alcohol use, and smoking.
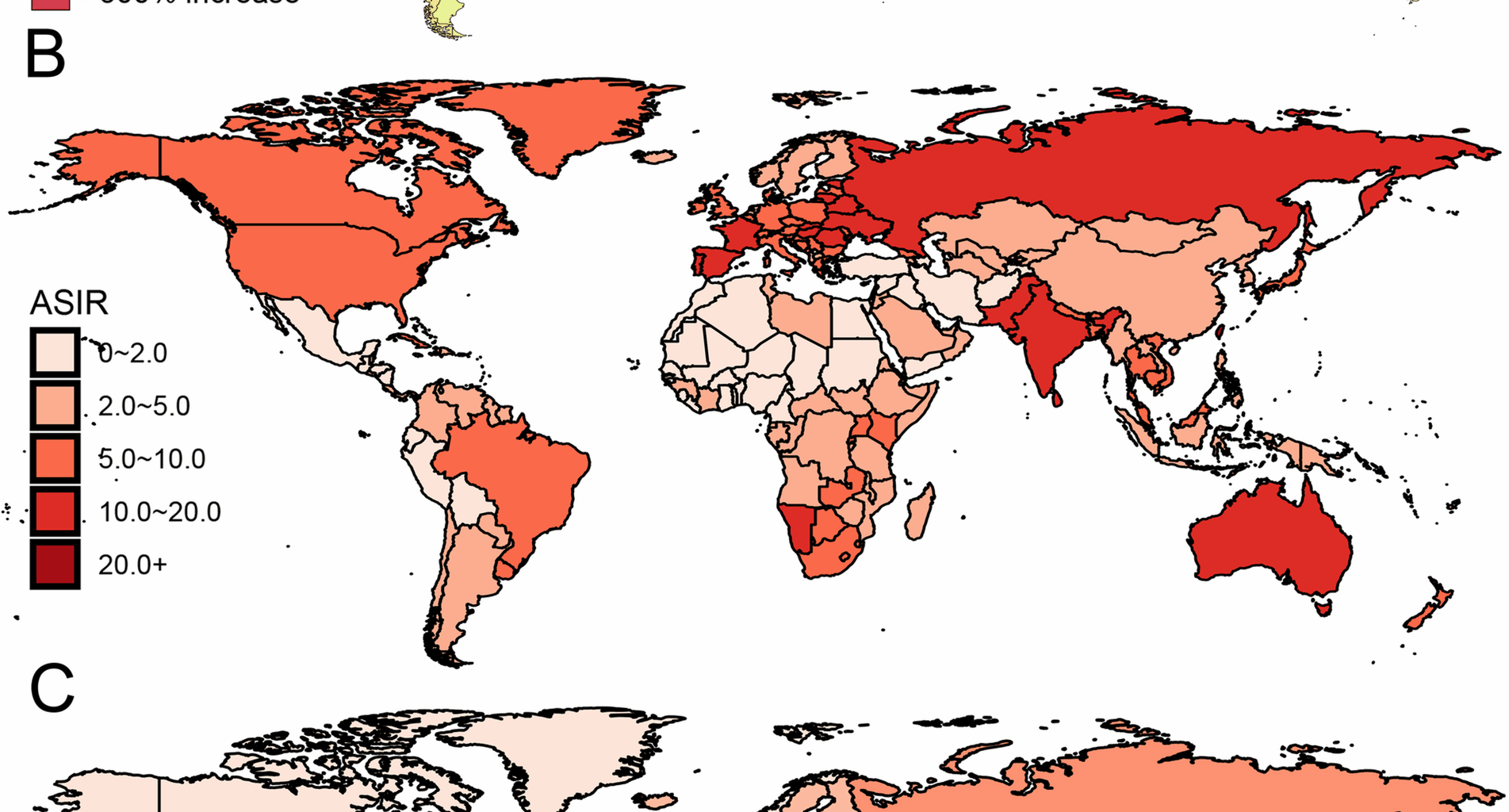
A salient finding emerges in the marked geographical heterogeneity of LOCC incidence. South Asia demonstrated the highest burden of new cases, followed by Eastern Europe, while Western Sub-Saharan Africa reported substantially lower incidence rates. The ASIR in South Asia (9.8) exceeded that of Western Sub-Saharan Africa (1.3) by nearly sevenfold. This pronounced disparity likely reflects multiple factors, including differential exposure to risk factors—particularly the prevalent practice of tobacco chewing in South Asia—and disparities in healthcare accessibility and early detection capabilities. The notably lower incidence rates in Western Sub-Saharan Africa may partially reflect limitations in diagnostic infrastructure and surveillance systems, potentially resulting in case underascertainment. Furthermore, significant sex-specific disparities were observed globally, with males exhibiting higher incidence rates (ASIR: 6.7) compared to females (ASIR: 3.3). This sexual dimorphism in LOCC incidence aligns with established patterns of risk factor exposure, particularly regarding tobacco and alcohol consumption, and may be further influenced by occupational exposures and healthcare utilization patterns [26].
Mortality patterns demonstrated significant regional variation, with South Asia bearing a disproportionate burden of LOCC-related deaths, concordant with its elevated incidence rates and consistent with previous epidemiological investigations [27, 28]. In contrast, North Africa and the Middle East exhibited markedly lower mortality rates, potentially attributable to variations in healthcare infrastructure, early detection protocols, and therapeutic interventions [29]. The relatively lower mortality burden in these regions may also reflect distinct patterns of tobacco consumption, characterized by lower prevalence rates compared to global averages [30]. Notably, certain geographical areas, including Cabo Verde and the Northern Mariana Islands, demonstrated concerning upward trajectories in mortality rates, highlighting emergent challenges in regions with limited oncological infrastructure. Conversely, nations such as Kuwait and Kyrgyzstan demonstrated sustained decreases in mortality, underscoring the potential impact of strengthened healthcare systems on disease outcomes.
The longitudinal analysis of global DALY trends revealed complex temporal patterns from 1990 to 2036, with notable inflection points. DALYs, as a composite metric incorporating both years of life lost due to premature mortality and years lived with disability, provide crucial insights into the comprehensive societal impact of LOCC [31]. Our projections indicate that the age-standardized DALY rate reached its apex in 2019 and is projected to demonstrate a declining trajectory through 2027, followed by a gradual resurgence. This pattern suggests that while mortality rates may show improvement, the chronic sequelae of LOCC—including treatment-related morbidity and metastatic complications—will continue to pose significant challenges to healthcare systems globally. The geographical distribution of DALYs exhibited substantial heterogeneity, reflecting both disease incidence patterns and healthcare system capabilities. South Asia’s elevated DALY burden corresponded with its high incidence rates, while regions such as Central Europe demonstrated more favorable DALY profiles, likely attributable to robust healthcare infrastructure and effective early detection programs [32].
A critical finding emerging from our analysis is the substantial attributable burden associated with modifiable risk factors, particularly smoking, alcohol use, and chewing tobacco. Our analysis indicates that smoking was the predominant risk factor, accounting for 23.4% of mortality and 22.3% of DALYs globally. Alcohol consumption and chewing tobacco demonstrated comparable contributions, responsible for 19.2% and 18.7% of deaths, and 20.3% and 18.8% of DALYs, respectively. These findings underscore the imperative for targeted public health interventions aimed at risk factor modification, particularly in high-burden regions. The relative contribution of these risk factors demonstrated marked regional variation. East Asia exhibited the highest smoking-attributable burden, with approximately 42.0% of both deaths and DALYs attributable to this risk factor, reflecting the persistent high smoking prevalence in countries such as China and Japan despite ongoing tobacco control initiatives [33]. Central Europe demonstrated a distinct pattern, with alcohol consumption emerging as the dominant risk factor, accounting for 37.8% of mortality and 40.8% of DALYs, suggesting strong sociocultural determinants of alcohol-related LOCC burden in this region [34]. South Asia’s unique risk factor profile was characterized by the substantial burden attributable to smokeless tobacco, contributing to 35.7% of deaths and 33.8% of DALYs, highlighting the critical need for region-specific interventions targeting culturally embedded tobacco use practices.
Despite increasing recognition of the importance of early detection and preventive strategies, significant challenges persist in mitigating the global LOCC burden. The observed disparities in disease metrics across regions reflect both inequitable distribution of healthcare resources and persistent exposure to established risk factors. Regions such as South Asia, characterized by high incidence and mortality rates, require comprehensive public health strategies encompassing prevention, early detection, and therapeutic interventions [35]. While tobacco control policies have demonstrated efficacy in certain contexts, additional targeted interventions are necessary to address the high prevalence of chewing tobacco in South Asia [36]. In regions reporting lower disease burden, such as Western Sub-Saharan Africa, strengthening surveillance infrastructure and cancer registry systems is paramount for accurate burden estimation. The current limitations in cancer registration systems in many low and low-middle income countries potentially result in burden underestimation and delayed intervention implementation. Enhancement of cancer registry infrastructure and diagnostic capabilities represents a critical priority for improved disease monitoring and outcomes optimization [37].
The increasing global burden of LOCC, particularly in low- and middle-SDI regions, underscores the urgent need for targeted public health interventions. These findings highlight the importance of scaling up preventive strategies such as anti-tobacco and alcohol reduction campaigns, early detection programs, and public awareness initiatives. Moreover, countries with high or rising AAPCs should consider integrating LOCC surveillance into broader cancer control plans to ensure timely diagnosis and equitable access to treatment. Policymakers can also use regional ASMR and ASDR trends to guide resource allocation and prioritize interventions tailored to the specific epidemiological context.
The findings of this study highlight several avenues for future research in LOCC. First, longitudinal cohort and molecular studies are needed to better understand the interaction between traditional risk factors—such as smoking, alcohol use, and chewing tobacco—and emerging factors like HPV infection and environmental exposures. Second, evaluation of the effectiveness of prevention and early detection programs in high-burden regions could provide evidence for scaling up context-specific interventions. Third, integration of novel technologies, including the Internet of Medical Things (IoMT) and AI-assisted screening, warrants exploration to enhance early diagnosis and surveillance in resource-limited settings. Finally, comparative projections using future GBD releases, such as GBD 2023, will be essential for validating these findings and monitoring progress toward global oral cancer control goals.
While our study provides comprehensive insights into the global, regional, and national LOCC burden, several methodological Limitations warrant acknowledgment. Primary among these is the reliance on GBD 2021 estimates, which, while robust, are subject to modeling assumptions that may not fully capture the complexity of LOCC epidemiology in certain contexts. Case under ascertainment, particularly in resource-limited settings with constrained healthcare infrastructure, may result in burden underestimation. Additionally, variations in diagnostic protocols, cancer classification systems, and healthcare accessibility may influence data accuracy. Future research priorities should include strengthening cancer registration systems in underrepresented regions and conducting robust population-based studies to refine burden estimates. Moreover, expanded investigation of genetic and environmental determinants of LOCC, particularly in high-burden regions, will be essential for developing targeted prevention and treatment strategies.