Model performance and validation
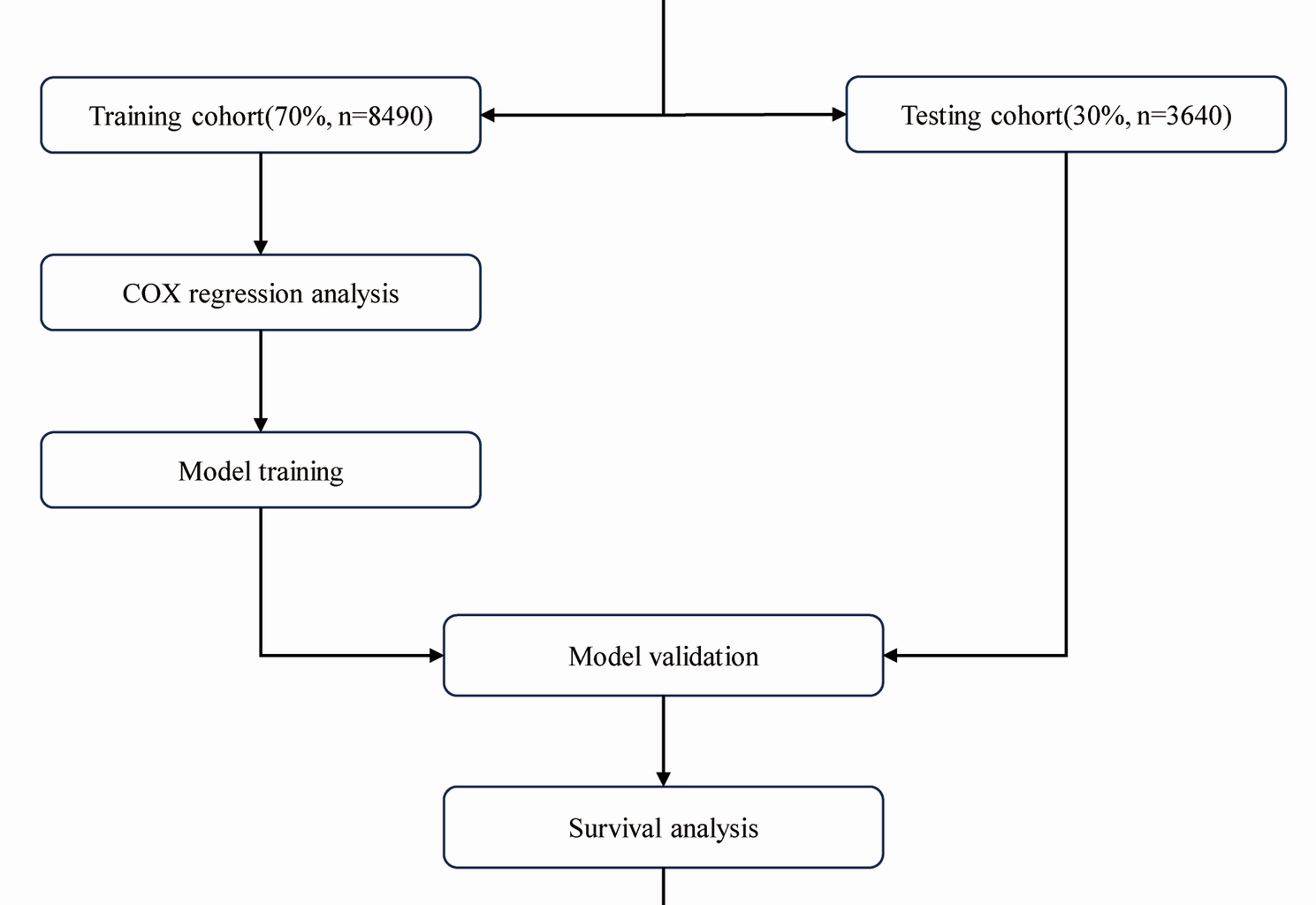
Our study provides comprehensive insights into the survival outcomes of AF patients during their first ICU admission, leveraging the extensive data from the MIMIC-IV database. The findings underscore the critical role of PersAF in significantly elevating the risk of all-cause mortality, as compared to PAF. Through rigorous statistical analysis, we identified independent predictors of 90-day mortality, including age, type of AF, and the presence of comorbidities such as cerebral infarction, intracranial injury, CHF, AKF, severe sepsis, cardiogenic shock, ARDS, malignant neoplasm, and ARF. Notably, the use of antiplatelet therapy and anticoagulants emerged as protective factors, associated with reduced mortality risk. A key contribution of our study lies in the development and validation of a comprehensive prediction model designed to assess 30, 60, and 90-day survival probabilities for AF patients admitted to the ICU. Our nomogram, which integrates a wide array of demographic, clinical, and treatment-related factors, exhibits outstanding discriminatory performance, with an area under the ROC curve AUC ranging between 0.80 and 0.84. This level of precision is on par with, and sometimes even surpasses, other established risk prediction tools tailored for AF patients.
Comparison with existing studies
Our model builds upon and extends the existing literature, such as the work by Verhaeghe, J., et al. [7], who emphasized the importance of generalizable and calibrated machine learning models for real-time AF risk prediction in ICU patients. Similar to the approach taken by Verhaeghe, J., et al., we assessed the calibration of our model’s predicted probabilities using Expected Calibration Error (ECE) and Expected Signed Calibration Error (ESCE) metrics. Our model demonstrated good calibration, indicating that the predicted risks closely align with the actual outcomes.
One of the key strengths of our model lies in its comparison with established risk scores such as CHA2DS2-VASc and HAS-BLED. Similar to the findings of Fox et al. [8] in their study of the GARFIELD-AF risk tool, our model outperformed CHA2DS2-VASc in predicting all-cause mortality. This finding highlights the importance of considering a broader spectrum of risk factors beyond those included in traditional scores. Moreover, by incorporating the effect of oral anticoagulation (OAC) therapy, our model aligns with the GARFIELD-AF risk tool in enabling clinicians to make informed decisions regarding anticoagulation strategies, which is crucial for optimizing patient outcomes.
Our model integrates 11 independent predictors, including ICU-specific critical conditions (e.g., AKF, ARDS, malignant neoplasm) that were rarely incorporated in prior AF prognostic models (e.g., Chen et al., 2021, which focused on post-discharge mortality and excluded ICU-specific comorbidities). For example, we identified AKF as a strong predictor (adjusted HR = 1.79, 95%CI 1.59–2.01), a finding specific to ICU settings where renal dysfunction rapidly exacerbates AF-related mortality [9]. Our nomogram aligns with existing literature, including Chen et al.‘s emphasis on the adverse prognosis associated with persistent AF [9] and Wang et al.‘s predictive nomogram for in-hospital mortality in AF patients in the ICU [10].
Similar to other studies, we identified age, comorbidities, and clinical indices such as SAPSII, RDW, and urine output as important predictors of in-hospital mortality in patients with coexisting heart failure (HF) and AF [11]. These factors have consistently been shown to be associated with poor prognosis in both HF and AF patients, aligning with previous research that indicates the combination of HF and AF poses a significant risk for increased mortality. For instance, a study by Guan et al. [12] identified several risk factors for 1-year mortality in this patient population, including age, sex, New York Heart Association (NYHA) cardiac function class, history of myocardial infarction, and laboratory parameters such as albumin, triglycerides, N-terminal pro-B-type natriuretic peptide (NT-proBNP), and blood urea nitrogen (BUN) levels. Our model included age, sex, NYHA class III or IV, history of myocardial infarction, and these same laboratory markers, underscoring their consistent prognostic value. Similar to the study by Yan et al. [11], which used both internal and external validation sets to validate their prediction model, our comprehensive validation strategy ensures that our model is not overfitted to a specific dataset.
Our study, in conjunction with the findings of Paludan-Müller et al. [13], emphasizes the pivotal role of age at diagnosis in predicting the prognosis of AF patients. Younger patients with AF exhibit disproportionately higher hazard ratios for cardiovascular events and mortality compared to older counterparts, echoing the nationwide cohort study by Paludan-Müller et al., which reported hazard ratios of 8.90 for cardiomyopathy, 8.64 for heart failure, 2.18 for ischaemic stroke, and 2.74 for mortality in individuals ≤ 50 years old. These results underscore the particularly detrimental effects of early-onset AF, associated with shortened life expectancy and increased morbidity, with an estimated average loss of 9.2 life years among those ≤ 50 years. In parallel, Li et al. [14] reported a significant global increase in the burden of AF/AFL over the past three decades, particularly affecting older populations and women, and highlighted an upward trend in low-middle and low sociodemographic index (SDI) regions despite overall decreasing global net drift mortality. This trend, coupled with identified risk factors such as high body mass index, hypertension, smoking, alcohol consumption in developed countries, and lead exposure in developing regions, underscores the multifaceted nature of AF/AFL and the urgent need for comprehensive, risk-differentiated, and cost-effective management strategies to address inequities and treatment gaps across different socioeconomic strata.
An interesting parallel emerges from the genetic risk score study by Ebana Y et al., which pinpointed eight genetic variants linked to the risk of CI in AF patients [15]. Although traditional risk scores like CHADS2 and CHA2DS2-VASc are commonly employed to gauge stroke risk in AF patients, Ebana et al. revealed that their genetic risk score (GRS) independently correlated with CI risk, emphasizing the potential role of genetic factors in enhancing risk stratification. This underscores the necessity for timely management strategies to prevent AF progression and related complications, as genetic variants may help identify high-risk AF patients, paving the way for more personalized and targeted interventions. These findings resonate with those of Ivănescu et al. [16], who conducted a thorough review on the utility of stroke risk scores in predicting severe outcomes in AF patients. Both studies highlight that elevated CHADS2 and CHA2DS2-VASc scores are associated with increased mortality rates, confirming their utility in pinpointing patients at higher risk for all-cause death. While Ivănescu et al. explored the broader application of these scores beyond thromboembolic risk assessment, our study delved into their implications within the ICU setting, where the complex interplay of multiple comorbidities and critical illnesses markedly influences patient outcomes.
Our findings are consistent with those reported by Hussain et al. [17], who investigated the timing of AF diagnosis in oncology patients and its impact on mortality, alongside the CHA2DS2-VASc score and cancer therapeutics. Hussain et al. [17] noted that the initial diagnosis of AF in cancer patients often occurred at or shortly after cancer diagnosis, especially in older patients and those receiving cardiotoxic treatments. Importantly, pre-existing AF or a diagnosis within three years of cancer diagnosis was associated with a poor prognosis, with AF diagnosis significantly linked to death during this ‘early phase’. Conversely, the CHA2DS2-VASc score, used for stroke risk stratification in AF patients, was only associated with mortality in the ‘late phase’, beyond three years after cancer diagnosis. In agreement, a nationwide Dutch study by Chen et al. [18] also found that concurrent AF and cancer adversely affected survival outcomes, highlighting the bidirectional association between AF and cancer, as well as variations in AF risk across different cancer types. Additionally, our results are corroborated by a nationwide population-based study by Jakobsen et al. [19], which revealed an elevated incidence of AF across all major cancer subtypes, suggesting a potential connection between malignancy and AF development.
Despite our cohort spanning 2008–2019, the fundamental ICU management principles for atrial fibrillation—stroke-preventive anticoagulation and haemodynamically guided rate control—remain unchanged in the 2022 ESC and 2023 AHA/ACC/HRS guidelines, and earlier data (Jamal et al., 2004–2014) already linked AF subtypes to ICU mortality [20]. Extending these observations, we demonstrate that among ARDS patients AF is an independent marker of multi-organ vulnerability: although adjusted all-cause mortality did not differ significantly, AF conferred heightened odds of acute myocardial infarction, cardiogenic shock, vasopressor dependence, acute kidney injury, permanent pacemaker placement, cardiac arrest and mechanical circulatory support, coinciding with a heavier comorbidity burden. Collectively, the evidence mandates systematic risk stratification and aggressive, guideline-concordant intervention for AF complicating critical illness, while mechanistic studies and targeted therapeutics are warranted to interrupt the AF–ARDS adverse-outcome axis.
Consistent with the study by Schupp et al. [21], which examined the prognostic impact of preexisting and new-onset AF in patients with septic or cardiogenic shock, we found no significant association between the presence of AF (either preexisting or new-onset) and 30-day all-cause mortality in our broader cohort of critically ill AF patients. However, our study extended the analysis to 90-day mortality and identified independent predictors that include age, type of AF, and the presence of comorbidities such as cerebral infarction, intracranial injury, CHF, AKF, severe sepsis, cardiogenic shock, ARDS, malignant neoplasm, and ARF.
Consistent with prior research, such as the study by Wang G et al., which reported an AKF incidence of 8.0% among AF patients [22]. The observed association between AKF and an increased risk of major adverse cardiovascular events underscores its prognostic significance in AF patients. Furthermore, the retrospective study by Bo et al. [23] demonstrates that AKF in AF patients is associated with a higher risk of mortality, but also reveals a potential benefit of oral anticoagulation therapy (OACs) in reducing 30-day mortality, despite a prolonged length of stay in both the hospital and ICU. These findings emphasize the critical role of clinicians in vigilant monitoring of renal function and early recognition and management of AKF in AF patients, particularly those in critical care settings. Appropriate anticoagulation therapy, balanced against the potential for bleeding complications and considering individual patient characteristics, may play a pivotal role in improving outcomes for these vulnerable patients [23].
We confirmed that antiplatelet therapy (adjusted HR = 0.65, 95%CI 0.55–0.77) and anticoagulants (adjusted HR = 0.78, 95%CI 0.70–0.88) are protective factors in ICU AF patients—this validates the clinical utility of these therapies in critically ill populations, whereas most prior studies (e.g., Ge et al., 2024) only explored their effects in non-ICU sepsis patients [24]. Despite the potential for an increased length of stay in the ICU and hospital, the improvement in survival underscores the clinical value of OACs in this context, possibly due to their mitigation of systemic clotting activation associated with sepsis, thereby reducing the risk of adverse cardiovascular events. Consistent with previous research, our findings reinforce the crucial role of anticoagulation therapy in improving survival outcomes in AF patients, as evidenced by the study by Calderon et al. [25], which found that new oral anticoagulants (NOACs) offered significant protection against stroke and all-cause mortality compared to vitamin K antagonists (VKAs) and untreated patients. The findings from the systematic review and meta-analysis by Benz et al. [26] align with our observations, emphasizing that antiplatelet therapy may modestly reduce stroke risk in AF patients not receiving oral anticoagulation. This underscores the importance of a thorough risk-benefit assessment when prescribing antiplatelet therapy in AF patients, particularly considering their overall treatment regimen and comorbidities.
Consistent with the findings of Camm et al. [27] and the growing body of evidence, our study, which analyzed the survival outcomes of AF patients during their first ICU admission using the MIMIC-IV database, adds support to the increasing role of rhythm control in AF management. Despite the historical focus on rate control, early rhythm control using safe and effective therapies, such as antiarrhythmic drugs and AF ablation, is increasingly recognized for its potential to reduce adverse cardiovascular outcomes, including AF-related deaths, heart failure, and strokes. Our findings align with the EARLY-AF trial by Kirchhof et al. [28], demonstrating that early rhythm-control therapy was associated with a lower risk of adverse cardiovascular outcomes among patients with early AF and cardiovascular conditions. Furthermore, consistent with Ravi et al.‘s [29] results, which showed a significant reduction in all-cause mortality with catheter ablation compared to medical therapy alone, our analysis also found that PersAF significantly increases the risk of all-cause mortality. Additionally, echoing Akerström et al.‘s findings [13], our study revealed that catheter ablation was associated with a significant reduction in the risk of all-cause mortality and stroke, with a reported 42% lower risk of the composite endpoint of all-cause mortality or stroke in patients undergoing catheter ablation compared to medically managed patients. Our study similarly demonstrated the heightened risk of all-cause mortality with PersAF and suggested that catheter ablation, among other therapeutic strategies, may contribute to improving survival outcomes in this high-risk population.
Limitations and future directions
A critical limitation of the present model is its derivation from retrospectively extracted MIMIC-IV data confined to a single academic centre, which not only restricts generalisability to community hospitals but also precludes prospective validation with real-time, longitudinal information that captures the full spectrum of dynamic clinical trajectories during ICU stay. The baseline-only feature set further undermines performance by ignoring time-varying physiology, genomic determinants of AF susceptibility, and procedural interventions such as catheter ablation or antiarrhythmic drug use—elements increasingly recognised as essential for accurate risk stratification and individualised therapy. Consequently, the absence of AF-specific treatment data prevents us from evaluating their impact on mortality. Although planned external validation in the multi-centre eICU Collaborative Research Database and the MIMIC-IV extension cohort will partly address geographic representativeness, translation into a robust precision-medicine tool will require integration of electronic health record free-text data (e.g., procedure notes) to extract ablation or drug exposure histories, prospective streaming physiologic data, and genomic profiling.