Data collecting
This comparative study received ethical approval from the Institutional Review Board of Zhujiang Hospital, Southern Medical University (Protocol No: 2023-KY-164-01), with written informed consent obtained from all participants. Patients requiring single tooth restorations were consecutively enrolled between February 1 and February 28, 2024, meeting the following criteria: presence of intact adjacent teeth, absence of active periodontal disease or carious lesions in adjacent dentition.
Standardized tooth preparations were performed by a single prosthodontist with 10 years’ clinical experience (Wei Li). Digital impressions were acquired using a CEREC Omnicam intraoral scanner (Dentsply Sirona, York, PA, USA) following manufacturer protocols, capturing the prepared tooth surface, adjacent dentition, and opposing arch in maximum intercuspation. CAD designs were created using 3Shape Dental System (v2021.1, 3Shape A/S, Copenhagen, Denmark) by an experienced technician with 7 years’ clinical experience (Bing-ying Xie), incorporating manual margin delineation and occlusal adjustments based on software-guided dynamic analysis.
The selection of cases for this study was governed by stringent success criteria, evaluated at both the delivery appointment and a subsequent 6-month follow-up. At the time of delivery, a restoration was required to demonstrate continuous marginal adaptation, with no palpable catch or step when traced with a dental explorer; appropriate proximal contacts, verified to allow dental floss to pass with tactile resistance; and harmonious occlusion, confirmed with articulating paper (
Studying groups
A paired study design was employed, using the same 30 cases for each of the three experimental groups.
Reference group
The original clinically-approved designs were used as reference.
Manual group
Manual designs created by the same reference technician (Bing-ying Xie) using 3Shape Dental System. The technician imported an initial restoration morphology from the system’s built-in database, then performed comprehensive manual adjustments to the crown’s shape, contacts, and occlusion, based on her clinical experience. These designs employed identical margin tracing and contour adjustment protocols as the original workflow but were executed following completion of the 6-month clinical follow-up period.
AI group
The designs for the AI group were generated using 3Shape Automate (automate.3shape.com), a platform recognized for employing artificial intelligence in automated dental restoration design [8]. All designs were created using the system’s default clinical parameters without any manual intervention. The specific parameters were as follows:
-
Emergence Profile: Regular
-
Contact Shape: Regular
-
Contact Distance: −0.01 mm
-
Occlusal Style: Mature
-
Occlusion Distance: 0.45 mm
-
Undercuts: Allowed
For the purposes of this study, “manual design” refers to a conventional, operator-led workflow where an experienced technician utilizes the software’s standard semi-automated proposals (e.g., for margin line and insertion path) and digital sculpting tools to achieve the final design. “AI-driven design” utilized a fully autonomous generative module (3Shape Automate) that produces a complete proposal in a single step, without intermediate operator input.
Morphological comparison
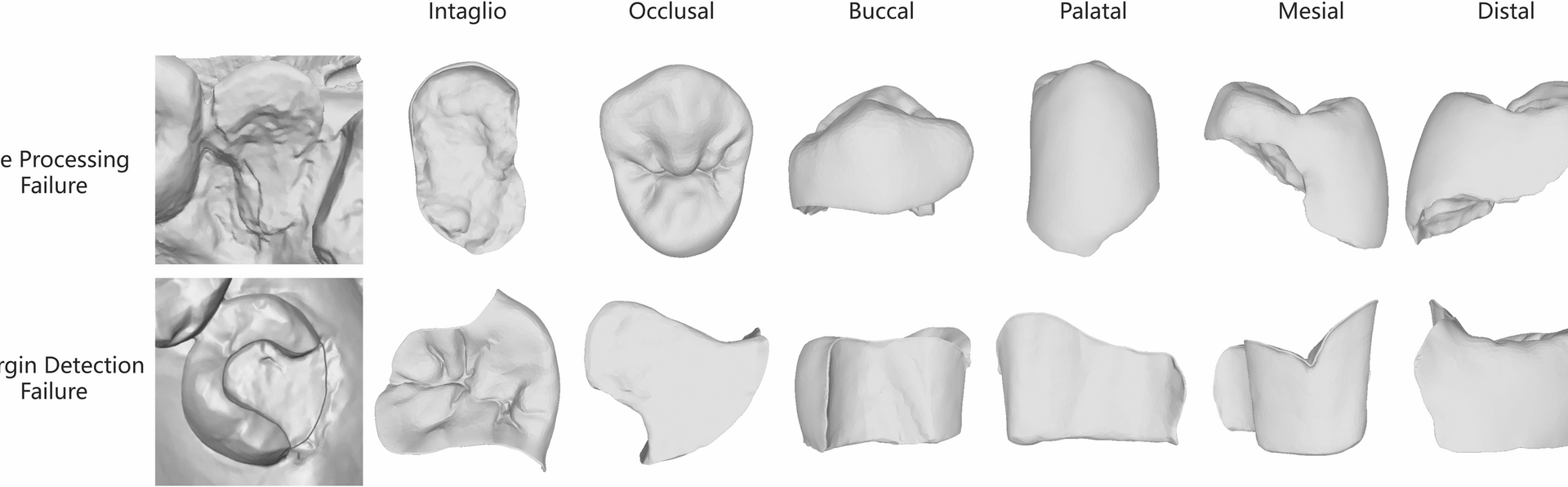
Morphological evaluation was conducted using Geomagic Control X (2018.1.1; 3D Systems, Rock Hill, SC), to quantify the trueness of the AI- and manual- designs against the original, clinically approved design, which served as the reference standard. For each case, three separate CAD design files in STL (Standard Tessellation Language) format were used:
-
The Reference: The original, archived CAD file of the restoration that was clinically delivered and confirmed successful after 6 months.
-
The AI Design: The new design generated by the AI module for this study.
-
The Manual Design: The new design created manually by the expert technician for this study.
The AI design file and the Manual Design file were each independently superimposed onto the Reference Design file. To ensure a precise and objective alignment, the superimposition was based on the identical, unchanged surfaces of the adjacent teeth present in all three scan files. This provided a stable and consistent reference area, isolating the restoration itself for comparison. Once aligned, the software performed a 3D surface comparison, calculating the point-to-point distances between the surface of the reference restoration and the surfaces of the AI and manual designs. The overall trueness was quantified by calculating root mean square error (RMSE). The software was also used to identify the single point of maximum discrepancy (positive or negative) for each comparison.
$$\mathrm{RMSE} = \sqrt{\frac{1}{n} \sum_{i=1}^{n} (X_{1,i} – X_{2,i})^2}$$
where X1 and X2 represent corresponding surface points in reference and test models, respectively, with n denoting total measurement points. The software was also used to identify the single point of maximum discrepancy for each comparison. Discrepancy maps were generated using a ± 500 μm color scale, with green zones (± 50 μm) indicating acceptable deviations.
Statistical analysis
Quantitative analyses were conducted using GraphPad Prism (v8.3.0, GraphPad Software). A paired analytical approach was employed, with all comparisons structured by the individual patient case. To guide the selection of the appropriate statistical test, the normality of data distribution was first evaluated using the Shapiro-Wilk test (α = 0.05). Based on these results, normally distributed data were analyzed using paired Student’s t-test, while datasets that did not follow a normal distribution were compared using the two-tailed Wilcoxon signed-rank test. All morphological trueness metrics are reported as median (interquartile range, IQR).