Carabotti, M., Scirocco, A., Antonietta Maselli, M. & Severi, C. The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems 28 www.annalsgastro.gr (2015).
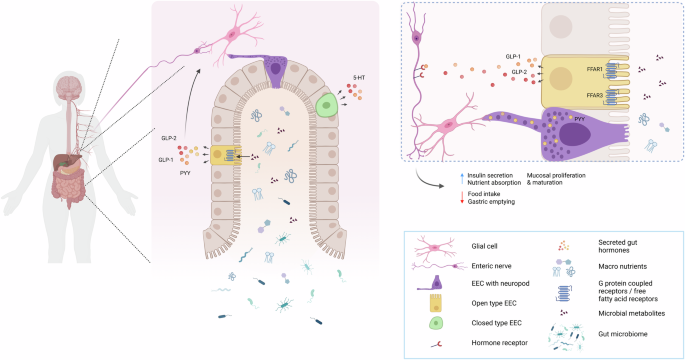
Worthington, J. J., Reimann, F. & Gribble, F. M. Enteroendocrine cells-sensory sentinels of the intestinal environment and orchestrators of mucosal immunity. Mucosal Immunol. 11, 3–20 (2018).
Latorre, R., Sternini, C., De Giorgio, R. & Greenwood-Van Meerveld, B. Enteroendocrine cells: a review of their role in brain-gut communication. Neurogastroenterol. Motil. 28, 620–630 (2016).
Gribble, F. M. & Reimann, F. Enteroendocrine cells: chemosensors in the intestinal epithelium. Annu. Rev. Physiol. 78, 277–299 (2016).
Gribble, F. M. & Reimann, F. Function and mechanisms of enteroendocrine cells and gut hormones in metabolism. Nat. Rev. Endocrinol. 15, 226–237 (2019).
Zeve, D. et al. Robust differentiation of human enteroendocrine cells from intestinal stem cells. Nat. Commun. 13, 261 (2022).
Atanga, R., Singh, V. & In, J. G. Intestinal enteroendocrine cells: present and future druggable targets. Int. J. Mol. Sci. 24, 8836 (2023).
Bohórquez, D. V. et al. Neuroepithelial circuit formed by innervation of sensory enteroendocrine cells. J. Clin. Investig. 125, 782–786 (2015).
Karra, E., Chandarana, K. & Batterham, R. L. The role of peptide YY in appetite regulation and obesity. J. Physiol. 587, 19–25 (2009).
Dockray, G. J. Cholecystokinin and gut-brain signalling. Regulatory Pept. 155, 6–10 (2009).
Karra, E. & Batterham, R. L. The role of gut hormones in the regulation of body weight and energy homeostasis. Mol. Cell. Endocrinol. 316, 120–128 (2010).
Kaunitz, J. D. & Akiba, Y. Control of intestinal epithelial proliferation and differentiation: the microbiome, enteroendocrine L cells, telocytes, enteric nerves, and GLP, too. Dig. Dis. Sci. 64, 2709–2716 (2019).
Liddle, R. A. Neuropods. CMGH 7, 739–747 (2019).
Loh, Y. P., Xiao, L. & Park, J. J. Trafficking of hormones and trophic factors to secretory and extracellular vesicles: a historical perspective and new hypothesis. Extracell. Vesicles Circulating Nucleic Acids 4, 568–587 (2023).
Park, J. J. & Loh, Y. P. How peptide hormone vesicles are transported to the secretion site for exocytosis. Mol. Endocrinol. 22, 2583–2595 (2008).
Bohórquez, D. V. et al. An enteroendocrine cell—Enteric glia connection revealed by 3D electron microscopy. PLoS ONE 9, e89881 (2014).
Rao, M. et al. Enteric glia regulate gastrointestinal motility but are not required for maintenance of the epithelium in mice. Gastroenterology 153, 1068–1081.e7 (2017).
Santhosh, S., Zanoletti, L., Stamp, L. A., Hao, M. M. & Matteoli, G. From diversity to disease: unravelling the role of enteric glial cells. Front. Immunol. 15, 1408744 (2024).
Spencer, N. J. & Hu, H. Enteric nervous system: sensory transduction, neural circuits and gastrointestinal motility. Nat. Rev. Gastroenterol. Hepatol. 17, 338–351 (2020).
Timpka, J. & Odin, P. Gastrointestinal dysfunction in Parkinson’s disease. Int. Rev. Movement Disorders 1, 179–208 (2021).
Fine, R. E. In Receptors in the Evolution and Development of the Brain, pp. 183–191 (Elsevier, 2019). https://doi.org/10.1016/C2016-0-00013-X.
Waclawiková, B., Codutti, A., Alim, K. & El Aidy, S. Gut microbiota-motility interregulation: insights from in vivo, ex vivo and in silico studies. Gut Microbes 14, 1997296 (2022).
Progatzky, F. & Pachnis, V. The role of enteric glia in intestinal immunity. Curr. Opin. Immunol. 77, 102183 (2022).
Seguella, L. & Gulbransen, B. D. Enteric glial biology, intercellular signalling and roles in gastrointestinal disease. Nat. Rev. Gastroenterol. Hepatol. 18, 571–587 (2021).
Savidge, T. C., Sofroniew, M. V. & Neunlist, M. Starring roles for astroglia in barrier pathologies of gut and brain. Lab. Investig. 87, 731–736 (2007).
De Giorgio, R. et al. Enteric glia and neuroprotection: basic and clinical aspects. Am. J. Physiol. Gastro-intest Liver Physiol. 303, 887–893 (2012).
Han, Y. et al. Vagus nerve and underlying impact on the gut microbiota-brain axis in behavior and neurodegenerative diseases. J. Inflamm. Res. 15, 6213–6230 (2022).
Corp, E. S., McQuade, J., Moran, T. H. & Smith, G. P. Characterization of type A and type B CCK receptor binding sites in rat vagus nerve. Brain Res. 623, 161–166 (1993).
Kaelberer, M. M. et al. A gut-brain neural circuit for nutrient sensory transduction. Science 361, eaat5236 (2018).
López-Ojeda, W. & Hurley, R. A. The vagus nerve and the brain-gut axis: implications for neuropsychiatric disorders. J. Neuropsychiatry Clin. Neurosci. 36, 278–282 (2024).
Breit, S., Kupferberg, A., Rogler, G. & Hasler, G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front. Psychiatry 9, 44 (2018).
Bharwani, A., Mian, M. F., Surette, M. G., Bienenstock, J. & Forsythe, P. Oral treatment with Lactobacillus rhamnosus attenuates behavioural deficits and immune changes in chronic social stress. BMC Med. 15, 7 (2017).
Bravo, J. A. et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl Acad. Sci. USA 108, 16050–16055 (2011).
Schmidt, K. et al. Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology (Berl.) 232, 1793–1801 (2015).
Homan, P. et al. Serotonin versus catecholamine deficiency: behavioral and neural effects of experimental depletion in remitted depression. Transl. Psychiatry 5, e532 (2015).
Ye, L. et al. Enteroendocrine cells sense bacterial tryptophan catabolites to activate enteric and vagal neuronal pathways. Cell Host Microbe 29, 179–196.e9 (2021).
Tian, P., Wang, G., Zhao, J., Zhang, H. & Chen, W. Bifidobacterium with the role of 5-hydroxytryptophan synthesis regulation alleviates the symptom of depression and related microbiota dysbiosis. J. Nutritional Biochem. 66, 43–51 (2019).
Woźniak, D., Cichy, W., Przysławski, J. & Drzymała-Czyż, S. The role of microbiota and enteroendocrine cells in maintaining homeostasis in the human digestive tract. Adv. Med. Sci. 66, 284–292 (2021).
Prosapio, J. G., Sankar, P. & Jialal, I. Physiology, Gastrin (StatPearls Publishing, Treasure Island (FL), 2023).
Holst, J. J. The incretin system in healthy humans: the role of GIP and GLP-1. Metabolism 96, 46–55 (2019).
Martin, A. M., Sun, E. W., Rogers, G. B. & Keating, D. J. The influence of the gut microbiome on host metabolism through the regulation of gut hormone release. Front. Physiol. 10, 428 (2019).
Thomsen, C. et al. Differential effects of saturated and monounsaturated fatty acids on postprandial lipemia and incretin responses in healthy subjects. Am. J. Clin. Nutr. 69, 1135–1143 (1999).
Posovszky, C. & Wabitsch, M. Regulation of appetite, satiation, and body weight by enteroendocrine cells. Part 1: Characteristics of enteroendocrine cells and their capability of weight regulation. Horm. Res. Paediatrics 83, 1–10 (2015).
Amato, A., Baldassano, S. & Mulè, F. GLP2: An underestimated signal for improving glycaemic control and insulin sensitivity. J. Endocrinol. 229, R57–R66 (2016).
Rakipovski, G. et al. The GLP-1 analogs liraglutide and semaglutide reduce atherosclerosis in ApoE −/− and LDLr −/− mice by a mechanism that includes inflammatory pathways. JACC Basic Transl. Sci. 3, 844–857 (2018).
Knudsen, L. B. & Lau, J. The discovery and development of liraglutide and semaglutide. Front. Endocrinol. 10, 155 (2019).
Burness, C. B. & McCormack, P. L. Teduglutide: a review of its use in the treatment of patients with short bowel syndrome. Drugs 73, 935–947 (2013).
Sabra, H. K. et al. Efficacy and safety of glucagon-like peptide 2 in patients with short bowel syndrome: a systematic review and network meta-analysis. J. Gastrointest. Surg. 28, 1194–1205 (2024).
Oertel, M. et al. GLP-1 and PYY for the treatment of obesity: a pilot study on the use of agonists and antagonists in diet-induced rats. Endocr. Connect 13, e230398 (2024).
Guida, C. et al. PYY plays a key role in the resolution of diabetes following bariatric surgery in humans. EBioMedicine 40, 67–76 (2019).
Gerspach, A. C., Steinert, R. E., Schönenberger, L., Graber-Maier, A. & Beglinger, C. The role of the gut sweet taste receptor in regulating GLP-1, PYY, and CCK release in humans. Am. J. Physiol. Endocrinol. Metab. 301, 317–325 (2011).
Brown, R. J., Walter, M. & Rother, K. I. Ingestion of diet soda before a glucose load augments glucagon-like peptide-1 secretion. Diabetes Care 32, 2184–2186 (2009).
Ye, L. et al. High fat diet induces microbiota-dependent silencing of enteroendocrine cells. Elife 8, e48479 (2019).
Ohue-Kitano, R., Banno, Y., Masujima, Y. & Kimura, I. Gut microbial metabolites reveal diet-dependent metabolic changes induced by nicotine administration. Sci. Rep. 14, 1056 (2024).
Procházková, N. et al. Gut physiology and environment explain variations in human gut microbiome composition and metabolism. Nat. Microbiol 9, 3210–3225 (2024).
Cani, P. D., Everard, A. & Duparc, T. Gut microbiota, enteroendocrine functions and metabolism. Curr. Opin. Pharmacol. 13, 935–940 (2013).
Arora, T., Vanslette, A. M., Hjorth, S. A. & Bäckhed, F. Microbial regulation of enteroendocrine cells. Med 2, 553–570 (2021).
Akiba, Y. et al. Short-chain fatty acid sensing in rat duodenum. J. Physiol. 593, 585–599 (2015).
Tolhurst, G. et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61, 364–371 (2012).
Nøhr, M. K. et al. GPR41/FFAR3 and GPR43/FFAR2 as cosensors for short-chain fatty acids in enteroendocrine cells vs FFAR3 in enteric neurons and FFAR2 in enteric leukocytes. Endocrinology 154, 3552–3564 (2013).
Samuel, B. S. et al. Effects of the Gut Microbiota on Host Adiposity Are Modulated by the Short-Chain Fatty-Acid Binding G Protein-Coupled Receptor, Gpr41. www.pnas.org/cgi/content/full/ (2008).
Psichas, A. et al. The short chain fatty acid propionate stimulates GLP-1 and PYY secretion via free fatty acid receptor 2 in rodents. Int J. Obes. 39, 424–429 (2015).
Torres-Fuentes, C. et al. Short-chain fatty acids and microbiota metabolites attenuate ghrelin receptor signaling. FASEB J. 33, 13546–13559 (2019).
Chimerel, C. et al. Bacterial metabolite indole modulates incretin secretion from intestinal enteroendocrine L cells. Cell Rep. 9, 1202–1208 (2014).
Yano, J. M. et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161, 264–276 (2015).
Gautier, T. et al. Roseburia intestinalis modulates PYY expression in a new a multicellular model including enteroendocrine cells. Microorganisms 10, 2263 (2022).
Porter, N. T., Luis, A. S. & Martens, E. C. Bacteroides thetaiotaomicron. Trends Microbiol. 26, 966–967 (2018).
Modasia, A. et al. Regulation of enteroendocrine cell networks by the major human gut symbiont bacteroides thetaiotaomicron. Front Microbiol 11, 575595 (2020).
LeValley, S. L., Tomaro-Duchesneau, C. & Britton, R. A. Degradation of the incretin hormone glucagon-like peptide-1 (GLP-1) by enterococcus faecalis metalloprotease GelE. mSphere 5, e00585–19 (2020).
Steck, N. et al. Enterococcus faecalis metalloprotease compromises epithelial barrier and contributes to intestinal inflammation. Gastroenterology 141, 959–971 (2011).
Maharshak, N. et al. Enterococcus faecalis gelatinase mediates intestinal permeability via protease-activated receptor 2. Infect. Immun. 83, 2762–2770 (2015).
Ottman, N., Geerlings, S. Y., Aalvink, S., de Vos, W. M. & Belzer, C. Action and function of Akkermansia muciniphila in microbiome ecology, health and disease. Best. Pract. Res.: Clin. Gastroenterol. 31, 637–642 (2017).
Yoon, H. S. et al. Akkermansia muciniphila secretes a glucagon-like peptide-1-inducing protein that improves glucose homeostasis and ameliorates metabolic disease in mice. Nat. Microbiol. 6, 563–573 (2021).
Everard, A. et al. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes 60, 2775–2786 (2011).
Kim, E. J. et al. High levels of akkermansia muciniphilia growth associated with spring water ingestion prevents obesity and hyperglycemia in a high-fat diet-induced mouse model. Nat. Prod. Commun. 17 (2022).
Everard, A. et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc. Natl Acad. Sci. USA 110, 9066–9071 (2013).
Louis, S., Tappu, R. M., Damms-Machado, A., Huson, D. H. & Bischoff, S. C. Characterization of the gut microbial community of obese patients following a weight-loss intervention using whole metagenome shotgun sequencing. PLoS ONE 11, e0149564 (2016).
Mack, I. et al. Weight gain in anorexia nervosa does not ameliorate the faecal microbiota, branched chain fatty acid profiles, and gastrointestinal complaints. Sci. Rep. 6, 26742 (2016).
Desai, M. S. et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell 167, 1339–1353.e21 (2016).
Chatzipanagiotou, O. et al. All you need to know about gastrinoma today|Gastrinoma and Zollinger-Ellison syndrome: a thorough update. J. Neuroendocrinol. 35, e13267 (2023).
George, J., Ramage, J., White, B. & Srirajaskanthan, R. The role of serotonin inhibition within the treatment of carcinoid syndrome. Endocrine Oncol. 3, e220077 (2023).
Yu, Y., Yang, W., Li, Y. & Cong, Y. Enteroendocrine cells: sensing gut microbiota and regulating inflammatory bowel diseases. Inflamm. Bowel Dis. 26, 11–20 (2020).
Moran, G. W., Pennock, J. & McLaughlin, J. T. Enteroendocrine cells in terminal ileal Crohn’s disease. J. Crohns Colitis 6, 871–880 (2012).
El-Salhy, M., Danielsson, Å., Stenling, R. & Grimelius, L. Colonic endocrine cells in inflammatory bowel disease. J. Intern. Med. 242, 413–419 (1997).
Selleri, S. et al. Induction of pro-inflammatory programs in enteroendocrine cells by the Toll-like receptor agonists flagellin and bacterial LPS. Int. Immunol. 20, 961–970 (2008).
Dinarello, C. A. & Kim, S.-H. IL-32, a novel cytokine with a possible role in disease. Ann. Rheum. Dis. 65, iii61 (2006).
Tao, E. et al. Potential roles of enterochromaffin cells in early life stress-induced irritable bowel syndrome. Front. Cell. Neurosci. 16, 837166 (2022).
Chow, C. F. W. et al. From psychology to physicality: how nerve growth factor transduces early life stress into gastrointestinal motility disorders later in life. Cell Cycle 18, 1824–1829 (2019).
Wong, H. L. X. et al. Early life stress disrupts intestinal homeostasis via NGF-TrkA signaling. Nat. Commun. 10, 1745 (2019).
Heymsfield, S. B. & Wadden, T. A. Mechanisms, pathophysiology, and management of obesity. N. Engl. J. Med. 376, 254–266 (2017).
WHO. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2024).
Jeffery, R. W. & Harnack, L. J. Evidence implicating eating as a primary driver for the obesity epidemic. Diabetes 56, 2673–2676 (2007).
Vandevijvere, S., Chow, C. C., Hall, K. D., Umali, E. & Swinburn, B. A. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull. World Health Organ 93, 446–456 (2015).
Klein, S., Gastaldelli, A., Yki-Järvinen, H. & Scherer, P. E. Why does obesity cause diabetes? Cell Metab. 34, 11–20 (2022).
Steinert, R. E. et al. Ghrelin, CCK, GLP-1, and PYY(3-36): secretory controls and physiological roles in eating and glycemia in health, obesity, and after RYGB. Physiol. Rev. 97, 411–463 (2017).
Marzullo, P. et al. The relationship between active ghrelin levels and human obesity involves alterations in resting energy expenditure. J. Clin. Endocrinol. Metab. 89, 936–939 (2004).
English, P. J., Ghatei, M. A., Malik, I. A., Bloom, S. R. & Wilding, J. P. H. Food fails to suppress ghrelin levels in obese humans. J. Clin. Endocrinol. Metab. 87, 2984–2987 (2002).
Cummings, D. E. et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 346, 1623–1630 (2002).
De Krom, M. et al. Common genetic variations in CCK, leptin, and leptin receptor genes are associated with specific human eating patterns. Diabetes 56, 276–280 (2007).
Marchal-Victorion, S. et al. Genetic, pharmacological and functional analysis of cholecystokinin-1 and cholecystokinin-2 receptor polymorphism in type 2 diabetes and obese patients. Pharmacogenetics 12, 23–30 (2002).
Rushakoff, R. A. et al. Reduced postprandial cholecystokinin (CCK) secretion in patients with noninsulin-dependent diabetes mellitus: evidence for a role for CCK in regulating postprandial hyperglycemia. J. Clin. Endocrinol. Metab. 76, 489–493 (1993).
Bucceri, A. M., Calogero, A. E. & Brogna, A. Gallbladder and gastric emptying: relationship to cholecystokininemia in diabetics. Eur. J. Intern. Med. 13, 123–128 (2002).
Calanna, S. et al. Secretion of glucagon-like peptide-1 in patients with type 2 diabetes mellitus: Systematic review and meta-analyses of clinical studies. Diabetologia 56, 965–972 (2013).
Collins, L. & Costello, R. A. Glucagon-like peptide-1 receptor agonists. StatPearls https://www.ncbi.nlm.nih.gov/books/NBK551568/ (2024).
Unger, J. & Parkin, C. G. Type 2 diabetes: an expanded view of pathophysiology and therapy. Postgrad. Med. 122, 145–157 (2010).
Aranias, T. et al. Lipid-rich diet enhances L-cell density in obese subjects and in mice through improved L-cell differentiation. J. Nutr. Sci. 4, e22 (2015).
Osinski, C. et al. Type 2 diabetes is associated with impaired jejunal enteroendocrine GLP-1 cell lineage in human obesity. Int J. Obes. 45, 170–183 (2021).
Uellendahl-Werth, F. et al. Cross-tissue transcriptome-wide association studies identify susceptibility genes shared between schizophrenia and inflammatory bowel disease. Commun. Biol. 5, 80 (2022).
Yu, L. & Li, Y. Involvement of intestinal enteroendocrine cells in neurological and psychiatric disorders. Biomedicines 10, 2577 (2022).
Lin, Y., Sun, I. W., Liu, S. I., Loh, E. W. & Lin, Y. C. Tacrolimus ointment-induced relapse of schizophrenia: a case report. Int. J. Neuropsychopharmacol. 10, 851–854 (2007).
Angot, E. & Brundin, P. Dissecting the potential molecular mechanisms underlying α-synuclein cell-to-cell transfer in Parkinson’s disease. Parkinsonism Relat. Disord. 15, S143–S147 (2009).
Chandra, R., Hiniker, A., Kuo, Y. M., Nussbaum, R. L. & Liddle, R. A. α-Synuclein in gut endocrine cells and its implications for Parkinson’s disease. JCI Insight 2, e92295 (2017).
Amorim Neto, D. P. et al. Akkermansia muciniphila induces mitochondrial calcium overload and α-synuclein aggregation in an enteroendocrine cell line. iScience 25, 103908 (2022).
Chandra, R. et al. Gut mucosal cells transfer α-synuclein to the vagus nerve. JCI Insight 8, e172192 (2023).
Gustafsson, G. et al. Secretion and uptake of α-synuclein via extracellular vesicles in cultured cells. Cell Mol. Neurobiol. 38, 1539–1550 (2018).
Xie, Y. X. et al. Lysosomal exocytosis releases pathogenic α-synuclein species from neurons in synucleinopathy models. Nat. Commun. 13, 4918 (2022).
Lee, H. J., Patel, S. & Lee, S. J. Intravesicular localization and exocytosis of α-synuclein and its aggregates. J. Neurosci. 25, 6016–6024 (2005).
Emmanouilidou, E. & Vekrellis, K. Exocytosis and spreading of normal and aberrant α-synuclein. Brain Pathol. 26, 398–403 (2016).
Abounit, S. et al. Tunneling nanotubes spread fibrillar α‐synuclein by intercellular trafficking of lysosomes. EMBO J. 35, 2120–2138 (2016).
Dieriks, B. V. et al. α-synuclein transfer through tunneling nanotubes occurs in SH-SY5Y cells and primary brain pericytes from Parkinson’s disease patients. Sci. Rep. 7, 42984 (2017).
Rostami, J. et al. Human astrocytes transfer aggregated alpha-synuclein via tunneling nanotubes. J. Neurosci. 37, 11835–11853 (2017).
Scheiblich, H. et al. Microglia jointly degrade fibrillar alpha-synuclein cargo by distribution through tunneling nanotubes. Cell 184, 5089–5106.e21 (2021).
Athauda, D. & Foltynie, T. The glucagon-like peptide 1 (GLP) receptor as a therapeutic target in Parkinson’s disease: mechanisms of action. Drug Discov. Today 21, 802–818 (2016).
Manfready, R. A. et al. Attenuated postprandial GLP-1 response in Parkinson’s disease. Front. Neurosci. 15, 660942 (2021).
Meissner, W. G. et al. Trial of Lixisenatide in early Parkinson’s disease. N. Engl. J. Med. 390, 1176–1185 (2024).
Aviles-Olmos, I. et al. Exenatide and the treatment of patients with Parkinson’s disease. J. Clin. Investig. 123, 2730–2736 (2013).
Athauda, D. et al. Exenatide once weekly versus placebo in Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet 390, 1664–1675 (2017).
McGarry, A. et al. Safety, Tolerability, and Efficacy of NLY01 in Early Untreated Parkinson’s Disease: A Randomised, Double-Blind, Placebo-Controlled Trial. Articles Lancet Neurol 23 www.thelancet.com/neurology (2024).
Kalinderi, K., Papaliagkas, V. & Fidani, L. GLP-1 receptor agonists: a new treatment in Parkinson’s disease. Int. J. Mol. Sci. 25, 3812 (2024).
Cox, H. M. et al. Peptide YY is critical for acylethanolamine receptor Gpr119-induced activation of gastrointestinal mucosal responses. Cell Metab. 11, 532–542 (2010).
Goldspink, D. A., Reimann, F. & Gribble, F. M. Models and tools for studying enteroendocrine cells. Endocrinology 159, 3874–3884 (2018).
Reimann, F. et al. Glucose sensing in L cells: a primary cell study. Cell Metab. 8, 532–539 (2008).
Habib, A. M. et al. Overlap of endocrine hormone expression in the mouse intestine revealed by transcriptional profiling and flow cytometry. Endocrinology 153, 3054–3065 (2012).
Verhoeckx, K. et al. The impact of food bioactives on health: In Vitro and Ex Vivo Models [Internet]. Cham (CH): Springer; 2015. https://doi.org/10.1007/978-3-319-16104-4.
Kuhre, R. E. et al. Peptide production and secretion in GLUTag, NCI-H716, and STC-1 cells: A comparison to native L-cells. J. Mol. Endocrinol. 56, 201–211 (2016).
Martinez-Silgado, A. et al. Differentiation and CRISPR-Cas9-mediated genetic engineering of human intestinal organoids. STAR Protoc. 3, 101639 (2022).
Clevers, H. Modeling development and disease with organoids. Cell 165, 1586–1597 (2016).
Clarke, L. L. A guide to ussing chamber studies of mouse intestine Clarke LL. A guide to Ussing chamber studies of mouse intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 296, 1151–1166 (2009).
Westerhout, J. et al. A new approach to predict human intestinal absorption using porcine intestinal tissue and biorelevant matrices. Eur. J. Pharm. Sci. 63, 167–177 (2014).
Hayashi, M. et al. Enteroendocrine cell lineages that differentially control feeding and gut motility. Elife 12, e78512 (2023).
Mellitzer, G. et al. Loss of enteroendocrine cells in mice alters lipid absorption and glucose homeostasis and impairs postnatal survival. J. Clin. Investig. 120, 1708–1721 (2010).
Wallace, K. N., Akhter, S., Smith, E. M., Lorent, K. & Pack, M. Intestinal growth and differentiation in zebrafish. Mech. Dev. 122, 157–173 (2005).
Kuil, L. E., Chauhan, R. K., Cheng, W. W., Hofstra, R. M. W. & Alves, M. M. Zebrafish: A Model Organism for Studying Enteric Nervous System Development and Disease. Front. Cell Dev. Biol. 8, 629073 (2021).
Gao, J. et al. Dietary L-Glu sensing by enteroendocrine cells adjusts food intake via modulating gut PYY/NPF secretion. Nat. Commun. 15, 3514 (2024).
Guo, X., Lv, J. & Xi, R. The specification and function of enteroendocrine cells in Drosophila and mammals: a comparative review. FEBS J. 289, 4773–4796 (2022).
Xia, Q. et al. PARP-1 inhibition rescues short lifespan in hyperglycemic C. elegans and improves GLP-1 secretion in human cells. Aging Dis. 9, 17–30 (2018).
Gadgaard, S. et al. Long-acting agonists of human and rodent GLP-2 receptors for studies of the physiology and pharmacological potential of the GLP-2 system. Biomed. Pharmacother. 160, 114383 (2023).
Reiner, J. et al. Dapiglutide, a novel dual GLP-1 and GLP-2 receptor agonist, attenuates intestinal insufficiency in a murine model of short bowel. J. Parenter. Enter. Nutr. 46, 1107–1118 (2022).
Cho, W., Kim, S. & Park, Y. G. Towards multiplexed immunofluorescence of 3D tissues. Mol. Brain 16, 37 (2023).
Diefenbach, A., Gnafakis, S. & Shomrat, O. Innate lymphoid cell-epithelial cell modules sustain intestinal homeostasis. Immunity 52, 452–463 (2020).
Beumer, J. et al. Mapping prohormone processing by proteases in human enteroendocrine cells using genetically engineered organoid models. Proc. Natl Acad. Sci .USA 119, e2212057119 (2022).
Afroze, S. et al. The physiological roles of secretin and its receptor. Ann. Transl. Med 1, 29 (2013).
Markovic, M. A. & Brubaker, P. L. The roles of glucagon-like peptide-2 and the intestinal epithelial insulin-like growth factor-1 receptor in regulating microvillus length. Sci. Rep. 9 (2019).
Cekic, C. et al. Evaluation of the relationship between serum ghrelin, C-reactive protein and interleukin-6 levels, and disease activity in inflammatory bowel diseases. Hepatogastroenterology 61, 1196–1200 (2014).
Epelboym, I. & Mazeh, H. Zollinger-Ellison syndrome: classical considerations and current controversies. Oncologist 19, 44–50 (2014).
Modlin, I. M., Lye, K. D. & Kidd, M. Carcinoid tumors of the stomach. Surg. Oncol. 12, 153–172 (2003).