MD Anderson Research News
October 15, 2025
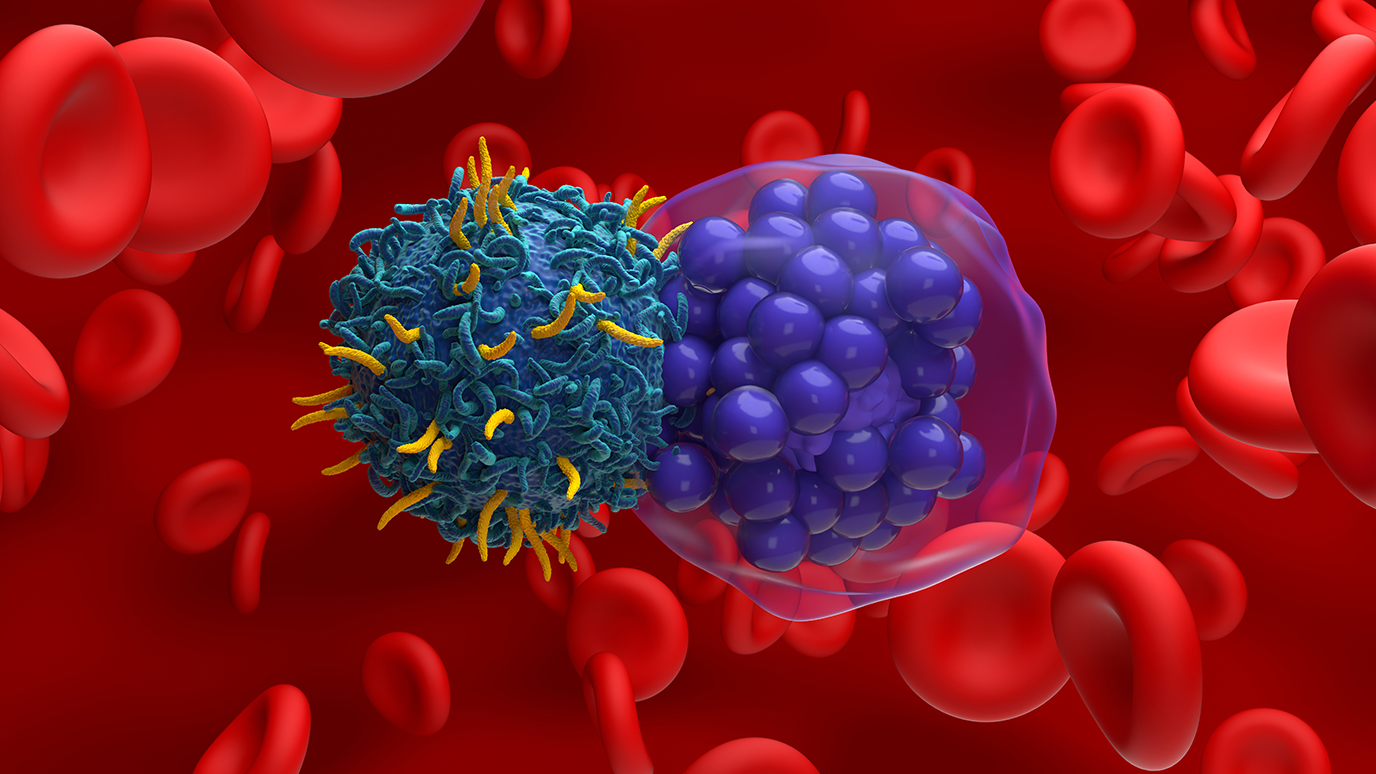
Multiple genetic markers play a key role in the treatment outcomes of patients with large B-cell lymphoma (LBCL) who received chimeric antigen receptor (CAR) T cell therapy, according to a new study from researchers at The University of Texas MD Anderson Cancer Center.
The study, published in the Journal of ImmunoTherapy for Cancer, was led by first author Paolo Strati, M.D., associate professor of Lymphoma/Myeloma, and senior author Michelle Hildebrandt, Ph.D., professor of Lymphoma/Myeloma.
“Our findings provide more insight into how we can select the patients who will benefit the most from CAR T cell therapy,” Strati said. “Understanding the genetic determinants may help in improving developing strategies to enhance CAR T therapy’s efficacy in patients with these markers.”
What are the key findings of this research?
For this study, researchers analyzed the genome of 170 patients who were treated with standard-of-care axicabtagene ciloleucel to identify patterns linked to treatment outcomes.
Patients with a higher polygenic risk score for monocyte count were linked to an increased risk of cytokine release syndrome. Other genetic signals were linked to low blood cell counts and changes in immune-related genes, which may affect recovery and long-term survival.
Importantly, the study identified specific genetic variants associated with better or worse survival outcomes. Few differences were based on ancestry, except for a lower risk of blood cell complications in patients of European descent.
What should patients with large B-cell lymphoma take away from these findings?
These findings suggest that inherited genetic traits can help physicians predict how patients will respond to CAR T cell therapy. In the future, this could lead to more personalized treatment plans that improve safety and effectiveness for patients with LBCL.
++++++
For a full list of collaborating authors and disclosures, see the full paper in the Journal of ImmunoTherapy for Cancer.