Weetman D, Kamgang B, Badolo A, Moyes CL, Shearer FM, Coulibaly M, et al. Aedes mosquitoes and Aedes-borne arboviruses in Africa: current and future threats. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15020220.
Garske T, Van Kerkhove MD, Yactayo S, Ronveaux O, Lewis RF, Staples JE, et al. Yellow fever in Africa: estimating the burden of disease and impact of mass vaccination from outbreak and serological data. PLoS Med. 2014;11:e1001638.
Jaenisch T, Junghanss T, Wills B, Brady OJ, Eckerle I, Farlow A, et al. Dengue expansion in Africa-not recognized or not happening? Emerg Infect Dis. 2014;20:e140487.
Chan M. Yellow fever: the resurgence of a forgotten disease. Lancet. 2016;387:2165–6.
Mattingly PF. Genetical aspects of the Aedes aegypti problem. I. Taxonom: and bionomics. Ann Trop Med Parasitol. 1957;51:392–408.
Moore M, Sylla M, Goss L, Burugu MW, Sang R, Kamau LW, et al. Dual African origins of global Aedes aegypti s.l. populations revealed by mitochondrial DNA. PLoS Negl Trop Dis. 2013;7:e2175.
Gubler DJ. Aedes albopictus in Africa. Lancet Infect Dis. 2003;3:751–2.
Longbottom J, Walekhwa AW, Mwingira V, Kijanga O, Mramba F, Lord JS. Aedes albopictus invasion across Africa: the time is now for cross-country collaboration and control. Lancet Glob Health. 2023;11:e623–8.
Braack L, Gouveia de Almeida AP, Cornel AJ, Swanepoel R, de Jager C. Mosquito-borne arboviruses of African origin: review of key viruses and vectors. Parasit Vectors. 2018;11:29.
Agboli E, Zahouli JBZ, Badolo A, Jöst H. Mosquito-associated viruses and their related mosquitoes in West Africa. Viruses. 2021;13:67.
Oxborough RM, Chilito KCF, Tokponnon F, Messenger LA. Malaria vector control in sub-Saharan Africa: complex trade-offs to combat the growing threat of insecticide resistance. Lancet Planet Health. 2024;8:e804–12.
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
Stoler J, Al Dashti R, Anto F, Fobil JN, Awandare GA. Deconstructing “malaria”: West Africa as the next front for dengue fever surveillance and control. Acta Trop. 2014;134:58–65.
Ahmed A, Ali Y, Mohamed NS. Arboviral diseases: the emergence of a major yet ignored public health threat in Africa. Lancet Planet Health. 2020;4:e555.
Buchwald AG, Hayden MH, Dadzie SK, Paull SH, Carlton EJ. Aedes-borne disease outbreaks in West Africa: a call for enhanced surveillance. Acta Trop. 2020;209:105468.
WHO. Strategic preparedness, readiness and response plan: dengue and other Aedes-borne arboviruses. Geneva: World Health Organization; 2024.
WHO. WHO African Region Health Emergency Situation Report. Multi-country outbreak of dengue. Regional Situation Report No. 06 with data as of 28 April 2024. 2024. https://iris.who.int/bitstream/handle/10665/376915/AFRO.Dengue.Sitrep006-20240428.pdf?sequence=1Accessed 3 May 2025.
Mordecai EA, Ryan SJ, Caldwell JM, Shah MM, LaBeaud AD. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet Health. 2020;4:e416–23.
Rose NH, Sylla M, Badolo A, Lutomiah J, Ayala D, Aribodor OB, et al. Climate and Urbanization Drive Mosquito Preference for Humans. Curr Biol. 2020;30:3570-3579.e3576.
Kolimenakis A, Heinz S, Wilson ML, Winkler V, Yakob L, Michaelakis A, et al. The role of urbanisation in the spread of Aedes mosquitoes and the diseases they transmit-a systematic review. PLoS Negl Trop Dis. 2021;15:e0009631.
Tatem AJ, Gething PW, Smith DL, Hay SI. Urbanization and the global malaria recession. Malar J. 2013;12:133.
Forsyth JE, Kempinsky A, Pitchik HO, Alberts CJ, Mutuku FM, Kibe L, et al. Larval source reduction with a purpose: designing and evaluating a household- and school-based intervention in coastal Kenya. PLoS Negl Trop Dis. 2022;16:e0010199.
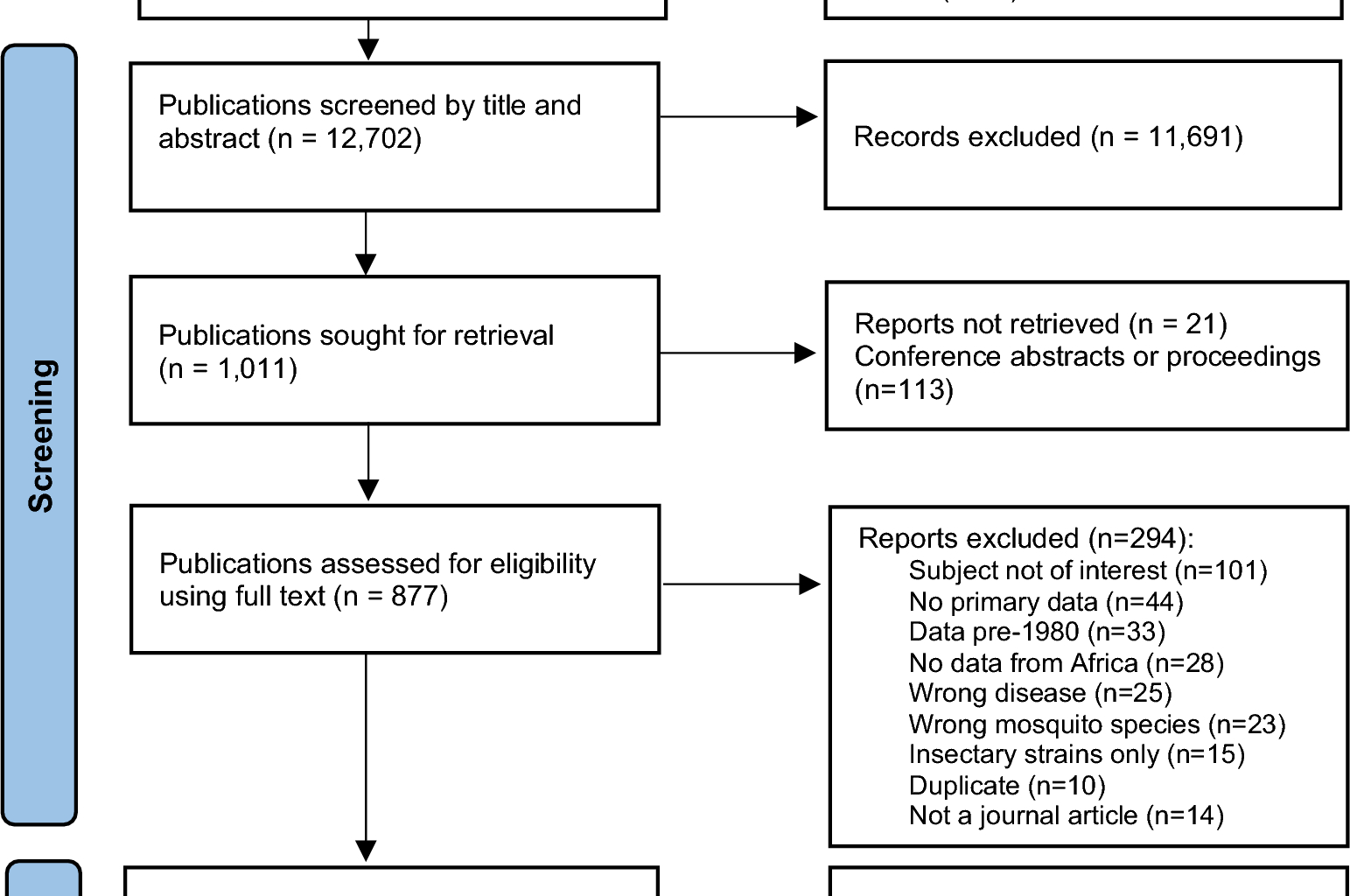
Kristan M, Messenger LA, Kamgang B, Biggs JR, Chan K, Emidi B, et al. Aedes in Africa: building resilience against the growing threat of arboviruses: a scoping review of Aedes vector surveillance, control strategies and insecticide resistance in Africa, a scoping review protocol. 2025. https://osf.io/vz5gh. Accessed 28 June 2025.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2002;8:58.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Falconer J, Kristan M. Search strategies for: “Building resilience against the growing threat of arboviruses (chikungunya, dengue, yellow fever, Zika); a scoping review of Aedes vector surveillance, control strategies and insecticide resistance monitoring in Africa.” London: LSHTM Data Compass; 2025.
Library, Archive & Open Research Services blog. Removing duplicates from an EndNote library. https://blogs.lshtm.ac.uk/library/2018/12/07/removing-duplicates-from-an-endnote-library/. Accessed 02 February 2025.
Ndiaye EH, Diallo D, Fall G, Ba Y, Faye O, Dia I, et al. Arboviruses isolated from the Barkedji mosquito-based surveillance system, 2012–2013. BMC Infect Dis. 2018;18:642.
Traoré-Lamizana M, Fontenille D, Zeller HG, Mondo M, Diallo M, Adam F, et al. Surveillance for yellow fever virus in eastern Senegal during 1993. J Med Entomol. 1996;33:760–5.
Boyer S, Foray C, Dehecq JS. Spatial and temporal heterogeneities of Aedes albopictus density in La Reunion Island: rise and weakness of entomological indices. PLoS ONE. 2014;9:e91170.
Dehecq J-S, Fohr G, Thiria J. Plan de lutte contre Aedes albopictus pendant l’épidémie de chikungunyaà La Réunion en 2005–2007. Bull Epidemiol Hebdomadaire. 2008; BEH thématique 38-39-40.
Fontenille D, Mathiot C, Rodhain F, Coulanges P. Arbovirus infections on the island of Nosy-Be; serologic and entomologic findings. Arch Inst Pasteur Madagascar. 1988;54:101–15.
Cordellier R, Bouchité B, Roche J-C, Monteny N, Diaco B, Akoliba P. Circulation selvatique du virus Dengue 2 en 1980, dans les savanes sub-soudaniennes de Côte d’Ivoire. Cah ORSTOM sér Ent méd et Parasitol. 1983; vol XXI, no.3, pg 165-179.
Jupp PG, Kemp A. Aedes albopictus and other mosquitoes imported in tires into Durban, South Africa. J Am Mosq Control Assoc. 1992;8:321–2.
Guarido MM, Govender K, Riddin MA, Schrama M, Gorsich EE, Brooke BD, et al. Detection of insect-specific flaviviruses in mosquitoes (Diptera. Viruses. 2021;13:456.
Gould LH, Osman MS, Farnon EC, Griffith KS, Godsey MS, Karch S, et al. An outbreak of yellow fever with concurrent chikungunya virus transmission in South Kordofan, Sudan, 2005. Trans R Soc Trop Med Hyg. 2008;102:1247–54.
Seidahmed OM, Siam HA, Soghaier MA, Abubakr M, Osman HA, Abd Elrhman LS, et al. Dengue vector control and surveillance during a major outbreak in a coastal Red Sea area in Sudan. East Mediterr Health J. 2012;18:1217–24.
Kemabonta KA, Anikwe JC, Adaezeobiora IB. Bioefficacy of Skeeter Abate and Spintor on Anopheles gambiae and Aedes aegypti mosquitoes from insecticide resistance areas in Lagos and Oyo States, Nigeria. J Biol Agric Healthc. 2013;3:546.
Derua YA, Tungu PK, Malima RC, Mwingira V, Kimambo AG, Batengana BM, et al. Laboratory and semi-field evaluation of the efficacy of Bacillus thuringiensis var. israelensis (Bactivec®) and Bacillus sphaericus (Griselesf®) for control of mosquito vectors in northeastern Tanzania. Curr Res Parasitol Vector Borne Dis. 2022;2:100089.
Logan TM, Linthicum KJ, Wagateh JN, Thande PC, Kamau CW, Roberts CR. Pretreatment of floodwater Aedes habitats (dambos) in Kenya with a sustained-release formulation of methoprene. J Am Mosq Control Assoc. 1990;6:736–8.
Nnakumusana ES. Susceptibility of mosquito larvae to Coelomomyces indicus. Indian J Med Res. 1985;82:316–20.
Nnakumusana E. Effects of temperature on the susceptibility of Aedes aegypti (L.) (Diptera: Culicidae) larvae to a mosquito pathogen Coelomomyces stegomyiae in Uganda. Appl Entomol Zool. 1987;22:7–12. https://doi.org/10.1303/aez.22.7.
Nnakumusana E. The pathogenicity of two isolates of Pythium spp. to mosquito larvae in the laboratory. Insect Sci Appl. 1987. https://doi.org/10.1017/S1742758400006883.
Nzelibe H, Albaba S. Larvicidal potential of Persea americana seed extract against Aedes vittatus mosquito. Curr J Appl Sci Technol. 2015;11:1–9.
Eze EA, Danga SP, Okoye FB. Larvicidal activity of the leaf extracts of Spondias mombin Linn. (Anacardiaceae) from various solvents against malarial, dengue and filarial vector mosquitoes (Diptera: Culicidae). J Vector Borne Dis. 2014;51:300–6.
Diallo D, Marston A, Terreaux C, Touré Y, Paulsen BS, Hostettmann K. Screening of Malian medicinal plants for antifungal, larvicidal, molluscicidal, antioxidant and radical scavenging activities. Phytother Res. 2001;15:401–6.
Fletcher M, Teklehaimanot A, Yemane G. Control of mosquito larvae in the port city of Assab by an indigenous larvivorous fish, Aphanius dispar. Acta Trop. 1992;52:155–66.
Sabatinelli G, Majori G. Utilisation de Poecilia reticulata dans la lutte contre le paludisme dans la R.F.I des Comores. Parassitologia. 1988;30:68.
Ouédraogo S, Benmarhnia T, Bonnet E, Somé PA, Barro AS, Kafando Y, et al. Evaluation of effectiveness of a community-based intervention for control of dengue virus vector, Ouagadougou, Burkina Faso. Emerg Infect Dis. 2018;24:1859–67.
Bonnet E, Fournet F, Benmarhnia T, Ouedraogo S, Dabiré R, Ridde V. Impact of a community-based intervention on Aedes aegypti and its spatial distribution in Ouagadougou, Burkina Faso. Infect Dis Poverty. 2020;9:61.
Badolo A, Ilboudo-Sanogo E, Ouédraogo AP, Costantini C. Evaluation of the sensitivity of Aedes aegypti and Anopheles gambiae complex mosquitoes to two insect repellents: DEET and KBR 3023. Trop Med Int Health. 2004;9:330–4.
Staikowsky F, Le Roux K, Schuffenecker I, Laurent P, Grivard P, Develay A, et al. Retrospective survey of Chikungunya disease in Réunion Island hospital staff. Epidemiol Infect. 2008;136:196–206.
Waldetensai A, Gemechu F, Kinfe E, Amare H, Hagos S, Teshome D, et al. Aedes mosquito responses to control interventionsagainst the Chikungunya outbreak of Dire Dawa, Eastern Ethiopia. Int J Trop Insect Sci. 2021. https://doi.org/10.1007/s42690-021-00430-w.
Yougang AP, Keumeni CR, Wilson-Bahun TA, Tedjou AN, Njiokou F, Wondji C, et al. Spatial distribution and insecticide resistance profile of Aedes aegypti and Aedes albopictus in Douala, the most important city of Cameroon. PLoS ONE. 2022;17:e0278779.
Toé HK, Zongo S, Guelbeogo MW, Kamgang B, Viana M, Tapsoba M, et al. Multiple insecticide resistance and first evidence of V410L kdr mutation in Aedes (Stegomyia) aegypti (Linnaeus) from Burkina Faso. Med Vet Entomol. 2022;36:309–19.
Mukhtar MM, Ibrahim SS. Temporal evaluation of insecticide resistance in populations of the major arboviral vector. Insects. 2022;13:23.
Kwame Amlalo G, Akorli J, Etornam Akyea-Bobi N, Sowa Akporh S, Aqua-Baidoo D, Opoku M, et al. Evidence of high frequencies of insecticide resistance mutations in Aedes aegypti (Culicidae) mosquitoes in urban Accra, Ghana: implications for insecticide-based vector control of Aedes-borne arboviral diseases. J Med Entomol. 2022;59:2090–101.
Lebon C, Alout H, Zafihita S, Dehecq JS, Weill M, Tortosa P, et al. Spatio-temporal dynamics of a dieldrin resistance gene in Aedes albopictus and Culex quinquefasciatus populations from Reunion Island. J Insect Sci. 2022;22:56.
Konan LY, Oumbouke WA, Silué UG, Coulibaly IZ, Ziogba JT, N’Guessan RK, et al. Insecticide resistance patterns and mechanisms in Aedes aegypti (diptera: culicidae) populations across Abidjan, Côte d’ivoire reveal emergent pyrethroid resistance. J Med Entomol. 2021;58:1808–16.
Kampango A, Hocke EF, Hansson H, Furu P, Haji KA, David JP, et al. High DDT resistance without apparent association to kdr and glutathione-S-transferase (GST) gene mutations in Aedes aegypti population at hotel compounds in Zanzibar. PLoS Negl Trop Dis. 2022;16:e0010355.
Sene NM, Mavridis K, Ndiaye EH, Diagne CT, Gaye A, Ngom EHM, et al. Insecticide resistance status and mechanisms in Aedes aegypti populations from Senegal. PLoS Negl Trop Dis. 2021;15:e0009393.
Pires S, Alves J, Dia I, Gómez LF. Susceptibility of mosquito vectors of the city of Praia, Cabo Verde, to temephos and Bacillus thuringiensis var israelensis. PLoS ONE. 2020;15:e0234242.
Pocquet N, Darriet F, Zumbo B, Milesi P, Thiria J, Bernard V, et al. Insecticide resistance in disease vectors from Mayotte: an opportunity for integrated vector management. Parasit Vectors. 2014;7:299.
Kudom AA. Entomological surveillance to assess potential outbreak of Aedes-borne arboviruses and insecticide resistance status of Aedes aegypti from Cape Coast, Ghana. Acta Trop. 2020;202:105257.
Yougang AP, Kamgang B, Tedjou AN, Wilson-Bahun TA, Njiokou F, Wondji CS. Nationwide profiling of insecticide resistance in Aedes albopictus (Diptera: Culicidae) in Cameroon. PLoS ONE. 2020;15:e0234572.
Montgomery M, Harwood JF, Yougang AP, Wilson-Bahun TA, Tedjou AN, Keumeni CR, et al. Spatial distribution of insecticide resistant populations of Aedes aegypti and Ae. albopictus and first detection of V410L mutation in Ae. aegypti from Cameroon. Infect Dis Poverty. 2022;11:90.
Kamgang B, Marcombe S, Chandre F, Nchoutpouen E, Nwane P, Etang J, et al. Insecticide susceptibility of Aedes aegypti and Aedes albopictus in Central Africa. Parasit Vectors. 2011;4:79.
Kamgang B, Yougang AP, Tchoupo M, Riveron JM, Wondji C. Temporal distribution and insecticide resistance profile of two major arbovirus vectors Aedes aegypti and Aedes albopictus in Yaoundé, the capital city of Cameroon. Parasit Vectors. 2017;10:469.
Tantely ML, Tortosa P, Alout H, Berticat C, Berthomieu A, Rutee A, et al. Insecticide resistance in Culex pipiens quinquefasciatus and Aedes albopictus mosquitoes from La Réunion Island. Insect Biochem Mol Biol. 2010;40:317–24.
Xu J, Bonizzoni M, Zhong D, Zhou G, Cai S, Li Y, et al. Multi-country survey revealed prevalent and novel F1534S mutation in voltage-gated sodium channel (VGSC) gene in Aedes albopictus. PLoS Negl Trop Dis. 2016;10:e0004696.
Ngoagouni C, Kamgang B, Brengues C, Yahouedo G, Paupy C, Nakoune E, et al. Susceptibility profile and metabolic mechanisms involved in Aedes aegypti and Aedes albopictus resistant to DDT and deltamethrin in the Central African Republic. Parasit Vectors. 2016;9:599.
WHO. Determining discriminating concentrations of insecticides for monitoring resistance in mosquitoes: report of a multi-centre laboratory study and WHO expert consultations. 2022. https://www.who.int/publications/i/item/9789240045200. Accessed 8 January 2025.
Ayres CFJ, Seixas G, Borrego S, Marques C, Monteiro I, Marques CS, et al. The V410L knockdown resistance mutation occurs in island and continental populations of Aedes aegypti in West and Central Africa. PLoS Negl Trop Dis. 2020;14:e0008216.
Yadouleton C, Tchibozo C, Azondekon R, Agbanrin R, Ahissou F, Houndeton A, et al. Pyrethroid resistance in Aedes aegypti populations in southern Benin, West Africa. Int J Mosquito Res. 2018;5:56.
Padonou G, Osse R, Salako A, Aikpon R, Sovi A, Kpanou C, et al. Entomological assessment of the risk of dengue outbreak in Abomey-Calavi Commune, Benin. Trop Med Health. 2020;48:20.
Badolo A, Sombié A, Pignatelli PM, Sanon A, Yaméogo F, Wangrawa DW, et al. Insecticide resistance levels and mechanisms in Aedes aegypti populations in and around Ouagadougou, Burkina Faso. PLoS Negl Trop Dis. 2019;13:e0007439.
Sombié A, Saiki E, Yaméogo F, Sakurai T, Shirozu T, Fukumoto S, et al. High frequencies of F1534C and V1016I. Trop Med Health. 2019;47:2.
Ouattara LPE, Sangaré I, Namountougou M, Hien A, Ouari A, Soma DD, et al. Surveys of arboviruses vectors in four cities stretching along a railway transect of Burkina Faso: risk transmission and insecticide susceptibility status of potential vectors. Front Vet Sci. 2019;6:140.
Namountougou M, Soma DD, Balboné M, Kaboré DA, Kientega M, Hien A, et al. Monitoring insecticide susceptibility in Aedes aegypti populations from the two biggest cities, Ouagadougou and Bobo-Dioulasso, in Burkina Faso: implication of metabolic resistance. Trop Med Infect Dis. 2020;5:59.
Yougang AP, Kamgang B, Bahun TAW, Tedjou AN, Nguiffo-Nguete D, Njiokou F, et al. First detection of F1534C knockdown resistance mutation in Aedes aegypti (Diptera: Culicidae) from Cameroon. Infect Dis Poverty. 2020;9:152.
Djiappi-Tchamen B, Nana-Ndjangwo MS, Mavridis K, Talipouo A, Nchoutpouen E, Makoudjou I, et al. Analyses of insecticide resistance genes in. Genes (Basel). 2021;12:56.
Kouadio A, Guindo-Coulibaly N, Adja A, Kpan S, Assouho K, Zoh D, et al. High density in dry season and resistance to pyrethroids of Aedes aegypti populations in Bouake, Cote d’Ivoire. Int J Trop Insect Sci. 2022;42:3395.
Mostafa A, Rashed M, Aly N, Hasan A, Mikhail M. Entomological surveillance of Aedes aegypti and arboviruses outbreak of Dengue fever in the Red Sea Governorate, Egypt. J Egypt Soc Parasitol. 2019. https://doi.org/10.21608/jesp.2019.68080.
Kawada H, Higa Y, Futami K, Muranami Y, Kawashima E, Osei JH, et al. Discovery of point mutations in the voltage-gated sodium channel from African Aedes aegypti populations: potential phylogenetic reasons for gene introgression. PLoS Negl Trop Dis. 2016;10:e0004780.
Owusu-Asenso CM, Mingle JAA, Weetman D, Afrane YA. Spatiotemporal distribution and insecticide resistance status of Aedes aegypti in Ghana. Parasit Vectors. 2022;15:61.
Kamgang B, Wilson-Bahun TA, Yougang AP, Lenga A, Wondji CS. Contrasting resistance patterns to type I and II pyrethroids in two major arbovirus vectors Aedes aegypti and Aedes albopictus in the Republic of the Congo, Central Africa. Infect Dis Poverty. 2020;9:23.
Fagbohun I, Idowu E, Olakiigbe A, Oyeniyi A, Otubanjo O, Awolola T. Metabolic resistance mechanism in Aedes aegypti from Lagos State, Nigeria. J Basic Appl Zool. 2020. https://doi.org/10.1186/s41936-020-00194-8.
Mathias L, Baraka V, Philbert A, Innocent E, Francis F, Nkwengulila G, et al. Habitat productivity and pyrethroid susceptibility status of Aedes aegypti mosquitoes in Dar es Salaam, Tanzania. Infect Dis Poverty. 2017;6:102.
WHO. Prequalification of medical products. Vector control products. 2023. https://extranet.who.int/prequal/vector-control-products. Accessed 20 January 2025.
WHO. Global arbovirus initiative; preparing for the next pandemic by tackling mosquito-borne viruses with epidemic and pandemic potential. Geneva: World Health Organization; 2024.
WHO. Framework for a national plan for monitoring and management of insecticide resistance in malaria vectors. Geneva: WHO. 2017. http://apps.who.int/iris/bitstream/handle/10665/254916/9789241512138-eng.pdf?sequence=1]
Dadzie SK, Akorli J, Coulibaly MB, Ahadji-Dabla KM, Baber I, Bobanga T, et al. Building the capacity of West African countries in Aedes surveillance: inaugural meeting of the West African Aedes Surveillance Network (WAASuN). Parasit Vectors. 2022;15:381.
Bowman LR, Donegan S, McCall PJ. Is dengue vector control deficient in effectiveness or evidence? Systematic review and meta-analysis. PLoS Negl Trop Dis. 2016;10:e0004551.
Lepore L, Vanlerberghe V, Verdonck K, Metelo E, Diallo M, Van Bortel W. Vector control for Aedes aegypti and Aedes albopictus mosquitoes implemented in the field in sub-Saharan Africa: a scoping review. PLoS Negl Trop Dis. 2025;19:e0013203.
McGregor BL, Connelly CR. A review of the control of Aedes aegypti (Diptera: Culicidae) in the continental United States. J Med Entomol. 2021;58:10–25.
Otshudiema JO, Diao WR, Ouedraogo SMW, Kapete AN, Moyenga L, Chanda E, et al. Estimating dengue outbreak thresholds in West Africa: a comprehensive analysis of climatic influences in Burkina Faso, 2018–2024. Trop Med Infect Dis. 2025. https://doi.org/10.3390/tropicalmed10030066.
Newby G, Chaki P, Latham M, Marrenjo D, Ochomo E, Nimmo D, et al. Larviciding for malaria control and elimination in Africa. Malar J. 2025;24:16.
Geissbühler Y, Kannady K, Chaki PP, Emidi B, Govella NJ, Mayagaya V, et al. Microbial larvicide application by a large-scale, community-based program reduces malaria infection prevalence in urban Dar es Salaam, Tanzania. PLoS ONE. 2009;4:e5107.
Antonio-Nkondjio C, Doumbe-Belisse P, Djamouko-Djonkam L, Ngadjeu CS, Talipouo A, Kopya E, et al. High efficacy of microbial larvicides for malaria vectors control in the city of Yaounde Cameroon following a cluster randomized trial. Sci Rep. 2021;11:17101.
Chaki PP, Govella NJ, Shoo B, Hemed A, Tanner M, Fillinger U, et al. Achieving high coverage of larval-stage mosquito surveillance: challenges for a community-based mosquito control programme in urban Dar es Salaam, Tanzania. Malar J. 2009;8:311.
Takken W, Lindsay S. Increased threat of urban malaria from Anopheles stephensi mosquitoes, Africa. Emerg Infect Dis. 2019;25:1431–3.
Hamlet A, Dengela D, Tongren JE, Tadesse FG, Bousema T, Sinka M, et al. The potential impact of Anopheles stephensi establishment on the transmission of Plasmodium falciparum in Ethiopia and prospective control measures. BMC Med. 2022;20:135.
Karch S, Asidi N, Manzambi Z, Salaun JJ, Mouchet J. Impact of deltamethrin-impregnated bednets on biting rates of mosquitoes in Zaire. J Am Mosq Control Assoc. 1995;11:191–4.
Trimmer JT, Qureshi H, Otoo M, Delaire C. The enabling environment for citywide water service provision: insights from six successful cities. PLoS Water. 2023. https://doi.org/10.1371/journal.pwat.0000071.
Morrison AC, Zielinski-Gutierrez E, Scott TW, Rosenberg R. Defining challenges and proposing solutions for control of the virus vector Aedes aegypti. PLoS Med. 2008;5:e68.
Aberese-Ako M, Doegah PT, Kpodo L, Ebelin W, Kuatewo M, Baba AA, et al. The role of community engagement toward ensuring healthy lives: a case study of COVID-19 management in two Ghanaian municipalities. Front Public Health. 2023;11:1213121.
Chen YA, Lai YT, Wu KC, Yen TY, Chen CY, Tsai KH. Using UPLC-MS/MS to evaluate the dissemination of pyriproxyfen by Aedes mosquitoes to combat cryptic larval habitats after source reduction in Kaohsiung in Southern Taiwan. Insects. 2020;11:26.
Sim S, Ng LC, Lindsay SW, Wilson AL. A greener vision for vector control: the example of the Singapore dengue control programme. PLoS Negl Trop Dis. 2020;14:e0008428.
Fox T, Sguassero Y, Chaplin M, Rose W, Doum D, Arevalo-Rodriguez I, et al. Wolbachia-carrying Aedes mosquitoes for preventing dengue infection. Cochrane Database Syst Rev. 2024;4:CD015636.
Morrison AC, Reiner RC, Elson WH, Astete H, Guevara C, Del Aguila C, et al. Efficacy of a spatial repellent for control of Aedes-borne virus transmission: a cluster-randomized trial in Iquitos, Peru. Proc Natl Acad Sci USA. 2022;119:e2118283119.
Patil PB, Dasgupta SK, Gorman K, Pickl-Herk A, Puinean M, McKemey A, et al. Elimination of a closed population of the yellow fever mosquito, Aedes aegypti, through releases of self-limiting male mosquitoes. PLoS Negl Trop Dis. 2022;16:e0010315.
Anderson MAE, Gonzalez E, Edgington MP, Ang JXD, Purusothaman DK, Shackleford L, et al. A multiplexed, confinable CRISPR/Cas9 gene drive can propagate in caged Aedes aegypti populations. Nat Commun. 2024;15:729.
Johnson BJ, Ritchie SA, Fonseca DM. The state of the art of lethal oviposition trap-based mass interventions for Arboviral control. Insects. 2017;8:56.
Utarini A, Indriani C, Ahmad RA, Tantowijoyo W, Arguni E, Ansari MR, et al. Efficacy of Wolbachia-infected mosquito deployments for the control of dengue. N Engl J Med. 2021;384:2177–86.
Mancini MV, Murdochy SM, Bilgo E, Ant TH, Gingell D, Gnambani EJ, et al. Wolbachia strain wAlbB shows favourable characteristics for dengue control use in Aedes aegypti from Burkina Faso. Environ Microbiol. 2024;26:e16588.
United Nations Environment Programme (UNEP). Ridding the world of POPs: a guide to the Stockholm Convention on persistent organic pollutants. 2010. http://www.pops.int/documents/guidance/beg_guide.pdf. Accessed 9 June 2023.
Che-Mendoza A, González-Olvera G, Medina-Barreiro A, Arisqueta-Chablé C, Bibiano-Marin W, Correa-Morales F, et al. Efficacy of targeted indoor residual spraying with the pyrrole insecticide chlorfenapyr against pyrethroid-resistant Aedes aegypti. PLoS Negl Trop Dis. 2021;15:e0009822.
Vazquez-Prokopec GM, Che-Mendoza A, Kirstein OD, Bibiano-Marin W, González-Olvera G, Medina-Barreiro A, et al. Preventive residual insecticide applications successfully controlled Aedes aegypti in Yucatan, Mexico. Sci Rep. 2022;12:21998.
Pan American Health Organization (PAHO). Manual for indoor residual spraying in urban areas for Aedes aegypti control. Washington, DC: PAHO; 2019.
Bonds JA. Ultra-low-volume space sprays in mosquito control: a critical review. Med Vet Entomol. 2012;26:121–30.
WHO. List of prequalified vector control products. https://extranet.who.int/prequal/vector-control-products/prequalified-product-list. Accessed 08 January 2025.
WHO. Pre-qualification of medical products, ReMoa-Tri. https://extranet.who.int/prequal/vector-control-products/remoa-tri. Accessed 31 March 2025.
Namias A, Jobe NB, Paaijmans KP, Huijben S. The need for practical insecticide-resistance guidelines to effectively inform mosquito-borne disease control programs. Elife. 2021;10:26.
Grunert R, Box E, Garrett K, Yabsley M, Cleveland C. Effects of temephos (Abate®), spinosad (Natular®), and diflubenzuron on the survival of cyclopoid copepods. Am J Trop Med Hyg. 2022;106:818–22.
Tetreau G, Stalinski R, David JP, Després L. Monitoring resistance to Bacillus thuringiensis subsp. israelensis in the field by performing bioassays with each Cry toxin separately. Mem Inst Oswaldo Cruz. 2013;108:894–900.
Kamgang B, Vazeille M, Tedjou A, Yougang AP, Wilson-Bahun TA, Mousson L, et al. Different populations of Aedes aegypti and Aedes albopictus (diptera: culicidae) from Central Africa are susceptible to Zika virus infection. PLoS Negl Trop Dis. 2020;14:e0008163.
Olusegun-Joseph T, Oboh M, Awoniyi A, Adebowale A, Agbaso M, Fagbohun I. Efficacy of piperonyl butoxide (PBO) synergist on pyrethroid and dichlorodiphenyl trichloroethane (DDT) resistant mosquitoes in Lekki, Lagos State Nigeria. Animal Res Int. 2020;17:3821–8.