This study was conducted in Tongliao City, Inner Mongolia, a region characterized by its unique geographical and economic profile. Tongliao City is situated in a semi-arid climate zone, with vast grasslands and limited industrial development. The region faces challenges in terms of economic development, infrastructure, and access to specialized healthcare services. These characteristics contribute to its status as a resource-limited setting, where the delivery of comprehensive mental health care, particularly for conditions like dementia, is constrained. This study makes a significant contribution to the existing literature by specifically examining the association between cognitive domains and suicidal ideation in older adults with mild dementia in a resource-limited setting. Our findings highlight the crucial role of the judgment domain in suicidal ideation, providing new insights into targeted interventions that could be particularly effective in regions with limited healthcare resources.
Our findings demonstrate that mild dementia is associated with a 3.37-fold increased odds for suicidal ideation compared to non-dementia individuals, even after controlling for anxiety and depressive mood. Importantly, the study reveals that anxiety emerged as the factor most strongly associated with suicidal ideation (OR = 18.02), followed by depression (OR = 7.87), while among cognitive domains, impairment in judgment and problem-solving emerges as the most strongly associated cognitive factor (OR = 3.44), aligning with recent evidence from multiple populations. One study similarly identified dysfunctional cognitive control, executive function, and problem-solving as key risk factors for attempted suicide in older people [22]. Another study demonstrated that executive dysfunction is associated with approximately seven times higher odds of suicide ideation in older adults, independent of depression, particularly in those living in disadvantaged environments, a finding highly relevant to our resource-limited setting in Tongliao City [26]. While some studies emphasize different domains, research has found that depressed patients with recent suicide attempts showed poorer executive function performance compared to both lifetime attempters and non-attempters [13]. The consistency of judgment and executive function impairments across diverse populations strengthens our conclusion that these domains represent critical intervention targets. These converging findings suggest that judgment and executive functions serve as a ‘cognitive buffer’ against suicidal behavior [7]. When this buffer is compromised through dementia-related deterioration, individuals become more vulnerable to suicidal thoughts, particularly under conditions of interpersonal stress. This vulnerability is further amplified by factors such as awareness of cognitive decline and anticipated loss of autonomy [9].
The neurobiological basis of judgment impairment is further substantiated by evidence linking orbitofrontal cortex (OFC) degeneration to decision-making deficits [20]. The OFC maintains crucial connections with limbic structures including the amygdala and anterior cingulate cortex, forming circuits essential for emotional regulation and value-based decision-making [11]. In dementia, disruption of these OFC-limbic circuits compromises both cognitive control and emotional processing, particularly affecting the ventromedial prefrontal cortex’s role in evaluating future consequences [30]. This neural degradation impairs the ability to anticipate the consequences of suicidal acts, thus lowering the threshold for ideation. In the cultural context of Tongliao City, traditional family values and social roles play a significant part in the psychological well-being of older adults. The region’s strong emphasis on family decision-making and moral authority means that cognitive decline, particularly in judgment, can have profound psychological consequences. This cultural backdrop may exacerbate feelings of isolation and distress among older adults, contributing to an increased association with suicidal ideation.
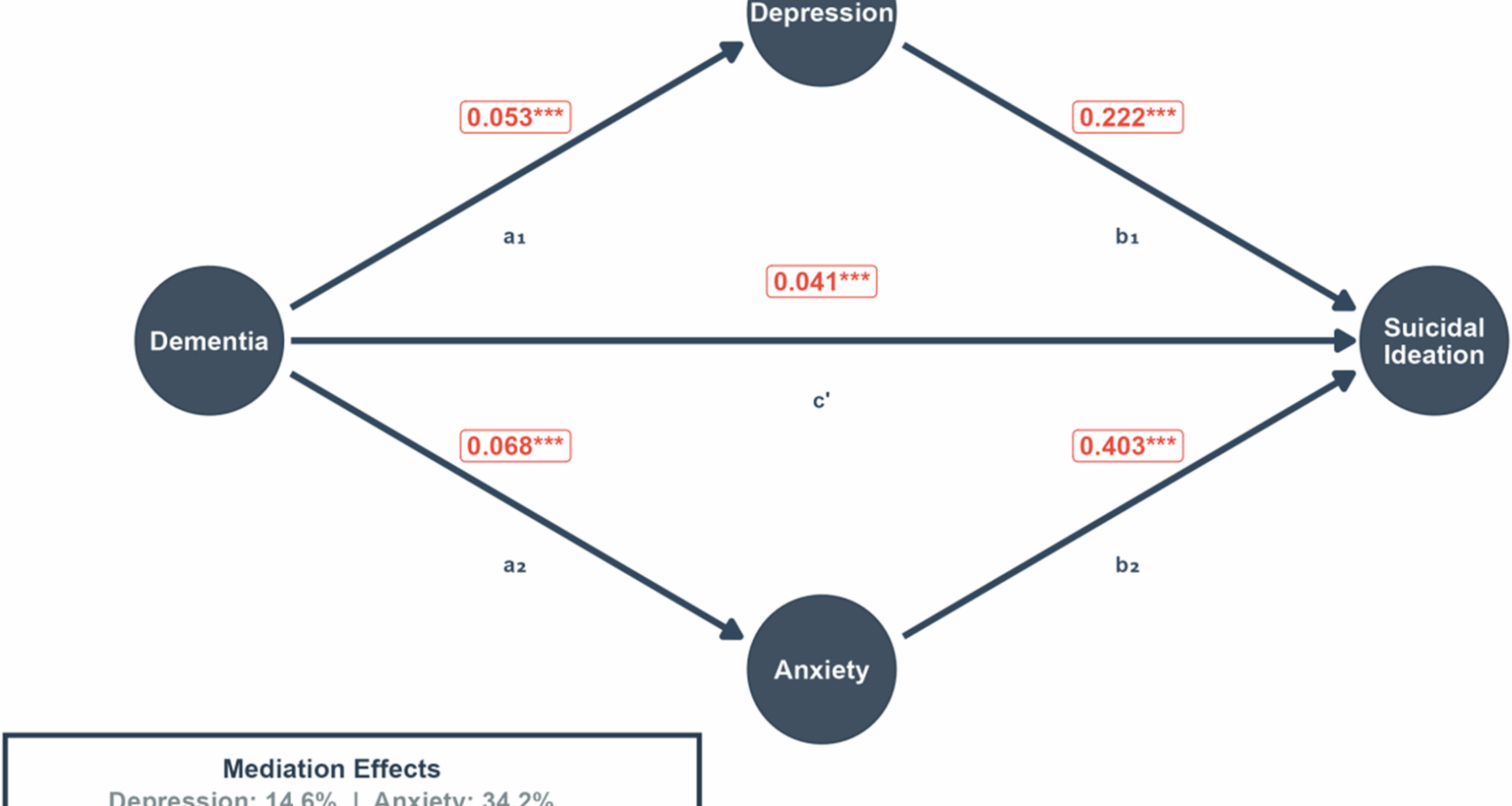
Our study reveals that cognitive factors, particularly judgment impairment, maintain independent associations with suicidal ideation even after controlling for anxiety and depression. Our mediation analysis reveals that anxiety and depressive mood together account for 48.8% of the relationship between dementia and suicidal ideation, with anxiety contributing more substantially (34.2%) than depression (14.6%). This finding challenges the traditional focus on depression as the primary emotional pathway and highlights anxiety as a potentially more critical factor in the dementia-suicide relationship. The prominence of anxiety in our findings aligns with emerging research suggesting that anxiety disorders are highly prevalent in dementia and may be more directly linked to cognitive awareness and anticipatory distress about functional decline. Unlike depression, which may develop as a reactive response to loss, anxiety in dementia often reflects the individual’s preserved insight into their declining capabilities and uncertain future. This distinction has important implications for intervention strategies, as anxiety-focused interventions may need to address cognitive concerns and uncertainty management, while depression interventions may focus more on mood regulation and behavioral activation. The remaining 51.2% of the association suggests that other factors, particularly cognitive impairments including judgment deficits, play crucial roles in the dementia-suicide relationship. This suggests that while emotional symptom management is crucial, cognitive-focused interventions should be integrated with, rather than secondary to, emotional symptom management.
From a public health perspective, integrating judgment domain evaluations into routine dementia care protocols is crucial. Regular screenings should be prioritized for patients, particularly in resource-limited settings like Tongliao City, where healthcare access may be limited. Additionally, family-centered training programs that include role-playing modules on collaborative decision-making can help alleviate the pressure placed on elderly individuals with dementia. These training programs should be designed to help families understand the importance of adjusting expectations and reframing elders’ roles as “consultants” rather than primary decision-makers.
Given the strong associations of anxiety with suicidal ideation in our study, screening protocols should give equal, if not greater, attention to anxiety symptoms alongside traditional depression screening. Anxiety management interventions, including cognitive-behavioral therapy adapted for mild cognitive impairment, mindfulness-based stress reduction, and pharmacological approaches when appropriate, should be integrated into comprehensive care plans.
Community health systems should also focus on training village health workers to identify signs of judgment decline and anxiety symptoms and establish clear referral pathways to connect affected patients with appropriate mental health services and support. Such community-based initiatives could be pivotal in reducing suicidal ideation in resource-limited settings like Tongliao City, where access to specialized care may be limited.
While this study provides valuable insights, several limitations should be acknowledged and addressed in future research. The cross-sectional design precludes causal inferences, necessitating longitudinal studies that track the evolving relationship between cognitive decline and suicidal ideation over time, potentially using structural equation modeling. Our study did not comprehensively examine mediating factors; thus, future research should explore the roles of social support systems, family dynamics, quality of life, and psychological factors such as impulsivity and emotional dysregulation. Dimensional measures of depression severity, cognitive impairment, and suicidal intent are needed to examine dose–response relationships for more nuanced risk stratification. Given the distinct neuropathological features of different dementia subtypes, examining whether judgment impairment and suicidal ideation vary across these subtypes would be valuable. Additionally, qualitative interviews with patients and caregivers should complement quantitative approaches to reveal subjective experiences of cognitive decline and its impact on suicidal thoughts. Finally, developing and testing culturally tailored interventions, particularly those targeting judgment enhancement and emotional symptoms management, would be crucial in resource-limited settings like Tongliao City and other diverse cultural contexts.
In conclusion, this study establishes that judgment domain impairment plays a crucial and independent role in suicidal ideation among mild dementia patients. While emotional symptoms, particularly anxiety, show the strongest overall associations and mediate nearly half (48.8%) of the dementia-suicide relationship, cognitive factors—especially judgment impairment—account for the remaining association. These findings have important implications for clinical practice and public health policy, particularly in rapidly aging societies like China. Interventions targeting both cognitive function and emotional symptom management are urgently needed to address factors associated with suicide ideation among older adults with dementia. Further research should focus on developing and validating interventions specifically targeting judgment enhancement and anxiety management, while considering the cultural context of caregiving and dementia in resource-limited settings of China.