Mental health is a crucial component of overall well-being, encompassing an individual’s psychological, emotional, and social state. Despite its importance, mental health conditions are increasingly prevalent worldwide, particularly among young adults such as university students. These conditions pose significant public health challenges, often resulting in impaired academic performance, social isolation, and heightened suicide risks. The university environment can be uniquely stressful, as students often face pressures related to academic performance, future career uncertainty, and adapting to new social networks. This study addresses a gap in the existing literature by comprehensively examining the factors associated with depression, anxiety, and stress among Bangladeshi university students, using an integrated approach that combines traditional statistical methods with advanced machine learning techniques. The study’s unique contribution lies in its identification of risk factors, including gender, family relationships, academic pressures, and substance use, and the application of machine learning models (CatBoost, XGBoost, SVM, RF, KNN, LR, and GBM) to predict mental health risks. By integrating both conventional and advanced machine learning approaches, our findings offer a more comprehensive understanding of mental health risk in this population and highlight the value of multidisciplinary research in this area. The findings from this study will inform the development of targeted interventions and policies to improve student well-being in Bangladesh and similar low- and middle-income countries.
The prevalence of mental health conditions among the study participants was notable, with 56.9% experiencing depression, 69.5% anxiety, and 32.2% stress. These rates are generally higher than those reported in previous studies conducted in other countries, such as the USA (depression 22%) [5], China (depression 23.45%) [8], Malaysia (depression 29%) [9], Spain (depression 18.4% vs. anxiety 23.6% vs. stress 34.5%) [10], except in discordant findings in Pakistan (anxiety 88.4% vs. depression 75%) [4]. Among the university students. In the context of Bangladesh, previous studies conducted during the COVID-19 pandemic reported depression, anxiety, and stress prevalence rates ranged from 46.92 to 82.4%, 26.6–96.82%, and 28.5–70.1% [41,42,43,44,45]. These findings align more closely with those of the present study, suggesting a possible pandemic-related impact on the mental health of university students. Moreover, these high prevalence rates might reflect ongoing social and academic pressures, limited mental health resources, and cultural factors that may discourage help-seeking behaviors. Furthermore, a meta-analysis on mental health problems during the COVID-19 pandemic in Bangladesh revealed pooled prevalence rates of 47% for depression, 47% for anxiety, and 44% for stress [27]. These figures not only reinforce the high burden of psychological distress in Bangladeshi populations during and after the pandemic but also contextualize the elevated rates observed in our current study.
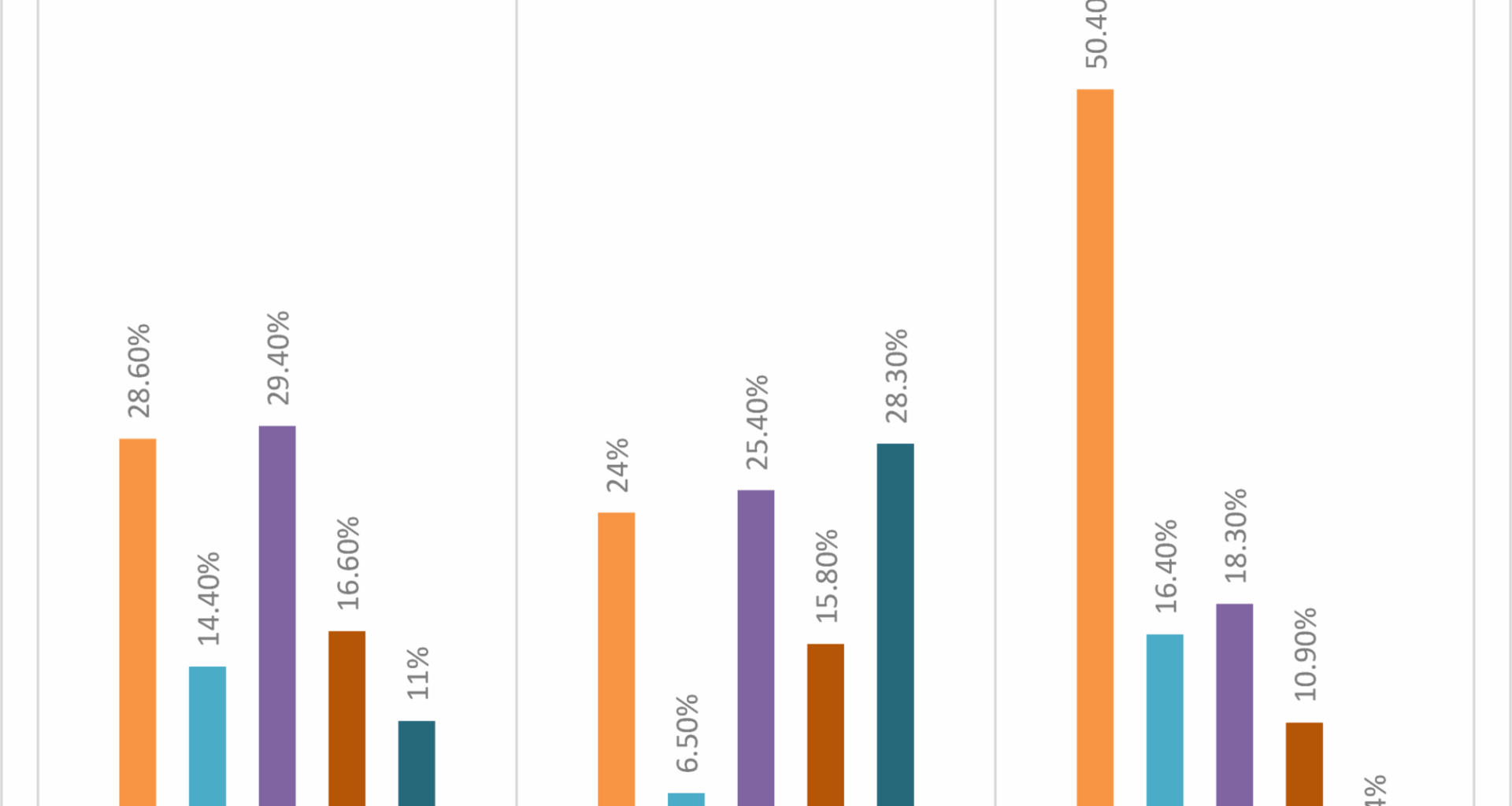
The gender-based comparison in this study aligns with previous research [10, 46], indicating that females were more likely to exhibit higher levels of depression and stress than their male counterparts. This finding is consistent with the broader literature reporting women’s vulnerability to anxiety and depression [47, 48]. Previous epidemiological studies have also suggested that females are more prone to psychological symptoms than male students [48,49,50]. Factors contributing to the higher prevalence of mental health conditions in women may include the heavy academic workload [50], academic pressure [51], and limited job opportunities compared to males. Additionally, women may experience greater societal expectations and restrictions, which can contribute to chronic stress and exacerbate underlying vulnerabilities to mental health problems. The social and intellectual challenges encountered during higher education can exacerbate emotional strain, potentially leading to the manifestation of mental health issues [52]. These stressors and societal challenges faced by female students may explain the higher rates of mental health conditions observed in the current study. In contrast, one study reported a higher prevalence of depression among male students than female students [53]. This difference suggests that gender-related mental health risks may be influenced by complex interactions between personal, academic, and cultural factors.
A notable finding of this study pertains to familial relationships and their association with mental health outcomes. Participants who reported having an unfriendly or strained relationship with their family exhibited significantly higher levels of depression, anxiety, and stress. This aligns with prior research, such as a study conducted among Jordanian students, which found that positive family functioning was inversely associated with these mental health conditions [54]. These findings are further supported by other literature highlighting the critical role of family support in fostering psychological well-being [46]. In the context of Bangladesh, where family plays a central role in students’ emotional and social lives, strained relationships may contribute to a sense of isolation and a lack of coping resources. This study expands upon this body of work by emphasizing that poor familial relationships are a contributing factor to mental health problems. Consequently, interventions aimed at improving family dynamics may serve as an effective strategy for mitigating these issues. This association is particularly salient within the context of Bangladeshi culture, where family plays a central role in the emotional and social lives of individuals, thereby significantly influencing mental health outcomes. A lack of emotional support from family may foster a sense of isolation, further exacerbating psychological distress among young people. This is consistent with other studies that have shown limited familial and community engagement to be predictive of adverse mental health outcomes [55]. Universities may benefit from engaging families through mental health education and outreach programs, fostering supportive networks beyond the campus.
The present study found that depression and anxiety, but not stress, were significantly associated with students’ academic disciplines. Students from commerce faculties reported the highest prevalence of depression (73.9%) and anxiety (69.7%) compared to those in other faculties, which is in line with a previous study reporting similar patterns [12]. Additionally, another study suggests that concerns such as perceived career uncertainty and feelings of personal inefficacy are commonly expressed by students in these disciplines [56], which may be relevant in interpreting these findings. The higher rates of distress in commerce students may reflect worries about employment prospects, economic instability, and intense competition in the job market. In terms of academic year, a significant association was observed with stress, but not with depression or anxiety. Third-year students reported the highest stress levels (41.4%), while first-year students reported the lowest (32.3%). This observation is consistent with earlier research indicating that academic demands and workload may increase throughout university education, possibly contributing to elevated stress levels in later years [57, 58]. Support programs for students in advanced academic years, such as mentorship and academic counseling, may help to alleviate these stressors and reduce risk. However, no significant association was observed between mental health outcomes and socioeconomic status in this study. This contrasts with findings from previous studies that often report lower and higher socioeconomic status as a risk factor for mental conditions [59]. The relatively homogenous background of the current sample, mainly comprising university students, may have limited the variability needed to detect such associations. It is also possible that strong peer networks or campus resources may buffer the impact of socioeconomic differences within this group.
The overall findings of this study indicated significant associations between health and behavioral risk factors and mental health outcomes. Specifically, substance use behaviors, including cigarette smoking, illicit drug use, and alcohol consumption, were significantly associated with symptoms of depression and anxiety. These results are in line with a substantial body of literature demonstrating links between substance use and mental health issues. For example, prior research has reported that heavy use of alcohol and drugs is associated with increased risks of depression, anxiety, and cognitive impairment among adolescents and young adults [60]. Psychologically, some students may use substances as a way of coping with academic or emotional stress, but this may in turn aggravate mental health issues, creating a vicious cycle. The current findings contribute to this growing body of evidence by documenting similar patterns within a Bangladeshi university student population. The observed comorbidity between mental health conditions and substance use may be interpreted in light of both biological and psychosocial frameworks. Some studies have suggested that substance use may influence brain chemistry in ways that exacerbate symptoms of anxiety and depression, while others point to the potential for individuals with pre-existing mental health concerns to engage in substance use as a form of self-medication [60]. In the context of cigarette smoking, the relationship appears to be bidirectional, with mental health challenges potentially leading to smoking as a coping strategy, and smoking itself possibly contributing to worsening psychological symptoms [61,62,63]. Prevention and intervention programs should consider this complex interplay and incorporate both mental health promotion and substance use prevention as integrated strategies for university students. These findings highlight the need for integrated approaches that address both substance use and mental health among young people. Including smoking cessation and substance use prevention as components of mental health interventions could be particularly relevant for university students in Bangladesh.
The application of machine learning techniques in the current study offered an additional layer of analysis to identify patterns associated with depression, anxiety, and stress among university students. SVM demonstrated the best performance for depression, achieving the highest accuracy (56.93%) and precision (75.60%), while also exhibiting a relatively low log loss (0.6847). In contrast, KNN performed the worst in depression, with the lowest accuracy (48.79%) and precision (53.35%). However, SVM showed strong results for anxiety, with an impressive accuracy (69.48%) and precision (78.81%), making it one of the top performers in this category. Similarly, LR performed decently in both anxiety, achieving relatively high accuracy and log loss scores across all models. For stress, CatBoost was particularly noteworthy, achieving the highest accuracy (67.06%) and precision (64.54%), while RF and XGBoost showed promising results in stress prediction, particularly in terms of log loss (0.6369 and 0.6305, respectively). Overall, SVM, RF, and CatBoost emerged as the top contenders in predicting depression, anxiety, and stress. These findings underscore the variability in model performance across different mental health outcomes, with no single model consistently outperforming others across all metrics. Its effectiveness may be attributed to its algorithmic strengths in handling categorical variables and reducing overfitting, as supported by existing literature [64]. These results indicate that, while machine learning can add value in identifying students at risk for poor mental health, predictive accuracy is still limited, possibly due to the complexity of mental health determinants and the available data. Despite these observations, receiver operating characteristic analysis revealed that the discriminative ability of all models was limited, with area under the curve values not exceeding 0.54 for any of the mental health outcomes. These results suggest that the predictive capacity of the models remains modest, potentially due to the complex and multifactorial nature of mental health conditions, which may not be fully captured by the available feature set. Future studies could benefit from incorporating additional features, such as digital behavioral markers or longitudinal data, to improve model performance. Nevertheless, the k-nearest neighbors algorithm yielded the highest F1 scores across outcomes, indicating a relatively balanced trade-off between precision and recall in classifying individuals with varying mental health symptomatology.
Feature importance analyses offered valuable insights into the most influential predictors. For instance, CatBoost identified cigarette smoking status as a key predictor across outcomes, whereas XGBoost highlighted relationship quality with family (feature importance = 1.30) as a significant correlate. These findings are consistent with earlier literature emphasizing the role of behavioral and psychosocial factors in mental health risk among youth. The integration of SHAP (SHapley Additive exPlanations) values further enhanced model interpretability, revealing feature-specific contributions to prediction and reinforcing the context-specific relevance of certain variables within the Bangladeshi student population. When benchmarked against international studies, such as the work by Zhai et al. [65], which achieved notably higher AUC values (0.74–0.77) by incorporating contextual socioeconomic and environmental variables in a large U.S. student cohort, the current models demonstrated comparatively limited performance. This discrepancy may highlight the need for a broader set of features, including dynamic or time-sensitive variables such as financial insecurity, academic stress trajectories, or campus support engagement, to better capture the complex determinants of mental health outcomes. Furthermore, differences in data collection methods, sample composition, and cultural context may contribute to the observed differences in model performance, emphasizing the need for context-specific model development and validation.
In recent years, several ML studies in Bangladesh have focused on predicting mental health outcomes among university students, particularly concerning depression, anxiety, and stress. For example, a study utilized seven machine learning models, such as Random Forest, Support Vector Machine, and Artificial Neural Networks, to analyze data from 750 students and found the RF as the best-performing model achieved an 87% accuracy, 78% precision and 86% f1-score rate in identifying depressive symptoms [66]. Another study implemented machine learning algorithms, including Decision Tree, RF, and SVM, to predict and classify perceived stress and that study identified significant predictors, including pulse rate, diastolic blood pressure, sleep status, and smoking status, where the RF model performs better with 0.8972 accuracy, 0.9241 precision and 0.8715 AUC-ROC [23, 67]. Furthermore, research that concentrated on the prediction of anxiety and depression employed eight machine learning algorithms. RF, Decision Tree, and AdaBoost achieved 100% accuracy and precision, while SVM exhibited the quickest performance time with 0.007 s [67]. The potential for early detection and intervention strategies is underscored by these studies, which emphasize the increasing implementation of ML techniques in mental health research within the Bangladeshi university context. Despite these technological advances, ensuring ethical use, transparency, and user trust in ML-based mental health tools remains a priority for research and practice.
This study’s findings have several important implications for university policy and mental health practice in Bangladesh and similar contexts. The high prevalence of depression, anxiety, and stress among university students—together with the identification of specific risk factors such as unfriendly family relationships, female gender, advanced academic year, and substance use—signals an urgent need for comprehensive and systematic mental health support at the institutional level. Universities should develop and implement evidence-based mental health policies that prioritize routine mental health screening, particularly targeting students with identified risk factors. Such screening could be integrated into regular student health services, orientation programs, or academic advising, enabling early identification and timely intervention for those at risk. The expansion of accessible, confidential, and culturally appropriate on-campus counseling services is also critical, with adequate staffing and training to address the diverse needs of the student population. Establishing structured peer support programs and student-led mental health clubs can further foster a supportive community, reduce stigma, and encourage help-seeking behaviors. Policies should promote collaboration between faculty, administration, and health professionals to ensure that mental health support is embedded across all aspects of campus life. In addition, universities should integrate mental health education into their curricula and co-curricular activities to enhance mental health literacy, resilience, and self-care skills among students. Awareness campaigns and anti-stigma initiatives can create a more open environment for discussing mental health concerns. At a broader policy level, the Ministry of Education and relevant governmental bodies should recognize student mental health as a priority, allocate resources accordingly, and develop national guidelines for university mental health services. Given the demonstrated utility of machine learning models in identifying students at risk for mental health problems, universities and policymakers should consider leveraging data-driven approaches—such as electronic risk assessments and early warning systems—to supplement traditional support mechanisms. Integrating these digital tools, while ensuring privacy and ethical use of student data, could enable more proactive and individualized support. Ultimately, a multi-level approach that combines institutional policy reform, resource allocation, technological innovation, and community engagement is needed to address the mental health crisis among university students in Bangladesh. These strategies can serve as a model for other low- and middle-income countries facing similar challenges in student mental health.
This study highlights the effectiveness of tree-based and boosting machine learning models in predicting mental health outcomes, offering advantages over traditional regression methods by capturing nonlinear relationships and interaction effects among predictors. Such capabilities enhance both the predictive accuracy and interpretability of complex behavioral health data. With a sample size of 1,697 students and balanced outcome classes, the models performed reliably within this context. However, the generalizability of these findings may be limited in studies with smaller or imbalanced datasets, where classification performance could decline. Additionally, as a cross-sectional design was employed, causal inferences cannot be drawn, underscoring the need for future longitudinal studies. The exclusive reliance on self-reported data also raises the potential for response bias; thus, future research should integrate objective measures of mental health. While the machine learning approaches used allowed for the exploration of intricate variable relationships, model interpretability remains a challenge and requires further refinement. Additionally, this study was limited to two public universities (Jahangirnagar University and Patuakhali Science and Technology University), and our sample did not include private universities. Thus, the findings may not be generalizable to students at private institutions, where mental health outcomes and influencing factors may differ [68]. Furthermore, Use of convenience sampling despite stratified quotas means participants were not selected with a known probability, so estimates may be affected by selection and volunteer bias. Coverage was limited to Jahangirnagar University, Dhaka, and Patuakhali Science and Technology University, Patuakhali, and specific recruitment times, potentially under-representing students who were absent, off-campus, or less engaged with classes. Non-response and self-selection may distort associations, and findings should not be generalized to all university students in Bangladesh without caution. Future studies should employ probability-based designs (e.g., multistage cluster sampling from a national or registrar sampling frame with stratification by university type, faculty, and academic year), implement non-response follow-up, and apply post-stratification weights to improve external validity. Future research should include diverse university types to provide a more comprehensive understanding of student mental health across Bangladesh. These findings emphasize the importance of developing targeted interventions addressing familial relationships, substance use, and academic stress to improve youth mental health in Bangladesh.