Study design
This was a prospective cohort study conducted from August 1, 2023 to July 31, 2024. Enrolled patients were followed for up to 90 days after hospital discharge or until the end of the study period.
Study setting and population
This study was conducted in the ED of Jigme Dorji Wangchuck National Referral Hospital (JDWNRH), a tertiary care hospital in Bhutan. The ED operates 24 h a day and provides comprehensive emergency services across all age groups, including medical, surgical, trauma, obstetric, and pediatric emergencies. It functions as both a primary emergency care center for the Thimphu region and a national referral center, receiving cases from across the country.
As of July 31, 2024 the ED was staffed by a multidisciplinary team comprising three emergency physicians with Doctor of Medicine (MD) in Emergency Medicine, eight emergency medicine residents enrolled in a four-year MD training program, ten general duty medical officers with MBBS degree, 33 nurses with either diploma or bachelor’s degrees in nursing, and six Emergency Medical Responders (EMRs) holding diplomas in emergency medical response. Most clinical staff including- including physicians, nurses, and EMRs – have received certification in Advanced Cardiovascular Life Support (ACLS), Advanced Trauma Life Support (ATLS), and Pediatric Advanced Life Support (PALS).
Emergency medical services (EMS) are activated via the national EMS number (112). Upon activation, EMRs are dispatched to the scene accompanied by an ambulance. The ambulances are equipped with basic life support capabilities, including oxygen cylinders, but lack advanced life-support equipment. Based on caller information, EMRs may carry pre-packed emergency kits containing emergency medications (e.g., adrenaline, antihistamines, and hydrocortisone), intravenous crystalloids, airway adjuncts (including laryngeal mask airways) and defibrillators. Within their scope of practice, EMRs are authorized to administer emergency medications, provide salbutamol nebulization, initiate intravenous crystalloids, administer dextrose, and insert laryngeal mask airways. However, endotracheal intubation is currently outside their scope of practice.
On arrival at the ED, all patients are triaged using the World Health Organization – International Committee of the Red Cross (WHO – ICRC) integrated triage tool, which categorizes patients into red (critical), yellow (urgent) and green (non-urgent). Patients triaged as red are immediately moved to the resuscitation room for immediate assessment and management by the physician-led resuscitation team. Those triaged as yellow or green are managed in the acute care area. After initial evaluation and stabilization, patients requiring further care are admitted to appropriate hospital wards or intensive care units (ICUs) following consultation with the relevant specialty teams. This study included all patients who sustained OHCA, defined as the absence of circulation or a palpable pulse occurring outside the hospital setting. Patients who sustained cardiac arrest in the hospital premises but outside ED or in-patient department were also categorized as OHCA.
OHCA patients presented to the ED through two main pathways: (1) via EMS, with EMRs notifying the triage or the ED in advance; or (2) via private transportation, typically accompanied by family members. Upon arrival, triage nurses promptly assessed patients for the presence of a pulse. In the absence of a palpable pulse, a code blue was activated by triggering an alarm system that simultaneously alerted the resuscitation room and the on-duty code blue team. The patient was then immediately moved to the adjacent resuscitation room and managed according to existing resuscitation protocols.
Sampling and recruitment
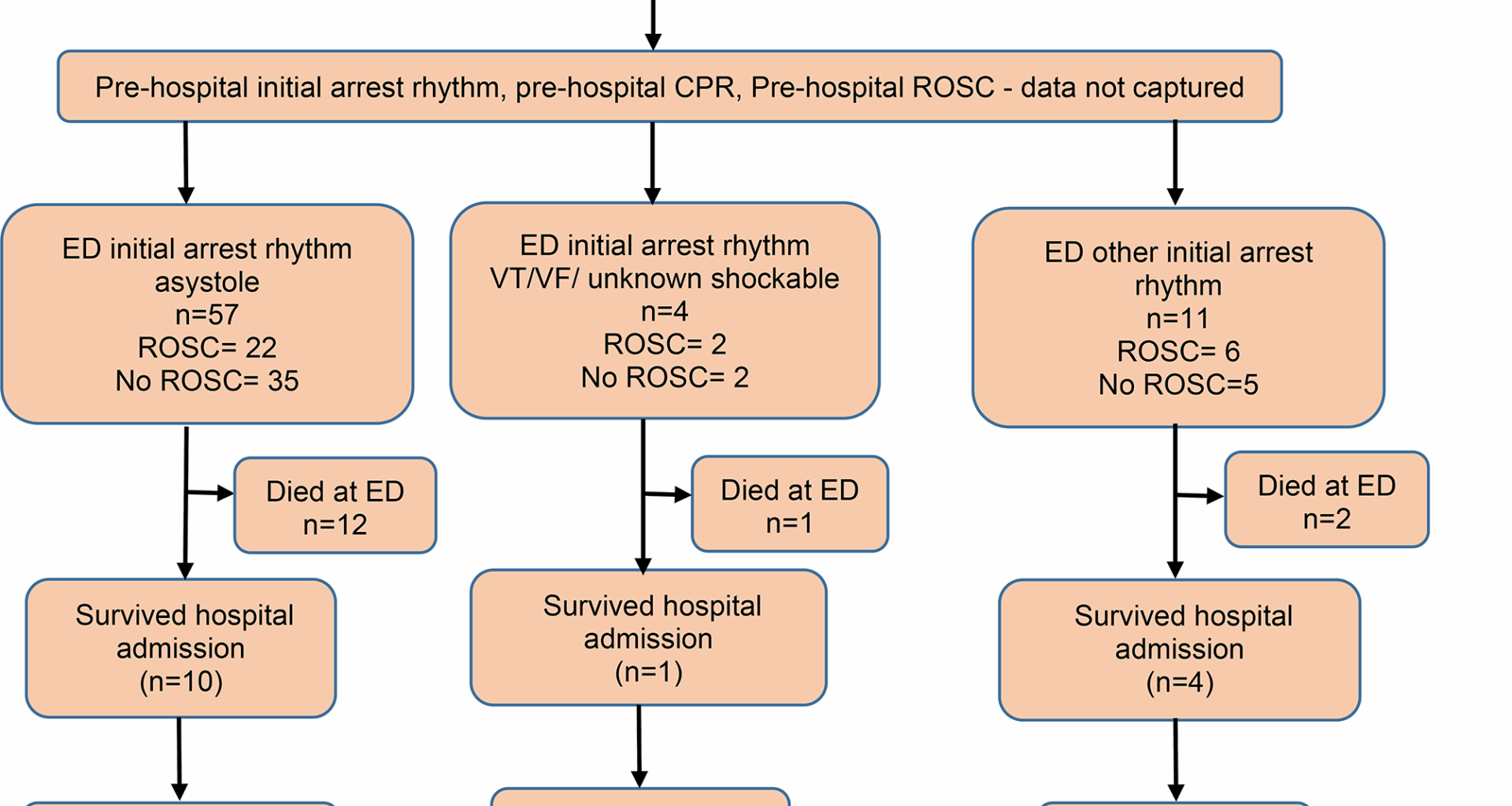
All patients presenting to the ED with OHCA who underwent resuscitation were included in the study. In 2023, the total number of ED visits was 42,665, and 94 OHCA cases were identified through the triage records. Patients who were not resuscitated, either due to physician discretion or family wishes were excluded. The study population included patients of all age groups, including neonates, pediatrics and pregnant women. A consecutive sampling method was used to ensure comprehensive inclusion of all eligible OHCA cases during the study period.
Upon arrival, OHCA patients were promptly resuscitated by the resuscitation team. Following the completion of resuscitation efforts, the team leader communicated the outcome to the patient’s family and, when applicable provided bereavement support. Enrollment in the study occurred after resuscitation was completed and bereavement support was offered.
Family members were then approached by the data collectors to obtain written informed consent for participation in the study. Written informed consent was obtained from immediate family members or legal guardians, including parents or guardians in the case of pediatric patients. Patients who achieved ROSC were admitted to the ICU, and followed up until hospital discharge, death, or up to 90 days post-discharge, with survival status recorded accordingly. Data collection was done by physicians, nurses, and the principal investigator provided they were not involved in the ED code blue response, typically while assigned to the acute medical care (AMC) unit. Clinical data were then obtained from treatment records and, where necessary through interview with family members.
Data collection
Data collection was done using a paper based case record form which was developed based on literature searches and the objectives of the study. Data was double entered into Epidata Version 3.1.
Data analysis
Data were double-entered and validated using EpiData (Version 3.1 for data entry and Version 2.2.2.183 for analysis, EpiData Association, Odense, Denmark). The validated datasets was then exported and analyzed using SPSS (Version 23). The Kolmogorov-Smirnov test was used to assess the normality of the study data. Normally distributed continuous variables, including demographic and clinical characteristics, were compared using a t-test. Non-normally distributed variables were analyzed using the Mann-Whitney test and expressed as medians with interquartile ranges (IQR). Categorical variables were analyzed using the Chi-square or Fisher’s exact test and presented as frequencies and percentages. Univariable and multivariable regression analysis was conducted to identify factors associated with favorable outcome after achieving ROSC in patient with OHCA. The odds ratio (OR) and 95% confidence interval were calculated to determine the strength of associations, with a p-value