Simonsen C, Sundet K, Vaskinn A, Birkenaes AB, Engh JA, Færden A, et al. Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophr Bull. 2011;37(1):73–83.
Li Z, Liu L, Lin W, Zhou Y, Zhang G, Du X, et al. NRG3 contributes to cognitive deficits in chronic patients with schizophrenia. Schizophr Res. 2020;215:134–39.
Su Y, Yang L, Li Z, Wang W, Xing M, Fang Y, et al. The interaction of ASAH1 and NGF gene involving in neurotrophin signaling pathway contributes to schizophrenia susceptibility and psychopathology. Prog Neuropsychopharmacol Biol Psychiatry. 2021;104:110015.
Zhu S, Zhao L, Fan Y, Lv Q, Wu KLang X, et al. Interaction between TNF-α and oxidative stress status in first-episode drug-naïve schizophrenia. Psychoneuroendocrino. 2020;114:104595.
Comparelli A, Corigliano V, De Carolis A, Mancinelli I, Trovini G, Ottavi G, et al. Emotion recognition impairment is present early and is stable throughout the course of schizophrenia. Schizophr Res. 2013;143(1):65–69.
Owen MJ, Sawa A. Mortensen pb. Schizophr Lancet. 2016;388:86–97.
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013. A systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800.
Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry. 2007;64(2):242–49.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–31.
Reininghaus U, Dutta R, Dazzan P, Doody GA, Fearon P, Lappin J, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ӔSOP first-episode cohort. Schizophr Bull. 2015;41(3):664–73.
Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ-Brit Med J. 2013;346.
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–41.
Shen Y. Shen YuCun’s Psychiatry.: The People’s Health Press; 2018.
Mohamud WNW, Ismail AA, Sharifuddin A, Ismail IS, Musa KI, Kadir KA, et al. Prevalence of metabolic syndrome and its risk factors in adult Malaysians: results of a nationwide survey. Diabetes Res Clin Pr. 2011;91(2):239–45.
Ösby U, Correia N, Brandt L, Ekbom A, Sparén P. Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophr Res. 2000;45(1–2):21–28.
Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders-a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):306–18.
Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T, et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatr. 2009;14(4):359–75.
Bhargava A. A longitudinal analysis of the risk factors for diabetes and coronary heart disease in the framingham offspring study. Popul Health Metr. 2003;1:1–10.
Arango C, Bobes J, Aranda P, Carmena R, Garcia-Garcia M, Rejas J, et al. A comparison of schizophrenia outpatients treated with antipsychotics with and without metabolic syndrome: findings from the CLAMORS study. Schizophr Res. 2008;104(1–3):1–12.
Challa F, Getahun T, Sileshi M, Geto Z, Kelkile TS, Gurmessa S, et al. Prevalence of metabolic syndrome among patients with schizophrenia in Ethiopia. BMC Psychiatry. 2021;21:1–9.
Sun Y, Lu Y, Xing M, Zhu L, Lu W. New developments in the study of schizophrenia with metabolic syndrome. Shanghai M ed J. 2022;45(1):60–64.
Lee NY, Kim SH, Jung DC, Kim EY, Yu HY, Sung KH, et al. The prevalence of metabolic syndrome in Korean patients with schizophrenia receiving a monotherapy with aripiprazole, olanzapine or risperidone. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(5):1273–78.
Sugai T, Suzuki Y, Yamazaki M, Shimoda K, Mori T, Ozeki Y, et al. High prevalence of obesity, hypertension, hyperlipidemia, and diabetes mellitus in Japanese outpatients with schizophrenia: a nationwide survey. PLoS One. 2016;11(11):e166429.
Coccurello R, Moles A. Potential mechanisms of atypical antipsychotic-induced metabolic derangement: clues for understanding obesity and novel drug design. Pharmacol Ther. 2010;127(3):210–51.
Carlson C, Hornbuckle K, DeLisle F, Kryzhanovskaya L, Breier A, Cavazzoni P. Diabetes mellitus and antipsychotic treatment in the United Kingdom. Eur Neuropsychopharm. 2006;16(5):366–75.
Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease-a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. 2014;5:137.
De Hert M, Detraux J, Van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2012;8(2):114–26.
Khalil RB. Metabolic syndrome in patients with schizophrenia independently from atypical antipsychotics intake. Presse Med (Paris, France: 1983). 2012;41(5):e238–43.
Emul M, Kalelioglu T. Etiology of cardiovascular disease in patients with schizophrenia: current perspectives. Neuropsych Dis Treat. 2015;2493–503.
Yan J, Chen Y, Ju P, Gao J, Zhang L, Li J, et al. Network association of biochemical and inflammatory abnormalities with psychiatric symptoms in first-episode schizophrenia patients. Front Psychiatry. 2022;13:834539.
Zhai D, Cui T, Xu Y, Feng Y, Wang XYang Y, et al. Cardiometabolic risk in first-episode schizophrenia (FES) patients with the earliest stages of both illness and antipsychotic treatment. Schizophr Res. 2017;179:41–49.
Fleischhacker WW, Siu CO, Bodén R, Pappadopulos E, Karayal ON, Kahn RS, et al. Metabolic risk factors in first-episode schizophrenia: baseline prevalence and course analysed from the European first-episode schizophrenia trial. Int J Neuropsychoph. 2013;16(5):987–95.
Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14(3):339–47.
De Hert MA, van Winkel R, Van Eyck D, Hanssens L, Wampers M, Scheen A, et al. Prevalence of the metabolic syndrome in patients with schizophrenia treated with antipsychotic medication. Schizophr Res. 2006;83(1):87–93.
Heiskanen T, Niskanen L, Lyytikainen R, Saarinen PI, Hintikka J. Metabolic syndrome in patients with schizophrenia. J Clin Psychiat. 2003;64(5):575–79.
Ganesh S, Ashok AH, Kumar CN, Thirthalli J. Prevalence and determinants of metabolic syndrome in patients with schizophrenia: a systematic review and meta-analysis of Indian studies. Asian J Psychiatr. 2016;22:86–92.
Shojaeimotlagh V, Hashiehbaf A, Karami M, Monjazebi F, Gheshlagh RG. Prevalence of metabolic syndrome in Iranian patients with schizophrenia: a systematic review and meta-analysis. Diabetes Metabolic Syndr: Clin Res Rev. 2019;13(1):143–47.
Roshdy R. Prevalence of metabolic syndrome in patients with schizophrenia. Middle East Curr Psychiatry. 2011;18(2):109–17.
Chen L, Yang GG, Zhang XL, Fu WH. Investigation of metabolic syndrome in long-term schizophrenic inpatients. J Clin Psychiat. 2011;21(4):272–73.
Chen J, Rao D, Wang C. Obesity and metabolic problems in long-stay schizophrenic inpatients. Guangzhou Med J. 2010;41(4):9–12.
Yang K. A study related to concomitant metabolic syndrome in hospitalised schizophrenic patients. The 13th National Academic Conference on Integrated Chinese and Western Medicine for Psychiatric Diseases. Changchun, Jilin, China: 2014.
Lang X, Liu Q, Fang H, Zhou Y, Forster MT, Li Z, et al. The prevalence and clinical correlates of metabolic syndrome and cardiometabolic alterations in 430 drug-naive patients in their first episode of schizophrenia. Psychopharmacology. 2021;238(12):3643–52.
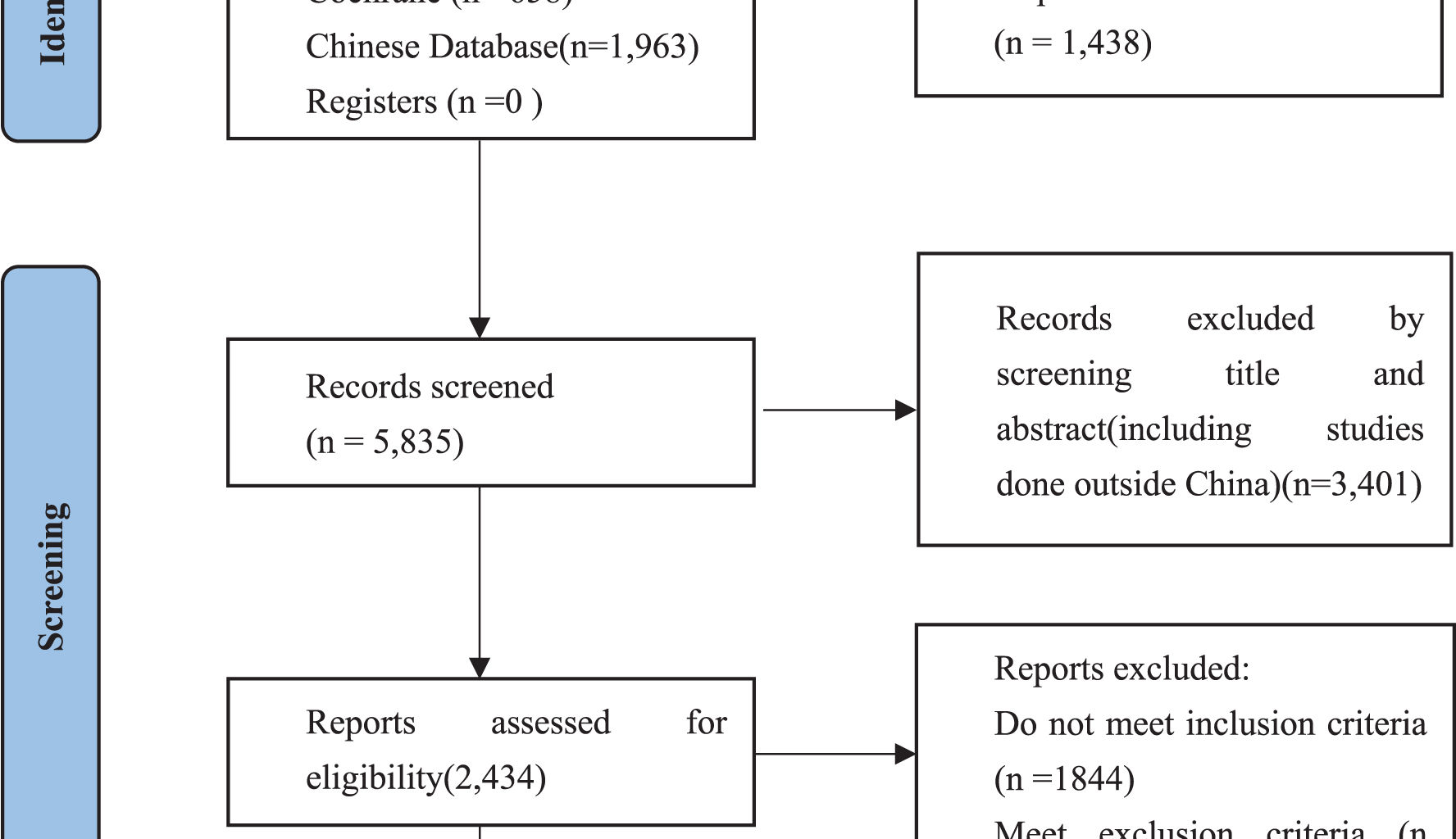
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev-Lond. 2015;4:1–9.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evid Implement. 2015;13(3):147–53.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Wang Z, Wang Y, Luo C, Fu R, Jiang Q. A study of factors influencing the comorbid metabolic syndrome in hospitalised schizophrenic patients. Home Med. 2019;4:86.
Wang S, Zhang H. A study to investigate the prevalence of concomitant metabolic syndrome in long-stay schizophrenic patients and related factors. Contemp Med. 2021;27(13):176–78.
Yang Z, Zhou L, Zhao C, Zhu J. Clinical study of metabolic syndrome associated with long-term hospitalised patients with chronic schizophrenia. Contemp Med. 2011;17(6):62–63.
Qin T, Tian T, Wang L, Wang C. Current status of metabolic syndrome and related influencing factors in long-term hospitalized schizophrenic patients. China Foreign Med Treat. 2023;42(26):46–49.
Zhong G. Analysis of influencing factors related to metabolic syndrome in chronic schizophrenic patients and preventive intervention. Mod Diagnosis Treat. 2017;28(9):1725–26.
Zhongya X. Analysis of the incidence and factors of metabolic syndrome in patients with schizophrenia. Med Health-Kuala Lum. 2024;2:28–31.
Demei Z. Comparison of the prevalence of metabolic syndrome in bipolar disorder and schizophrenia. Med J Chin People’s Health. 2011;23(12):1496–97.
Zhang H, Wang S. Analysis of the prevalence of metabolic syndrome and associated factors in hospitalised schizophrenic patients. Contemp Med. 2021;27(14):146–47.
Wu R, Song Z. Analysis of the prevalence of metabolic syndrome and related factors in schizophrenic patients taking antipsychotic medications. Med Health-Kuala Lum. 2023;5:51–54.
Li L, Hua L, Sujun G. Investigation on the situation and related factors of metabolic syndrome in longterm hospitalized patients with schizophrenia. Psychologies Mag. 2022;17(24):80–82.
Cui X, Cai X, Hu W. Analysis of influencing factors of metabolic syndrome in pa-tients with schizophrenia. J Educ Chang Clin Psychosomatic Dis. 2021;27(6):7–10.
Jibei S, Chunyou Z, Cuilu S. Incidence of metabolic syndrome in patients with schizophrenia and its influencing factors. J Retailing Changchun Univ Chin Med. 2023;39(3):319–22.
Zhang P, Huang J, Gou M, Zhou Y, Tong J, Fan F, et al. Kynurenine metabolism and metabolic syndrome in patients with schizophrenia. J Psychiatr Res. 2021;139:54–61.
Qiao Y, Wen H, Chen H, Xiang Z, Xue Z, Song Z, et al. The study of risk for metabolic syndromes in long-term hospitalized patients with schizophrenia. Shanghai Archiv Psychiatry. 2008;2:65–68.
Liu J, Wu J. Study of schizophrenia with metabolic syndrome and its associated factors. Med J Chin People’s Health. 2009;21(14):1657–59.
Xie R, Zhang L, Gao J, Sun Z, Chen S, Ju K. The related factors analysis and invention of metabolic syndrome in long-stay schizophrenic inpatients. Mod Med J. 2014;42(9):1058–62.
Yang Y. Correlation of levels of serum leptin and adiponectin with metabolic syndrome in patients with schizophrenia. Chin J Practical Med. 2021;48(9):51–53.
Ou J, Zhang C. Surveys of convalescence schizophrenics with metabolic syndrome. J Educ Chang Clin Psychosomatic Dis. 2013;19(3):214–16.
Lv J, Yang X, Kang Y, Jia C, Zhao X, Liu Y, et al. A survey of metabolic syndrome in schizophrenia. J Neurosci Ment Health. 2009;9(4):300–02.
Cao J, Jiang G, Su M, Guo Y. Construction and validation of a nomogram model for individualized prediction of the metabolic syndrome comorbidity risk in patients with schizophrenia. J Psychiatry. 2023;36(5):488–92.
Jianying C, Wentao C, Ruiqian L, Shaonan G, Ting H, Ming G, et al. The effect of first- versus second-generation antipsychotics on the metabolic syndrome in patients with chronic schizophrenia. Strait Pharm J. 2021;33(9):132–34.
You J, Shu F. Analysis of characteristics of metabolic syndrome in patients with chronic schizophrenia. J Qiqihar Univ Med. 2020;41(2):169–72.
Song X, Liu X, Ye M. Relationship between first-episode schizophrenia and metabolic syndrome: a case-control study. Chin J Rehabil Theory Pract. 2012;18(1):81–83.
Zhou Y, Song X, Guo Y, Lang X, Li Z, Zhang XY. Sex differences in metabolic disorder patterns of first-episode drug-naive patients with schizophrenia. Psychoneuroendocrino. 2021;124:105061.
Xie H, Zhou J, Wang F, Yin L, Feng Y. Prevalence of metabolic syndrome and its related factorsin schizophrenic inpatients. Med J Chin People’s Health. 2012;24(13):1549–53.
Chen J, Cheng W, Lin R, Guo S, Huang T, Gao M, et al. Prevalence of metabolic syndromein senile and pre-senilepatients with schizophrenia. Chin Foreign Med Res. 2020;18(19):40–42.
Chen VC, Chen C, Chiu Y, Lin T, Li F, Lu M. Leptin/Adiponectin ratio as a potential biomarker for metabolic syndrome in patients with schizophrenia. Psychoneuroendocrino. 2018;92:34–40.
Wang X. Study on related factors of schizophrenia complicated with metabolic syndrome. Capital Med. 2022;29(12):37–39.
Chang G, Wang S, Lu Z, Xie L, Lu Y, Xu X. A study of the prevalence of metabolic syndrome in schizophrenic inpatients and the factors influencing it. Ningxia Med J. 2023;45(12):1148–50.
Yueqian B, Heng S. Analysis of influencing factors of schizophrenia complicated with metabolic syndrome. Chin Community Doctors. 2024;40(2):16–18.
Yuan X, Yang Q, Yao Y, Song S, Zhou X, Liu H, et al. Role of HOMA-IR and IL-6 as screening markers for the metabolic syndrome in patients with chronic schizophrenia: a psychiatric hospital-based cross-sectional study. Eur Arch Psychiatry Clin Neurosci. 2024;274(5):1063–70. 2024-8-1.
Yao X, Xia L, Li W, Zhu M, Tao D, Liu H. Association between metabolic syndrome and the level of High-sensitivity C-reactive protein in patients with schizophrenia. Chin Gener Pract. 2020;23(3):294–98.
Yang L. Investigation of the prevalence of metabolic syndrome in patients with schizophrenia and discussion of prevention and control measures. Inner Mongolia Med J. 2019;51(11):1343–45.
Yang CY, Lo SC, Peng YC. Prevalence and predictors of metabolic syndrome in people with schizophrenia in inpatient rehabilitation wards. Biol Res Nurs. 2016;18(5):558–66. 2016-10-1.
Yang J, Liu H, Li Y, Ma J, Li Z. Prevalence rate of metabolic syndrome and associated factors in patients with Schizophre. J Health Psychol. 2012;20(6):808–09.
Li C, Zhan G, Rao S, Zhang H. Metabolic syndrome and its factors affect cognitive function in chronic schizophrenia complicated by metabolic syndrome. J Nerv Ment Dis. 2014;202(4):313–18.
Song Y, Fang X, Zhou C, Chen J, Liu D, Zhang X. A study of metabolic syndrome and cardiovascular disease risk factors in patients with schizophrenia. Clin J Med Officers. 2021;49(12):1346–49.
Lu W, Zheng H, Le H, Wu F, Hu W. Analysis of the related factors of the prevalence of metabolic syndrome in schizophrenia patients. J Clin Res. 2011;28(2):217–19.
Li W, Wang R. Prevalence of metabolic syndrome and it related in schizophrenic long-term inpatients. Med J Chin People’s Health. 2011;23(9):1068–69.
Zhang J, Wang J, Yang Y, Zhen Z. Prevalence of metabolic syndrome in schizophrenic long-term inpatients. J Neurosci And Ment Health. 2012;12(5):452–54.
Ye X, Yang Y, Gu W, Wang Q, Kong Z, Li M. A survey of the prevalence of concomitant metabolic syndrome in patients with schizophrenia. China Med Eng. 2014;22(6):183–85.
Li Z, Wang S, Chen Y, Wu X, Gu Y, Lang X, et al. Smoking affects the patterns of metabolic disorders and metabolic syndrome in patients with first-episode drug-naive schizophrenia: a large sample study based on the Chinese Han population. Int J Neuropsychopharmacol. 2021;24(10):798–807.
Huang W, Zhao Z, Bai Y, Jia H, Deng S, Ding L. Investigation of 456 hospitalized patients of schizophrenia with metabolic syndrome. China Med Her. 2012;9(22):124–26.
Liu J, Fu L. Metabolic syndrome in patients with schizophrenia: why should we care. Med (baltim). 2022;101(32):e29775.
Liu Y, Li H, Jiao Y, Wang P, Qian Z. Prevalence of metabolic syndrome and its related factors in schizophrenic inpatients. Shanghai Archiv Psychiatry. 2009;21(1):16–19.
Lang X, Zhou Y, Zhao L, Gu Y, Wu X, Zhao Y, et al. Differences in patterns of metabolic abnormality and metabolic syndrome between early-onset and adult-onset first-episode drug-naive schizophrenia patients. Psychoneuroendocrino. 2021;132:105344.
Yue D, Liu L, Fan Y, Dong Y. Investigation of metabolic syndrome in schizophrenics. J Clin Psychiat. 2011;21(5):326–28.
Cheng Z, Ling W, Zhou X, Ji Q. Prevalence of metabolic syndrome in patients with schizophrenia and its related factors. Chin J Behavioral Med Brain Sci. 2011;20(11):1012–15.
Li C, Shen W, Rao S. Investigation of the relative factors and quality of life of metabolic syndrome in schizophrenics. Med J Chin People’s Health. 2008;11:1112–14.
Huang MC, Lu ML, Tsai CJ, Chen PY, Chiu CC, Jian DL, et al. Prevalence of metabolic syndrome among patients with schizophrenia or schizoaffective disorder in Taiwan. Acta Psychiatr Scand. 2009;120(4):274–80.
Hu S, Liu X, Zhang Y, Ma J. Prevalence of metabolic syndrome and its associated factors in first-treatment drug-naive schizophrenia patients: a large-scale cross-sectional study. Early Interv Psychiatry. 2025;19(1):e13565.
Ye F, Liu X, Liu Y, Wang F, Jiang J. Analysis of long-term hospitalization detection rate and related factors of metabolic syndrome in patients with schizophrenia. Sichuan Ment Health. 2015;28(1):48–50.
Wang X, Yang J, Liu N, Xu D. Investigation of prevalence of metabolic syndrome in hospitalized patients with schizophrenia. J Med Forum. 2011;32(11):35–37.
Li D, Zhang Q, Liu G, Zheng L, Wu X, Yu W. Correlation between schizophrenia and metabolic synd rome. Chin Gener Pract. 2014;17(34):4083–86.
Zhong Y, Xie S, Yu J, Cai L, Yang Y. Survey of metabolic syndrome in 780 chronically hospitalized patients with schizophrenia. J Mod Clin Med. 2017;43(2):105–07.
Zhang B, Wang F, Wang X, Lu L, Wu S, Zhou Y, et al. Factors related to hospitalized schizophrenics with metabolic syndrome. Chin Ment Health J. 2006;10:661–64.
Luo X, Zhong L, Yan Y, Zhou W. Characterisation of the prevalence of metabolic syndrome in community schizophrenic patients in Shapingba District, Chongqing. Practical Preventative Med. 2020;27(10):1237–39.
Luo Q. Analysis of factors influencing the development of metabolic syndrome in schizophrenic patients with concomitant metabolic syndrome. Mod Med Health Res. 2021;5(10):127–29.
Xu H, Zhou Y, Zeng L, Huang W, Yang X, Li G, et al. Gender differences on incidence of metabolic syndrome and metabolic parameters in patients with chronic schizo- phrenia. Chin J Nerv Ment Dis. 2021;47(11):656–60.
Fan Y, Zhong S, Zhou L, Su J, Chen X, Huang X. Influencing factors of metabolic syndrome in community patients with schizophrenia. Sichuan Ment Health. 2023;36(6):515–20.
Gan H, Peng S, Lu Z, Wu Y, Yi Z, Yang D, et al. Prevalence and clinical characteristics of the metabolic syndrome in of inpatients with schizophrenia in Shanghai. J Clin Psychiatry. 2022;32(2):126–28.
Xie Z. Status study of the morbidity of concomitant metabolic syndromes of inpatient schizophrenia patients and its hazardous factors. 2024 [Master’s thesis]: Guangzhou Medical University.
Huang G, Yang Y. Construction of a risk warning model for metabolic syndrome caused by antipsychotic drugs in patients with schizophrenia. Jiangxi Med J. 2024;59(8):762–65.
Guo Y, Xu Y, Zeng W, Tan Y. Current status and comprehensive predictive model construction of metabolic syndrome comorbidity in schizophrenia patients. South China J Prev Med. 2025;51(1):90–93.
Xie H, Wang Y, Zheng C. Factors influencing the impact of schizophrenia and metabolic syndrome and the significance of measuring ApoA1 and Lp(a). Zhejiang Practical Med. 2024;29(6):503–05.
Kejin MO, Jie L. Real-world clinical characteristics and pharmacoeconomic evaluation of comorbidity in patients with schizophrenia. Chin J Drug Abuse Prev Treat. 2025;31(1):22–24.
Qi X, Yan J. A comparative analysis of metabolic syndrome in han Chinese patients with schizophrenia. J Bingtuan Med. 2005;4:3–5.
Xing G, Meixu L, Qianlong W, Qi M. Correlation between sleep quality and cognitive function in schizophrenia patients with metabolic syndrome. J Neurosci Ment Health. 2024;24(11):767–73.
Hu C. Guidelines and explanations recommended for the diagnosis and classification of schizophrenia. Nerv Dis Ment Health. 2005;5(6):483–87.
De Hert M, van Winkel R, Van Eyck D, Hanssens L, Wampers M, Scheen A, et al. Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health: CP EMH. 2006;2:14.
Tao H, Shen D, Zhou Y, Sun F, Li G, Jin W. A systematic review and meta-analysis of metabolic syndrome prevalence in Chinese inpatients with bipolar disorder. Horm Metab Res. 2022;54(9):587–92.
Patel JK, Buckley PF, Woolson S, Hamer RM, McEvoy JP, Perkins DO, et al. Metabolic profiles of second-generation antipsychotics in early psychosis: findings from the CAFE study. Schizophr Res. 2009;111(1–3):9–16.
Meyer JM, Stahl SM. The metabolic syndrome and schizophrenia. Acta Psychiatr Scand. 2009;119(1):4–14.
Rodriguez-Monforte M, Sanchez E, Barrio F, Costa B, Flores-Mateo G. Metabolic syndrome and dietary patterns: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2017;56(3):925–47.
Challa F, Getahun T, Sileshi M, Geto Z, Kelkile TSGurmessa S, et al. Prevalence of metabolic syndrome among patients with schizophrenia in Ethiopia. BMC Psychiatry. 2021;21(1):620.
Sugai T, Suzuki Y, Yamazaki M, Shimoda K, Mori T, Ozeki Y, et al. Difference in prevalence of metabolic syndrome between Japanese outpatients and inpatients with schizophrenia: a nationwide survey. Schizophr Res. 2016;171(1–3):68–73.
Kagal UA, Torgal SS, Patil NM, Malleshappa A. Prevalence of the metabolic syndrome in schizophrenic patients receiving second-generation antipsychotic agents-a cross-sectional study. J Pharm Pract. 2012;25(3):368–73.
Severi E, Ferrara M, Tedeschini E, Vacca F, Mungai F, Amendolara R, et al. Assessment of cardiovascular risk in an Italian psychiatric outpatient sample: a chart review of patients treated with second-generation antipsychotics. Int J Ment Health Nu. 2018;27(3):1002–08.
Thakore JH. Metabolic disturbance in first-episode schizophrenia. Br J Psychiatry Suppl. 2004;47:S76–9.
Wu X, Huang Z, Wu R, Zhong Z, Wei Q, Wang H, et al. The comparison of glycometabolism parameters and lipid profiles between drug-naive, first-episode schizophrenia patients and healthy controls. Schizophr Res. 2013;150(1):157–62.
Dasgupta A, Singh OP, Rout JK, Saha T, Mandal S. Insulin resistance and metabolic profile in antipsychotic naive schizophrenia patients. Prog Neuro-Psychoph. 2010;34(7):1202–07.
Liang J, Cai Y, Xue X, Li X, Li Z, Xu C, et al. Does schizophrenia itself cause obesity? Front Psychiatry. 2022;13:934384.
Chen DC, Du XD, Yin GZ, Yang KB, Nie Y, Wang N, et al. Impaired glucose tolerance in first-episode drug-naive patients with schizophrenia: relationships with clinical phenotypes and cognitive deficits. Psychol Med. 2016;46(15):3219–30.
Aoki R, Saito T, Ninomiya K, Shimasaki A, Ashizawa T, Ito K, et al. Shared genetic components between metabolic syndrome and schizophrenia: genetic correlation using multipopulation data sets. Psychiat Clin Neuros. 2022;76(8):361–66.
Grover S, Nebhinani N, Chakrabarti S, Avasthi A, Basu D, Kulhara P, et al. Cardiac risk factors and metabolic syndrome in patients with schizophrenia admitted to a general hospital psychiatric unit. Indian J Psychiat. 2014;56(4):371–76.
Shi L, Ascher-Svanum H, Chiang YJ, Zhao Y, Fonseca V, Winstead D. Predictors of metabolic monitoring among schizophrenia patients with a new episode of second-generation antipsychotic use in the veterans health administration. BMC Psychiatry. 2009;9:80.
Sun MJ, Jang MH. Risk factors of metabolic syndrome in Community-Dwelling People with schizophrenia. Int J Environ Res Pub Health Public Health. 2020;17(18).
Jung UJ, Choi MS. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15(4):6184–223.
Dickerson F, Origoni A, Schroeder J, Adamos M, Katsafanas E, Khushalani S, et al. Natural cause mortality in persons with serious mental illness. Acta Psychiatr Scand. 2018;137(5):371–79.
Liu Z, Liang Q, Ren Y, Guo C, Ge X, Wang L, et al. Immunosenescence: molecular mechanisms and diseases. Signal Transduct Tar. 2023;8(1):200.
Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. 2015;402:113–19.
Da ST, Ravindran AV. Contribution of sex hormones to gender differences in schizophrenia: a review. Asian J Psychiatr. 2015;18:2–14.
Bressington DT, Mui J, Cheung EF, Petch J, Clark AB, Gray R. The prevalence of metabolic syndrome amongst patients with severe mental illness in the community in Hong Kong-a cross sectional study. BMC Psychiatry. 2013;13:1–8.
Vancampfort D, Firth J, Schuch FB, Rosenbaum S, Mugisha J, Hallgren M, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry: Off J World Psychiatric Assoc (WPA). 2017;16(3):308–15.
Adamowicz K, Kucharska-Mazur J. Dietary behaviors and metabolic syndrome in schizophrenia patients. J Clin Med. 2020;9(2).
Aberg F, Byrne CD, Pirola CJ, Mannisto V, Sookoian S. Alcohol consumption and metabolic syndrome: clinical and epidemiological impact on liver disease. J Hepatol. 2023;78(1):191–206.