Carbapenemases are a group of β-lactamases that can degrade carbapenem antibiotics. The type of carbapenemase produced may vary across regions, time periods, populations, and bacterial species [5]. Our extensive screening of 14 CEGs revealed that 85.19% (46/54) of CREC carried CEGs, but only three genotypes, blaNDM−1, blaIMP, and blaKPC−2, were detected with the blaNDM−1 genotype being the most common, as high as 81.48% [(18 + 25 + 1)/54], and the detection rates of blaIMP and blaKPC−2 being lower, only 3.70% (2/54) and 1.85% (1/54). This is similar to the previous report in Guangdong Province (from November 2012 to August 2016) that blaNDM−1 (67.86%, 19/28) was the main genotype, supplemented by other carbapenems such as blaVIM−1 (3.57%, 1/28) [20]. Notably, the detection rate of blaNDM−1 has increased from 67.86 to 81.48%, suggesting a trend toward further spread of blaNDM−1 in Guangdong Province. However, this is not the same as in Jilin Province China where blaIMP−26, blaNDM−5, blaNDM−1 and blaKPC−2 gene could be detected from CREC before the COVID-19 epidemic (2016–2019), with the blaIMP−26 gene being the most common (50%; 6/12), followed by the blaNDM−5 gene (25%; 3/12) [21].In contrast, a study on the Enterobacter cloacae complex in Zhejiang Province, China, covering both the pre-epidemic and epidemic periods (2019–2020) identified six carbapenemase-encoding genes (CEGs): blaNDM−1, blaNDM−5, blaIMP−1, blaIMP−4, blaIMP−26, and blaKPC−2. Among these, blaNDM−5 was the most prevalent, detected in 42.86% (6/14) of isolates, followed by blaNDM−1, which was found in 28.57% (4/14) of cases. These findings differ from those reported in eight teaching hospitals in Guangdong Province, China [22], as well as from data collected in Vietnam prior to the COVID-19 pandemic (2014–2017). In the Vietnamese study, all CREC strains (100.00%; 18/18) carried the blaNDM−1 gene, and 72.22% (13/18) of these blaNDM−1-positive strains co-harbored the blaOXA−1 gene [23]. The above suggests that the prevalence of the various subtypes of CEG varies across regions and over time. The reasons for this may be related to regional differences in mobility, level of medical care, type of antibiotic used, frequency of antibiotic use and duration of use.
Among the 44 CREC strains carrying the blaNDM−1 gene, 59.09% [(25 + 1)/44)] had the blaNDM−1 gene localized exclusively on plasmids, while 40.91% (18/44) had it located on both plasmids and chromosomes. This differs from the findings of Weimei Ou et al. [8], who reported that 88.89% of blaNDM−1 genes were localized on plasmids, and 11.11% were located on chromosomes, with none found on both plasmids and chromosomes. These findings suggest that the blaNDM−1 gene is predominantly plasmid-borne. Interestingly, the detection rate of the blaNDM−1 gene on CREC chromosomes in Guangdong Province, China, is not negligible (33.33%, 18/54). Notably, in strains where the blaNDM−1 gene was found on the chromosome, the plasmid consistently carried the blaNDM−1 gene. There was no case where the gene was found exclusively on the chromosome, suggesting that the blaNDM−1 gene on the chromosome may have originated from the plasmid. This phenomenon could be explained by CREC acquiring compensatory mutations to overcome the fitness cost associated with plasmid-borne resistance genes. Such mutations may promote the integration of the blaNDM−1 gene from the plasmid into the chromosome under selective pressure from antibiotics [24]. Additionally, the ISCR1 element, which can mediate the integration of the blaNDM−1 gene from the plasmid to the chromosome, was found to be present in 82.60% (38/46) of the CEG-positive strains in our region [25]. This suggests that under certain conditions, ISCR1 can facilitate the transfer of the blaNDM−1 gene from the plasmid to the chromosome. The presence of the blaNDM−1 gene on both the chromosome and plasmid significantly enhances its transmission potential. Clinical workers should explore the synergistic roles of chromosomes and plasmids in the transmission of resistance to better control the spread of CREC. The blaIMP and blaKPC−2 genes were found exclusively on plasmids and not on chromosomes, which may be due to the limited sample size. However, the concurrent presence of blaIMP and blaKPC−2 genes on plasmids warrants attention. This study provides the first report on the current prevalence of CEGs on CREC plasmids and chromosomes in China over the past decade.
In the present study, the detection rate of CEGs was 85.19% (46/54), yet the resistance rate of CREC to all three carbapenem antibiotics exceeded 85.19%. This suggests that, in addition to CEG-mediated resistance, non-carbapenemase-producing mechanisms also contribute to CREC resistance [26]. These findings indicate that multiple resistance mechanisms likely work in tandem in CREC. The resistance rate of imipenem in the CEG-positive group was significantly higher than that in the CEG-negative group, indicating that CEGs play a crucial role in the development of CREC resistance to imipenem. The resistance rate of cefepime in the CEG-positive group was significantly higher than that in the CEG-negative group. This may be due to the fact that CEGs can confer resistance to almost all β-lactam antibiotics, potentially transforming them into “superbugs” [27]. Similarly, the resistance rate of cefotaxime/avibactam in the CEG-positive group was significantly higher than that in the CEG-negative group. This may be attributed to the fact that blaNDM-1 is very common in Guangdong Province, and avibactam cannot inhibit B-class metalloenzymes like blaNDM-1, which lack active site serine residues. As a result, avibactam cannot protect cefotaxime from being hydrolyzed by metalloenzymes [28].
Additionally, the resistance rates of gentamicin, ciprofloxacin and levofloxacin were significantly higher in the CEG-positive group compared to the CEG-negative group, likely due to the frequent presence of aminoglycoside antibiotic resistance genes and quinolone resistance genes in CEG-positive strains [23]. Another noteworthy observation is that the gentamicin resistance rate in this region (53.70%, 29/54) is more than twice that reported in Zhejiang Province, China, between 2004 and 2018 (26.55%) [29]. The analysis of the situation suggests the following possible reasons: the overall antibiotic resistance situation in China has worsened in recent years, especially during the COVID-19 pandemic, when patients frequently suffered from serious bacterial infections. Gentamicin was often used to alleviate the clinical symptoms of COVID-19 and reduce the rate of bacterial co-infection, leading to increased antibiotic selection pressure and promoting the emergence of gentamicin resistance [30, 31]. A concerning trend has emerged in the eight teaching hospitals in Guangdong Province, China: resistance rates of CEG-positive strains to tigecycline and polymyxin have significantly increased (both > 30%), contrasting with the 100% (18/18) sensitivity to these drugs observed in CEG-positive strains in Northeast China [32]. This increase in resistance may be attributed to the increased use of tigecycline and polymyxin in Guangdong in response to the COVID-19 pandemic. However, the specific reasons behind this phenomenon warrant further investigation. In conclusion, CEG-positive strains exhibit multiple resistance mechanisms, which may act independently or synergistically.
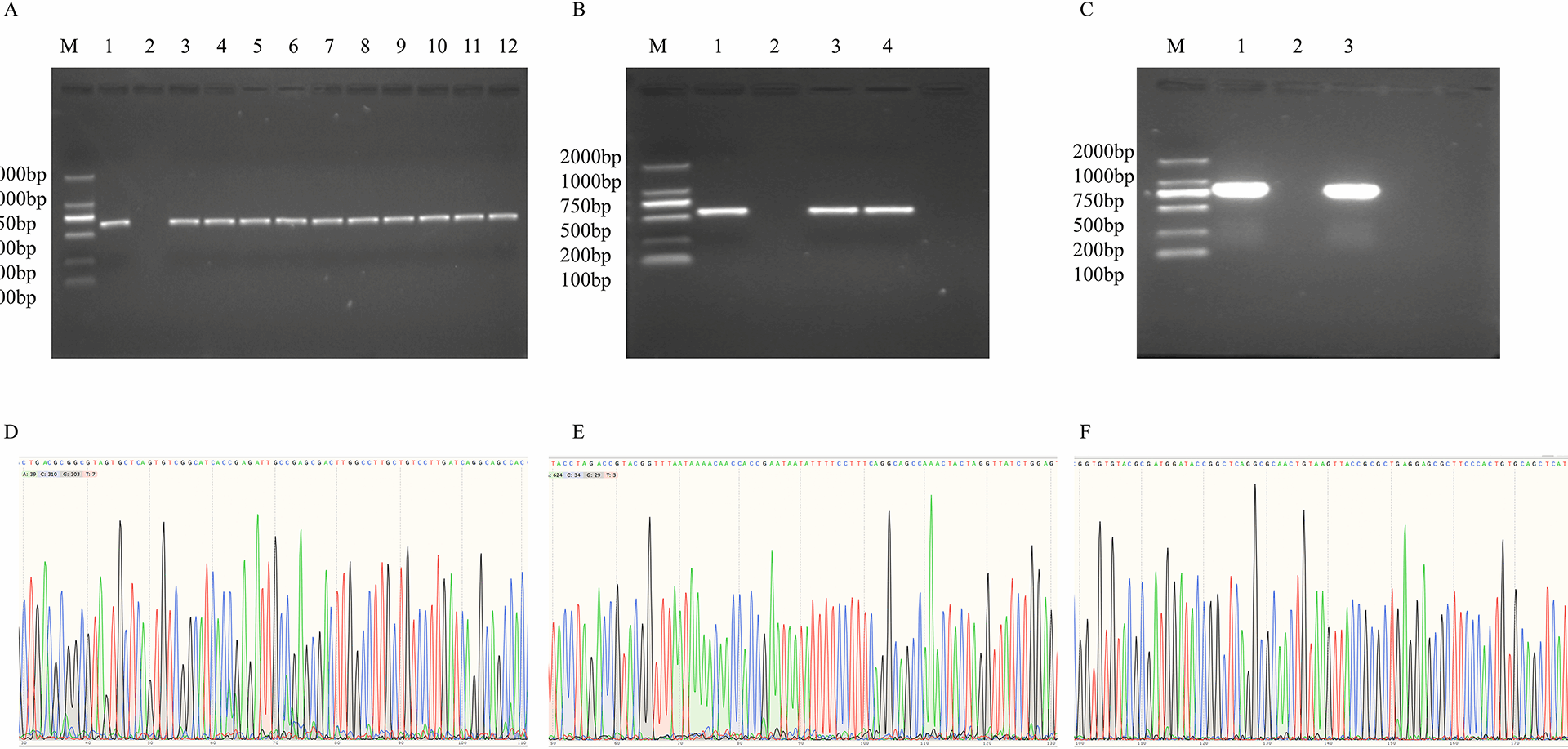
The two modes of transmission, horizontal and vertical, can act independently or synergistically, especially under the synergistic effect of these two mechanisms, which can accelerate the transmission speed of CEG [33]. CEG is spread horizontally between bacteria mainly through plasmids etc., which leads to rapid spread of bacterial resistance [4]. The blaKPC-2, blaNDM-1, and blaIMP genes can all be located on plasmids, indicating that the above-mentioned resistance genes may be transmitted horizontally through plasmid mediation. The conjugation experiment results confirmed that the blaNDM-1 and blaIMP genes are highly transmissible through conjugation, with a plasmid conjugation success rate of 95.65% (44/46). Specifically, the conjugation success rate was 100.00% (2/2) for the blaIMP gene and 95.45% (42/44) for the blaNDM-1 gene, significantly surpassing the 65.00% reported in southwestern China [34]. The analysis of the reasons is related to the fact that all detected CEG in this study can be localized on plasmids, and plasmid transmission of resistance genes is mainly achieved through conjugation mechanisms [35]. In CREC strains carrying both blaNDM-1 and blaKPC-2 genes, the blaNDM-1 gene was successfully conjugated, while the blaKPC-2 gene was not. This finding contrasts with the successful conjugation of the blaKPC-3 gene while the blaNDM-1 gene could not be conjugated in CREC strains carrying both blaKPC-3 and blaNDM-1 genes [36]. This difference may be attributed to the fact that the drug-resistant genes are located on different types of plasmids and associated with distinct mobile elements, which can influence the conjugation efficiency of these genes [36].
Mobile genetic elements, such as integrons, ISCR1, insertion sequences (ISEcp1, IS26), and the merA gene, are critical carriers of horizontal gene transfer, playing a significant role in facilitating the dissemination of resistance genes and accelerating their spread [37]. The positivity rate of IntI1 gene among CEG-positive strains is significantly higher than that among CEG-negative strains, and it was the only mobile genetic element that showed significant results, highlighting a strong association between IntI1gene and the transmission of CEG. This relationship may be attributed to the fact that IntI1gene, with a detection rate of 85.19% (46/54), is a genetic element capable of capturing and promoting the transfer of drug-resistance genes [38]. Its coexistence with other mobile genetic elements often enhances the ability of bacteria to spread resistance genes. For instance, the ISCR1 element, which shares structural similarities with IntI1gene, can form a complex with IntI1 gene, is facilitating the capture and dissemination of resistance genes [39]. In our region, 70.37% (38/54) of strains were positive for both ISCR1 and IntI1 gene, underscoring the need for clinical vigilance. Additionally, the IntI2 gene was detected in this region, contrasting with findings from Shanghai, China, where only the IntI1 gene has been reported [38]. Both IntI1 and IntI2 gene have been shown to enhance the transmission of antibiotic resistance genes in bacteria [40]. Clinicians should be aware of the development of this trend. Insertion sequence is a DNA fragment that can move within the genome and plays an important role in bacterial genome recombination, transfer, and drug resistance transmission, and the insertion sequences ISEcp1 and IS26 gene can mediate the fusion of two different plasmids through mechanisms such as homologous recombination, thereby achieving the spread of resistance genes between different bacterial strains [37]. In this region, the detection rates of ISEcp1 and IS26 gene in CREC were 87.04% (47/54) and 77.78% (42/54), respectively. Additionally, 68.52% (37/54) of CREC can carry both ISEcp1 and IS26 gene simultaneously, which undoubtedly enhances the transmission ability of resistance genes. This is different from Zambia where IS26 gene was not detected in enterobacter cloacae carrying ISEcp1 gene [41]. Current research on the role of ISEcp1 and IS26 gene in mediating drug resistance transmission in CREC remains limited, necessitating further investigation into the mechanisms by which these elements facilitate resistance gene transfer. The merA gene, closely associated with transposons, serves as a hallmark of the Tn21 gene transposon element. Notably, the Tn21 gene transposon, located upstream of the blaNDM-1 gene, enhances the effective dissemination of this resistance gene [42]. Another significant finding is the high detection rates of IntI1, ISCR1, ISEcp1, IS26, and merA gene, all exceeding 75%. Furthermore, 98.15% (53/54) of CREC isolates in this study carried two or more mobile genetic elements. This figure contrasts with the 83.33% (5/6) reported in Shandong Province, China, where CREC isolates carried at least two mobile genetic elements, such as ISAbal125, TN3-IS3000, and TN3 gene [43]. This disparity may stem from differences in the origins of the strains: the CREC strains in this study were isolated from clinical patients in hospitals, whereas the Shandong Province, China, study focused on isolates from healthy individuals. This finding indicates that there are significant differences in the types of mobile genetic elements carried in the bodies of healthy individuals and patients, which is of great significance for understanding the genetic diversity of CREC strains in different hosts.
The ERIC-PCR results revealed that the 54 CREC strains could be classified into 17 genotypes, with the two most prevalent genotypes being E and G, each accounting for 20.37% (11/54). Notably, all strains of genotype E were CEG-positive, while genotype G included CEG-positive strains, accounting for 18.52% (10/54). Given that the E and G genotypes were found in multiple hospitals and prefecture-level cities across Guangdong Province, China, this suggests the possibility of vertical transmission of CREC within the region, with the transmitted strains frequently carrying ECG. Additionally, two CEG-positive strains from the E genotype isolated from a single hospital exhibited a Dice coefficient of 100%, and a CEG-positive strain from the G genotype showed a Dice coefficient of over 70% with the two E-type strains, further indicating the occurrence of vertical transmission of CEG within the hospital. The possible reasons for this observation may include the fact that the CEG-positive strains mentioned above were all isolated from ICU patients with pulmonary infections (results not shown), who are often bedridden for extended periods and have limited direct contact with one another. Additionally, ICU patients frequently undergo various invasive procedures. Based on these factors, we speculate that the vertical transmission of CEG-positive strains may be linked to non-standard practices during medical procedures, such as inadequate hand hygiene by medical staff or incomplete cleaning and disinfection of medical equipment, which aligns with findings from other regions [44]. Therefore, clinical staff should emphasize hand hygiene and other preventive measures to avoid outbreaks similar to those reported in Zhejiang Province, China [45]. Furthermore, 50% strains (27/54) from genotypes E, F, G, and H across different hospitals had Dice coefficients greater than 70%, with CEG-positive strains accounting for 46.30% (25/54). This suggests a high degree of genetic homology among them. This may be due to Guangdong’s well-developed transportation network and the relaxation of COVID-19 control policies, which have led to increased population mobility and facilitated the spread of CREC.
The epidemiology of CREC and CEG exhibits regional variations [32,33,34]. However, the epidemiological characteristics of Guangdong Province, China, following the COVID-19 epidemic have not yet been reported. Therefore, it is important to clarify the specific epidemiological patterns in this region to better inform and guide anti-infection strategies. The detection rates of CREC and CEG, which are prevalent in eight teaching hospitals in Guangdong Province, China, are more than twice and three times higher in male patients [(72.22% (39/54), 64.81% (35/54)] than in female patients [(27.78% (15/54), 20.37% (11/54)], respectively. This is similar to the report from Nanjing, China [2]. It is noteworthy that current research predominantly focuses on the clinical and age-related distribution of CREC and CEG, with relatively limited attention given to the influence of gender differences on CREC infection. Therefore, future studies should aim to gather more comprehensive clinical data to investigate the role of gender in CREC infection. The prevalence of CREC and CEG in the eight teaching hospitals in Guangdong Province, China, is particularly high among elderly patients. This trend may be attributed to the fact that, within the context of the COVID-19 pandemic, elderly individuals, especially those with underlying health conditions, often experience more severe illness. Additionally, age-related organ function decline and compromised immune systems contribute to a heightened susceptibility to CREC infections. Notably, CREC and CEG have been detected across nearly all clinical departments, with respiratory medicine departments being the most frequently affected in the Guangdong hospitals. This is in contrast to the prevalence observed in burn surgery departments in southwestern China [34]. The above suggests that the prevalence of CREC and CEG may vary among different regions or medical institutions. CREC and CEG-positive strains from eight teaching hospitals in Guangdong Province, China, can infect almost any system of the body, with respiratory specimens being the most common [42.59% (23/54) and 33.33% (18/54)], followed by urine specimens and wound secretion specimens [22.22% (12/54) and 20.37% (11/54)], but the difference is that before the COVID-19, a cross regional study conducted in a tertiary hospital in northeast China from 2010 to 2019 found that CREC mainly causes urinary system and blood infections [32]. In summary, the detection rates of CREC and CEG in male, elderly, respiratory medicine and sputum specimens are the highest among the eight teaching hospitals in Guangdong Province China.
This study has some areas that could be improved. Firstly, the relatively small number of CREC strains included may not fully capture the diversity of the population, and there may also be statistical issues such as expanded confidence interval and excessive type II error risk, so future studies should aim to include a larger sample size. Secondly, the strains used in this study were sourced from only eight hospitals, which may not represent the prevalence of bacterial strains in other hospitals across Guangdong Province, China. Additionally, the localized nature of the sample collection may introduce some bias into the results. Expanding the scope of future research to encompass a wider range of hospitals and regions would provide more comprehensive and representative data on CREC.