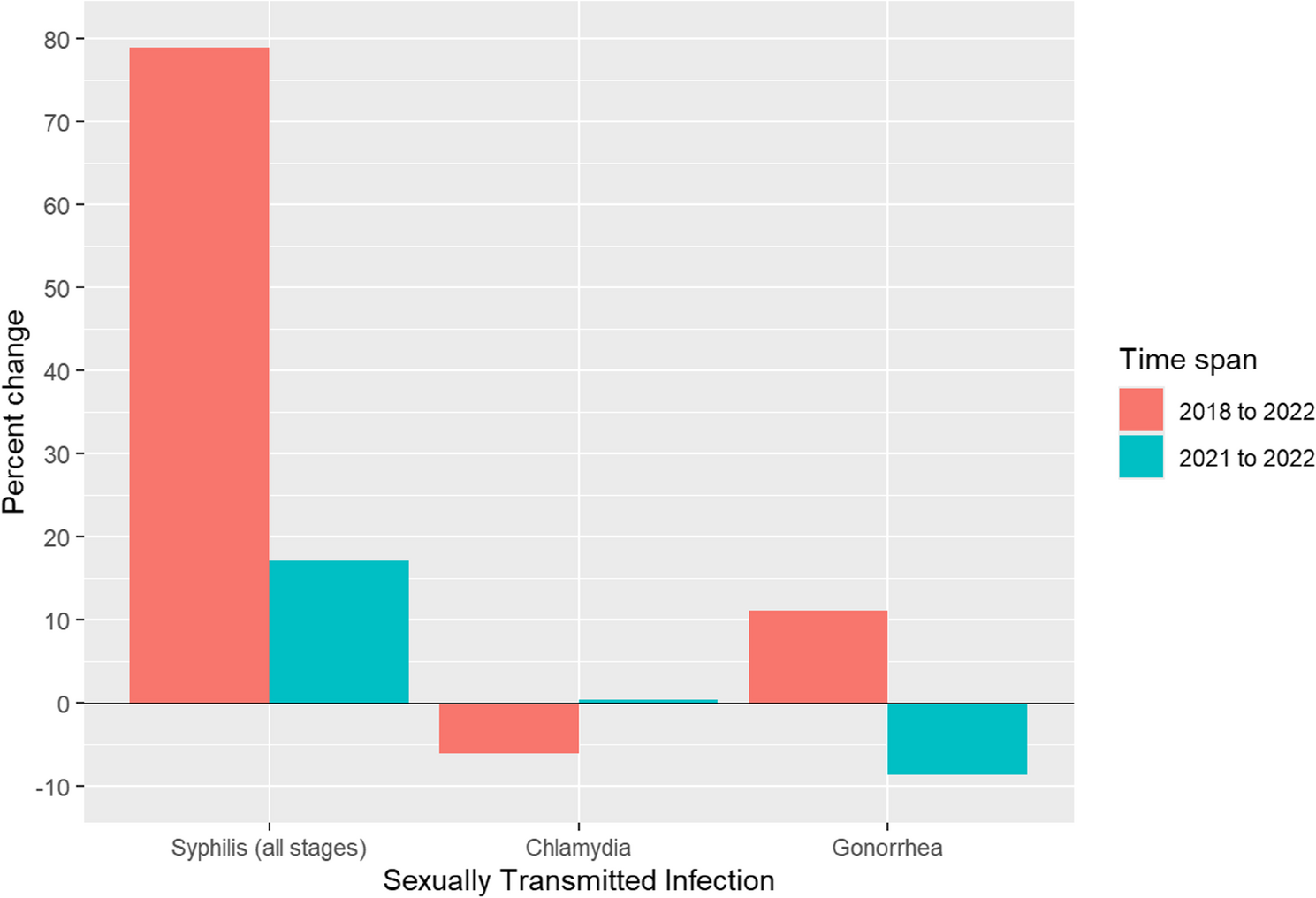
The resurgence of syphilis in the United States represents a growing public health crisis, driven by a complex interplay of social, structural, and behavioral determinants. Despite existing prevention efforts, including condom distribution and sex education programs, syphilis rates have risen sharply over the past five years, underscoring the limitations of current strategies in addressing this evolving epidemic [6]. These trends reflect a growing public health challenge, particularly in light of the resurgence of syphilis, and emphasize the need for enhanced surveillance, outreach, and intervention strategies.
Geographic and racial disparities were prominent, with the highest rates of syphilis reported in the Midwest and Southern regions, particularly in rural states like South Dakota, New Mexico, and Oklahoma. The identification of geographic hotspots for syphilis suggests potential disparities in healthcare access, public health infrastructure, and preventive services, particularly in rural and underserved areas. These findings underscore the need for targeted interventions that account for regional variations in resource availability, healthcare delivery, and social determinants of health. Our analysis shows that American Indian/Alaska Native (AI/AN) individuals were the most affected racial and ethnic group. In South Dakota, where AI/AN individuals make up a large proportion of the population, data indicate that this group accounted for a majority of syphilis cases during the resurgence [7, 8]. These patterns highlight the persistent healthcare disparities experienced by certain racial and ethnic groups, which may contribute to elevated rates of STIs. These areas face longstanding barriers to healthcare access, such as provider shortages, transportation limitations, and reduced availability of STI screening and treatment services [9, 10]. American Indian/Alaska Native (AI/AN) and Black/African American populations were disproportionately affected, reflecting historical and systemic inequities shaped by poverty, limited healthcare access, and systemic racism within healthcare delivery [11,12,13,14]. Strengthening partnerships with Indigenous-led healthcare organizations, expanding mobile clinics, and leveraging telemedicine services may help mitigate these barriers and improve access to STI prevention and care in high-burden communities. Previous community-engaged interventions, particularly in HIV prevention, have demonstrated the effectiveness of culturally tailored public health campaigns in improving testing uptake and reducing transmission in underserved populations [15, 16]. Such community-centered approaches should be applied to syphilis prevention efforts to ensure cultural relevance and trust-building within affected populations.
The widening disparities by sex and age highlight the need to expand prevention efforts beyond traditionally targeted populations. While males continue to bear a higher burden of syphilis, the near doubling of cases among females over the study period is concerning and may reflect under-testing, healthcare access barriers, and evolving behavioral risk patterns [17]. The marked increase in syphilis rates among individuals of reproductive age, particularly women of childbearing potential, likely contributed to the concurrent rise in congenital syphilis cases during this period. Integrating syphilis screening into routine reproductive health services, including prenatal care, and expanding outreach to women in high-burden areas should be prioritized.
Behavioral and substance use factors remain central drivers of syphilis transmission. High-risk sexual behaviors, including anonymous sex and sex while intoxicated or high on drugs, were significantly associated with increased odds of infection. One relevant consideration is the concept of “undetectable equals untransmissible” (U = U), which has gained prominence in the past decade as antiretroviral therapy has significantly improved viral suppression in people living with HIV [18]. As awareness and adoption of U = U have increased, some studies suggest a corresponding decline in condom use among individuals with HIV [18]. This behavioral shift may partially explain rising syphilis rates, particularly among men who have sex with men (MSM), individuals engaging in sex with anonymous partners, those using certain illicit drugs, and specific racial and ethnic groups. Additionally, methamphetamine use demonstrated the strongest association with syphilis, aligning with prior research linking stimulant use to increased sexual risk behaviors, particularly among men who have sex with men (MSM) [19]. Integrating STI prevention into harm reduction programs, including syringe service programs and substance use treatment services, is critical. Such approaches have been effective in reducing HIV and HCV transmission and should be adapted to address syphilis as well [15]. These findings indicate that while syphilis prevalence is increasing overall, the rate and intensity of this rise vary across demographic groups, reflecting underlying structural inequities and persistent barriers to care.
Beginning in 2020, syphilis rates stratified by sex, sexual behaviors, and substance use increased markedly compared to the period between 2018 and 2020. This surge aligns with the onset of the COVID-19 pandemic, which may have contributed to increased STI transmission due to social isolation, higher substance use, elevated engagement in high-risk sexual behaviors, and reduced access to healthcare services [20, 21]. Numerous studies have suggested that disruptions in diagnosis and treatment, resulting from the reallocation of healthcare resources during the pandemic, may have played a role in this increase [20, 21]. While more research is needed to establish a causal relationship, the temporal correlation between the COVID-19 pandemic and the rise in syphilis is notable.This study is not without limitations. Due to the constraints of the CDC dataset, key confounders such as socioeconomic status, education level, and healthcare access could not be directly assessed. The surveillance data used were derived from clinic-based reporting, which is subject to variability. Previous studies have identified underreporting of STIs and race/ethnicity data in private clinics compared to public health settings, potentially impacting the accuracy and completeness of surveillance data [22].Testing bias may also influence the interpretation of syphilis trends. For example, a retrospective analysis of patients seeking STI care found that men were more likely than women to receive comprehensive testing and to engage in additional preventive services such as HIV screening and risk-reduction counseling [22]. These patterns may help explain why men appear disproportionately affected, even as congenital syphilis rates continue to rise. In addition, research has shown racial disparities in STI testing practices, with Black individuals more likely to be tested for STIs compared to White individuals [16]. These biases should be taken into account when interpreting the observed disparities.
The recent shortage of benzathine penicillin G (BPG), the first-line treatment for syphilis, poses an additional barrier to disease control efforts [23]. Ensuring a stable and equitable supply of essential STI medications must be a public health priority, as treatment delays may lead to ongoing transmission and adverse health outcomes [24]. National policies aimed at strengthening the STI medication supply chain and creating reserve stockpiles could mitigate the impact of future shortages. Finally, improvements in STI surveillance infrastructure are urgently needed. Standardizing and improving the collection of race and ethnicity data, particularly in private healthcare settings, will enable more accurate monitoring of disparities and better allocation of resources [22, 25]. Targeted public health campaigns, such as the CDC’s successful “Get Yourself Tested” (GYT) initiative, have demonstrated the potential for increasing STI testing rates among youth and marginalized populations [26]. Leveraging similar culturally tailored, community-informed campaigns could enhance syphilis prevention efforts nationally.