If heat, irritants or toxins overstimulate the sensory neurons that detect them, some of these cells, called nociceptors, become desensitized or even die. Other nociceptors, however, survive the onslaught by downregulating components of the electron transport chain in their mitochondria, a new study shows.
“This is a very elegant story that combines ion channel biology with cell biology and also mitochondrial biology,” says Isaac Chiu, professor of immunology at Harvard Medical School, who was not involved in the work. It solves the mystery of how some nociceptors withstand a lifetime of noxious stimuli—a phenomenon familiar to almost every pain scientist, Chiu adds.
When a stimulus such as capsaicin, which is found in spicy peppers, activates a nociceptor, the cell transmits a signal to the spinal cord and then to the brain, where it registers as pain. At the molecular level, capsaicin binds an ion channel on the cell’s membrane called TRPV1, opening it and leading to an influx of calcium ions. David Julius, professor of physiology at University of California, San Francisco, and an investigator on the new study, received the 2021 Nobel Prize in Physiology or Medicine for the discovery of TRPV1.
“It was a huge, groundbreaking discovery because it started opening up our eyes to how nociceptors work,” Chiu says.
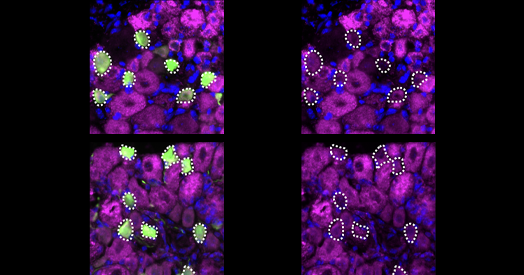
To understand what renders the cells susceptible or resilient to overstimulation, study investigator Lin Yuan, a postdoctoral fellow in Julius’ lab, conducted a genome-wide screen in human cell lines to pin down the responsible genes. The exercise identified components of the mitochondrial electron transport chain (ETC), which Yuan then manipulated by overexpressing them or knocking them out in cultured mouse sensory neurons from the dorsal root ganglia.
The results were “surprising,” Yuan says. Decreasing ETC activity, or genetically knocking down or knocking out elements of it, made nociceptors more resilient to capsaicin. “This is usually deleterious to cell health, but in this case, it’s actually protecting them against this type of toxicity,” Yuan says.
[Nociceptors] have tuned their electron transport chain to some sweet point where they can lower the risk of oxidative stress when they’re challenged by repetitive stimuli or very intense stimuli.
—
—
David Julius
In typical sensory neurons, capsaicin stimulation causes not only an influx of calcium ions but also a spike in mitochondrial reactive oxygen species (ROS), the researchers found. Knocking down ETC components in a cell lowered the calcium influx and attenuated the ROS increase. Together, the findings indicated that ROS from the ETC were a source of injury, and that stifling their production could also reduce cell damage and death.
And, compared with other sensory neurons, those that express TRPV1 have less activity in their electron transport chain at a steady state, Yuan found. These TRPV1-expressing neurons are also more resilient to death than other sensory neurons. She and her colleagues published their results in August in Cell.
T
he findings indicate that these neurons have adjusted their ETC and metabolic program to balance the onslaught of noxious events against the fact that they have axons that can be meters long and need some amount of metabolic activity to function, Julius says. “They’ve tuned their ETC to some sweet point where they can lower the risk of oxidative stress when they’re challenged by repetitive stimuli or very intense stimuli. And yet they can maintain enough of a mitochondrial function to support all the energetic needs that they have.”
Many neuronal cell types may modulate the activity of their mitochondrial ETC not just to meet metabolic demands, but to manage excitotoxicity, says Kivanç Birsoy, associate professor of metabolic regulation and genetics at Rockefeller University, who was not involved in the new study.
One of the open questions Julius and Yuan say they are working to understand is how the set point for mitochondrial function in different cell types is determined: “How much tuning is there of this mitochondrial function as you go from one cell type to another in the body? And how flexible is it? What’s the range of that in different cells across physiology?” Julius says.
Just as these mechanisms for resilience are likely used in different cell types, the specialized mechanisms by which cells die from excitotoxicity might be more general, too, Chiu says. “It could be that anything that causes a large influx of calcium could lead to this ROS-mediated cell death.”
Another open question is how the survival or death of sensory neurons is connected to sensing pain. Nociceptor death can lead to loss of pain. An ongoing clinical trial is testing the use of resiniferatoxin, a toxin about a thousand times more potent than capsaicin for treating pain, to kill nociceptors in joints to alleviate arthritis symptoms, Chiu says. But in some cases, such as diabetes or chemotherapy-induced neuropathy, nerve injury or death can lead to chronic pain.
“There’s a lot of interest in how nerves die, and the consequences of that,” Chiu says. “Understanding what regulates the health of nociceptors is quite important.”