A 28-year-old Caucasian male patient, previously healthy, presented with a one-week history of right lower quadrant (RLQ) pain. Pain is qualified as stabbing in nature, increases with motion, intermittent, with no radiation to other areas. The patient did not report any other symptoms, and a history of previous trauma or urinary problems was negative.
Vital signs on presentation were as follows: blood pressure 110/70 mmHg, heart rate 74 beats per minute, respiratory rate 13 breaths per minute, temperature 36.6 Celsius (°C), and an oxygen saturation of 98%. Physical examination revealed a soft abdomen with no visible or palpable mass, associated with mild tenderness upon deep compression on the RLQ. Respiratory, cardiovascular, and neurological exams were unremarkable. Routine laboratory tests on admission were normal regarding complete blood count, C-reactive protein, and urine analysis. Abdominopelvic ultrasound was ordered and revealed a small paracecal cystic collection of 2 × 2 cm without signs of appendicitis or free fluid. Thus, a CT scan of the abdomen and pelvis with IV and PO contrast was requested, demonstrating a 2.3 × 1.8 cm cystic collection with internal septation at the level of the cecum, 4 cm above the normal appendix, with mild fat stranding. The two major differential diagnoses at this level, based on the clinical presentation and the radiological findings, were cecal diverticulitis or complicated appendagitis. After consultation with the gastroenterology team, a 10-day course of Ibuprofen 400 mg orally twice daily, Ciprofloxacin 500 mg orally twice daily, and metronidazole 500 mg orally three times daily was started.
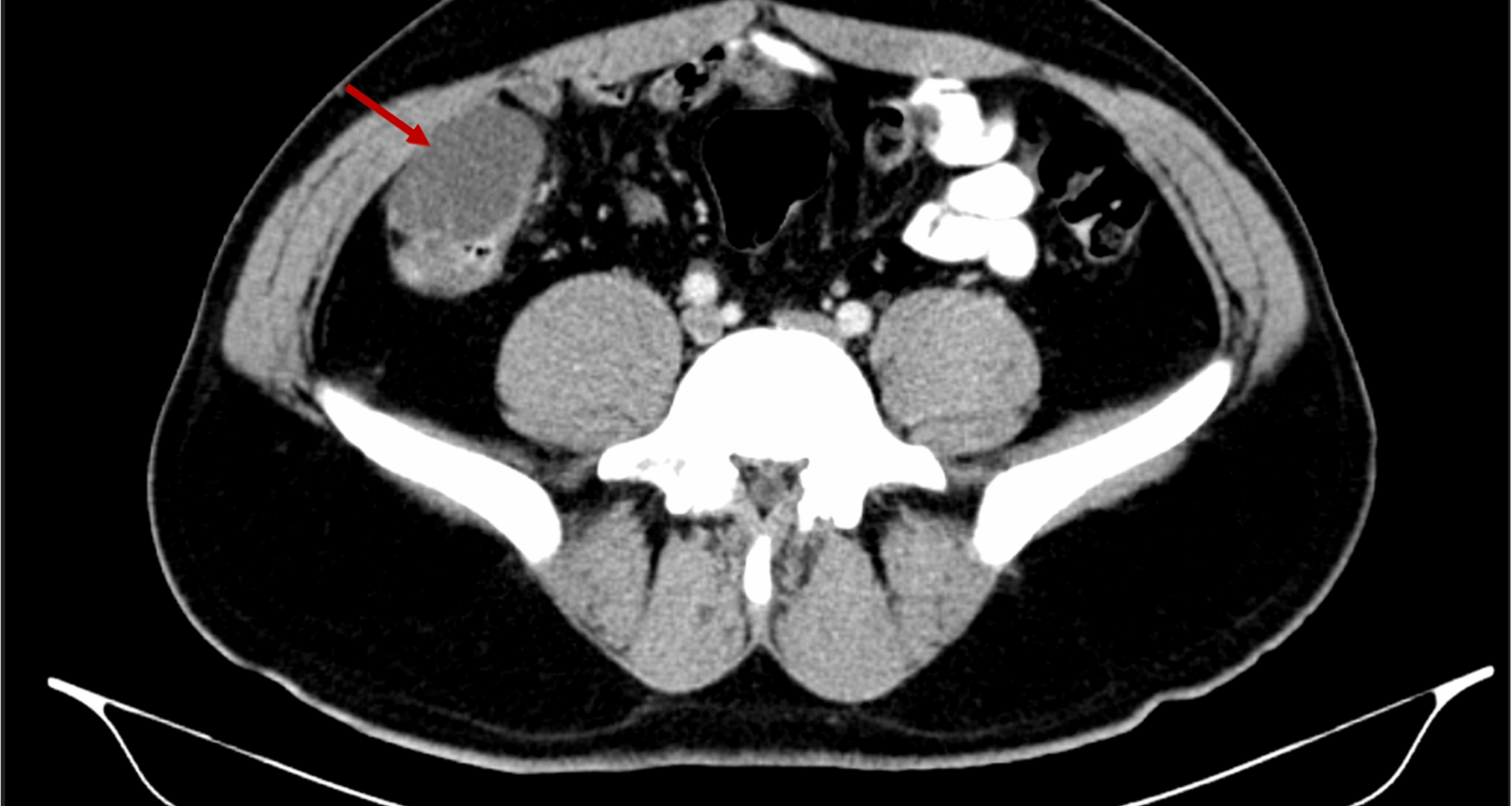
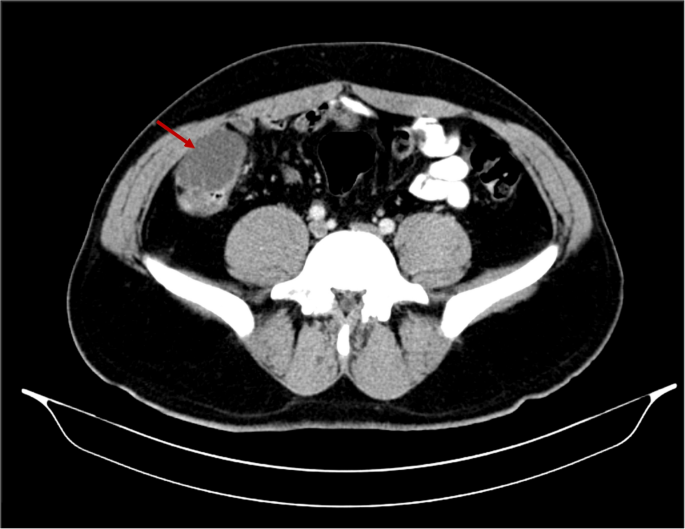
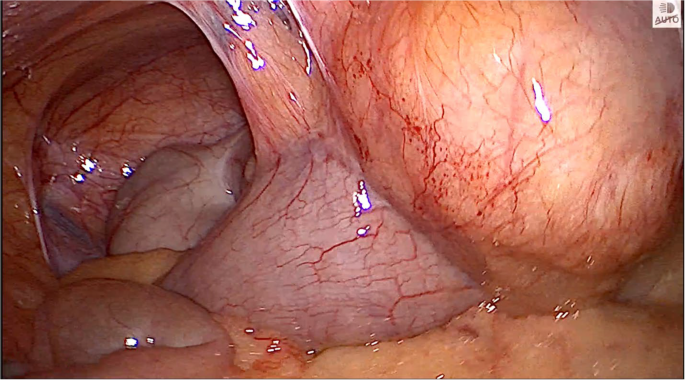
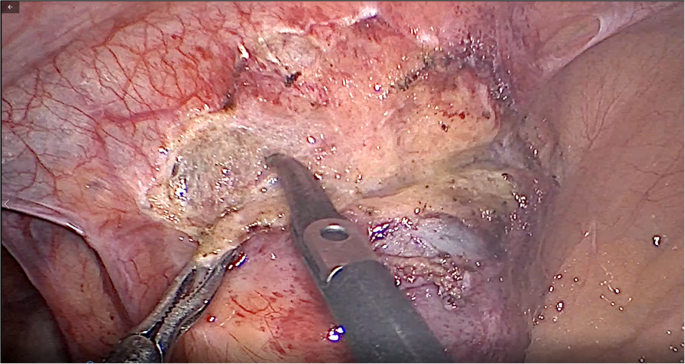
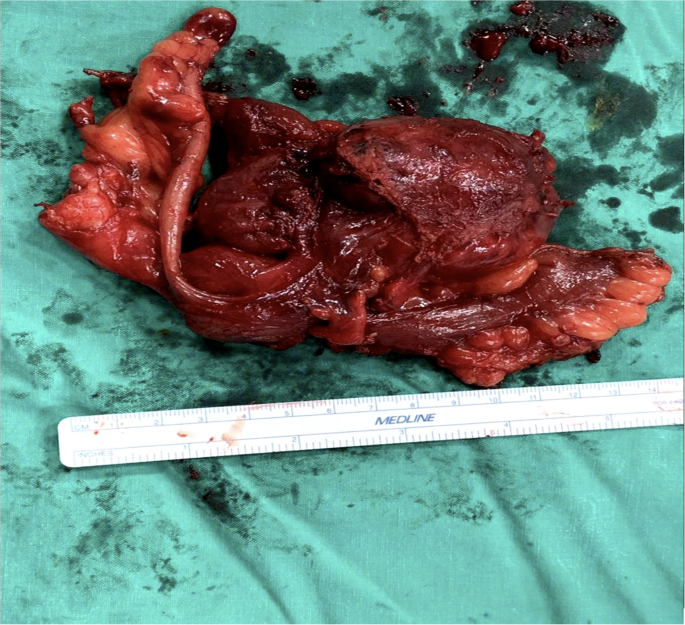
Upon reassessment post 10-day course, the patient stated that the pain decreased in severity but did not go away and was still causing discomfort. A follow-up abdomino-pelvic CT with IV and PO contrast was performed and revealed an increase in the size of the cystic collection to 4.3 × 5.5 cm, with enhancement of the previous fat stranding, adherence to the cecal wall medially, and to the abdominal wall laterally, with the suggestion of a possible complicated appendagitis or duplicated cyst as the main cause (Fig. 1). No mass lesion, adenopathy, or ascites was noted. The decision was taken to go for diagnostic laparoscopy. After insufflation and pneumoperitoneum creation, a fixed mass was perceived on the cecum, severely adherent to the cecal wall, and to the lateral peritoneal reflection, which was inconsistent with inflammatory lesions such as diverticulitis or epiploic appendagitis (Fig. 2). Successful dissection of the mass from the lateral wall was accomplished using scissors and cautery (Fig. 3). However, upon dissecting the mass from its connection to the cecal wall, great difficulty was experienced, with failure of the dissection, especially after noticing the presence of a common vessel supplying the cecum and the cyst at the same time. As a result, an ileocecectomy was decided by exteriorizing the ileum, cecum, and the cyst through a 6 cm RLQ incision and applying a mechanical side-to-side ileocolic anastomosis, then returning the bowel to the peritoneal cavity, followed by deflation and closure (Fig. 4). Postoperatively, the patient had mild pain with no major complaints, and was discharged home four days later.
Cystic collection to 4.3 × 5.5 cm, with fat stranding and adherence to the cecal wall medially and the abdominal wall laterally
Cecal mass severely adherent to the cecal wall and to the lateral peritoneal reflection
Dissection of the mass from the lateral wall using scissors and cautery
Specimen of the ileum, cecum, and cyst
The pathology report came back as a cystic lesion measuring 5 × 4 × 2.8 cm, adherent to the cecal serosal tissue with no communication to the cecal lumen, alongside the presence of duplication of the colonic wall at the cecal level, spherical in type, thus confirming the diagnosis of a cecal duplication cyst as the root etiology of our patient’s condition. No granuloma or malignancy was observed. The patient remains asymptomatic at the 6-month outpatient follow-up appointment.