Study design and setting.
A descriptive, facility-based study was conducted in 31 public health facilities located in humanitarian settings within the Amhara Region of Ethiopia. Ethiopia is the second most populous country in Africa, with a population of 126.5 million as of 2022 [21]. The government is divided into ten regional states, including the Amhara National Regional State, which is organized into 13 administrative zones. The study region is the second most populous region in Ethiopia, with an estimated population size of 22,876,991 [22].
The Ethiopian healthcare system is organized into three tiers: primary, secondary, and tertiary levels of care. The primary level encompasses primary healthcare units, including health posts, health centers, and primary hospitals. At the secondary level, services are delivered by general hospitals, whereas specialized hospitals provide tertiary care [23]. CAC services are available across all three levels of the healthcare system. Within the Amhara Region, there are 82 hospitals, 861 health centers, and 3,565 health posts serving both the host community and IDPs [24]. The number of Internally Displaced People (IDPs), refugees, returnees, and affected populations in the Amhara Region due to the northern Ethiopian conflict totals 542,300 people across 15 woredas (districts), corresponding to half of the total IDPs in Northern Ethiopia (1.1 million) [25].
The study was conducted in seven administrative zones of the Amhara Region: North Shewa, Oromia Special Zone, North Wollo, South Wollo, Waghimra, North Gondar, and South Gondar. Over the past five years, numerous humanitarian organizations, including the Ethiopian Midwives Association, have deployed more than 500 midwives to address the SRHR needs, including CAC, of displaced and host communities, with considerable financial and technical support from the United Nations Population Fund and the Ethiopian Ministry of Health (MOH) [26].
Study Population.
This study included women and adolescent girls who received CAC services at selected health facilities serving both host communities and IDPs over a seven-month data collection period, from September 21, 2023, to March 30, 2024. Eligible participants were those who sought CAC services for safely induced abortion, management of incomplete abortion, or post-abortion care during the study period. Women and girls who presented with complete abortions and did not receive any component of CAC services at the study facilities were excluded from the analysis.
Health Facility Selection.
A stratified sampling approach was initially employed to obtain a representative sample of public health facilities at different levels of care across the seven conflict-affected zones in northern Ethiopia. All three referral hospitals in the study area were purposively included. From the 46 primary and general hospitals in the selected administrative zones, 14 (30%) were randomly chosen, comprising seven general hospitals and seven primary hospitals. In addition, 14 of the 70 health centers (20%) were randomly selected. In total, this process yielded a sample of 31 public health facilities providing CAC services. In collaboration with the Ethiopian Ministry of Health (MOH) and the Amhara Regional Health Office, the selected facilities were subsequently assessed in terms of security conditions and client flow. Four facilities were found to be inaccessible due to active conflict and were replaced with more accessible alternatives (Ataye Hospital was replaced by Woldya Hospital, Ataye Health Center by Woldya Gonder Ber Health Center, Tefera Hailu Memorial Hospital by Dabat Hospital, and Seqota Health Center by Dabat Health Center). Over the seven-month data collection period, these facilities served an average of 60 women each for CAC services, amounting to approximately 1,860 clients.
Sample Selection.
The sample size for this study was determined based on the primary objective of a larger person-centered CAC project (Amare NS, Seyoum T, Tariku A, Mattison C, Klingberg Allvin M. Person-centered comprehensive abortion care provision and associated factors in northern Ethiopia: a cross-sectional study in a humanitarian setting, underview), yielding a final required sample size of 1,508 participants. All eligible participants (women and adolescent girls aged 13–49 years receiving CAC services) were consecutively enrolled over a seven-month data collection period. A total of 1,667 women and girls accessed health facilities during this period. However, 25 of them arrived with complete abortions and did not receive CAC services. Therefore, the actual study participants who received CAC at the 31 selected health facilities were 1,642, which comprises our final sample for analysis. 29.3% of our sample defined themselves as internally displaced women or girls (Amare NS, Seyoum T, Tariku A, Mattison C, Klingberg Allvin M. Person-centered comprehensive abortion care provision and associated factors in northern Ethiopia: a cross-sectional study in a humanitarian setting, underview).
Measurement.
Initially, a comprehensive costing assessment tool was developed based on previous studies done elsewhere [19, 27]. Data were collected using both closed-ended and open-ended questionnaires that covered several domains. The first domain included socio-demographic variables such as age, marital status, urban or rural residence, educational attainment, and occupation of the woman and her partner. Other domains included reproductive health-related characteristics such as the history of pregnancies and abortions, access to CAC services, women’s experiences and perceived quality of CAC, and assessments of immediate post-abortion contraceptive uptake. The rest of the survey was used to gather direct and opportunity costs incurred by the women from home to the facility level, including costs incurred by women who self-reported abortion attempts before reaching the health facility, costs of visits and stay at the health facility, costs after the procedure, and costs related to complications and readmissions.
More specifically, the tool was structured to gather the following inputs to calculate direct and opportunity costs: (i) before visiting a health facility: experiences with attempting unsafe pregnancy termination and consumption of substances, insertion of objects, and drugs, as well as inability of carrying out normal activities due to the pregnancy termination; (ii) at health facility: distance and time traveled and costs of transportation to one or multiple health facilities, days of stay at the health facility for women and caregivers, expenses on food, drugs, diagnostic tests or other fees, and inability to work during those days for both individuals; (iii) After the procedure: inability to work due to the recovery time for the woman, as well as for the caregiver taking care of her, and medical or other costs such as sanitary products; (iv) Revisits due to complications post abortion: whether the woman experienced complications and had to return to the health facility, transportation costs, duration of stay at the health facility, expenses on food, drugs, diagnostic tests or other fees, and inability to work during those days for her and her caregiver. For the opportunity cost of time, we use daily wages for low-skilled workers estimated by the International Labor Organization at ETB 2,382.4 (US$ 43.1) for men and ETB 1,584.6 (US$ 28.7) for women. All estimated costs in Ethiopian Birr (ETB) were converted to US dollars for reporting. The exchange rate of the Ethiopian Birr to the US dollar was based on the rate recorded at the beginning of the data collection period, from September 21, 2023, to March 30, 2024 (US$ 1 = ETB 55.28 ETB on September 21, 2023).Footnote 1 The survey tool is in the Supplementary Material.
Data collection.
The data collection tool was initially prepared in English and then translated into the local languages, followed by a back-translation into English to ensure consistency. The pilot test was conducted in a health facility in the North Wollo zone that was not included in the final list of study facilities. The choice of North Wollo was primarily due to security and logistical considerations, as it was one of the few accessible conflict-affected zones at the time of preparation. To avoid contamination, data from the pre-test facility were excluded from the sample for analysis. The data collection took place from September 21, 2023, to March 30, 2024, using Kobo Toolbox, an intuitive and powerful software for collecting, analyzing, monitoring, and managing survey data. Twenty midwife data collectors, all of whom held a bachelor’s degree, seven zonal supervisors, and one regional coordinator, received ten days of training on approaching women and conducting face-to-face interviews with participants. Consistency and quality of survey responses were maintained by assigning data collectors to study facilities that matched their local language fluency, such as Amharic or Afaan Oromo. Women aged 13–49 who received care for induced or incomplete abortions at study facilities were invited for interviews after providing written consent. Field assistants conducted interviews, with data quality monitored daily by central and regional teams. Continuous feedback ensured consistency and corrections during data collection.
Ethical Considerations.
The ethical approval was obtained from the Institutional Review Board (IRB) of the University of Gondar. The support letters were obtained from the Amhara Public Health Institute, Zonal, and Woreda health offices. The study was conducted under the principles of the Declaration of Helsinki and the International Ethical Guidelines for Biomedical Research involving human subjects. The IRB granted us to take informed consent from participants aged 13–49 years. Written informed consent was obtained after presenting the study’s aims and objectives to all participants, including emancipated minors, in accordance with the national research ethics guideline. These emancipated minors, typically under the age of 18 but working, earning their own living, married, or parenting, were eligible to provide consent, as approved by the IRB [28]. Special ethical consideration was given to emancipated minors, with additional safeguards such as confidentiality, post-abortion contraceptive counseling, and private settings during interviews, ensuring their protection throughout the study.
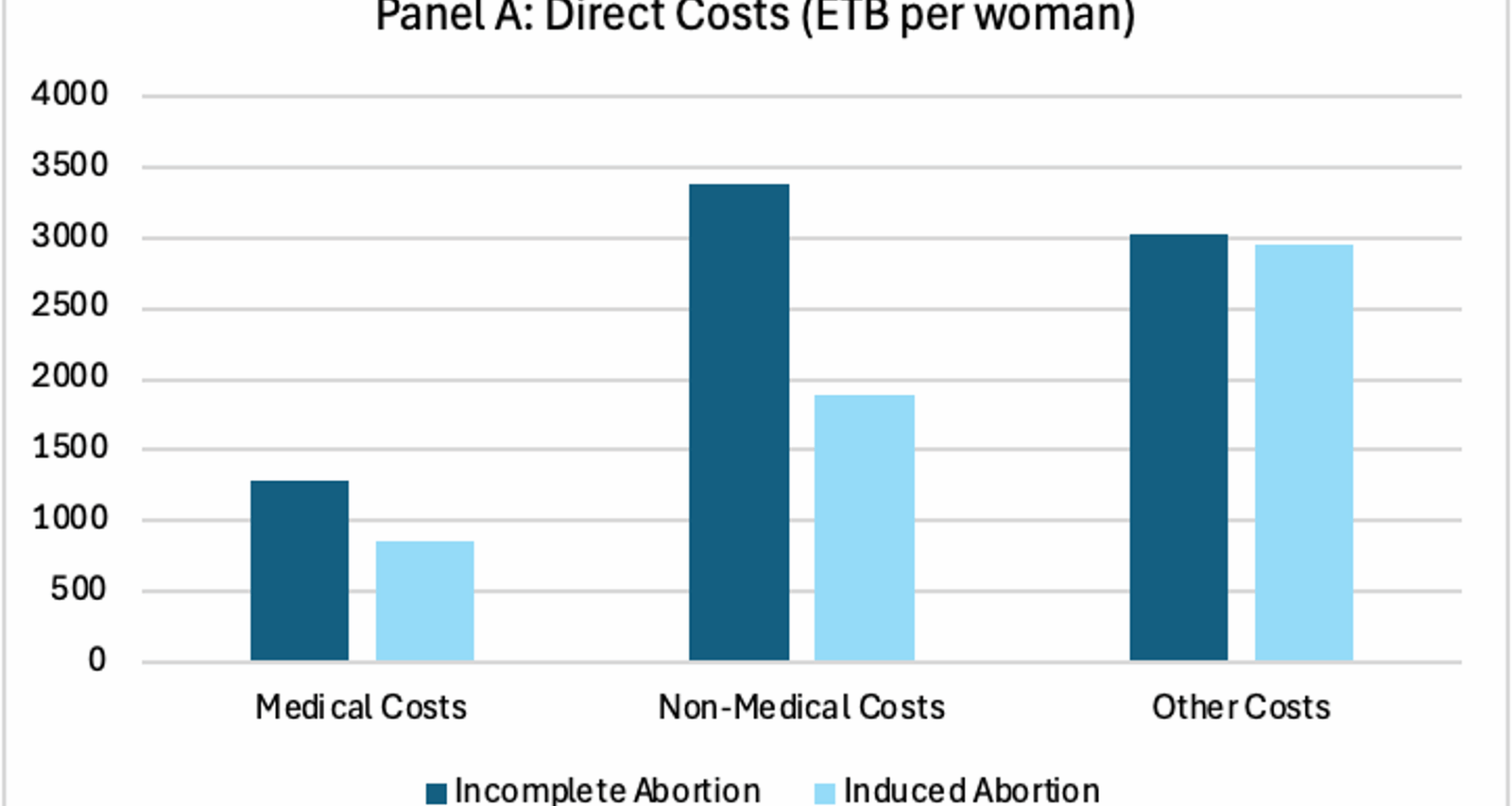
Data analysis.
The data were analyzed using Stata 18. The analysis aimed to: [1] provide descriptive statistics for the demographic characteristics of the women, and [2] examine the direct costs and opportunity costs involved in CAC. We also explore the costs by type of abortion (incomplete abortion or induced abortion), and by type of health facility (health centers, primary, general, and referral hospitals). Means and standard deviations (SD) were calculated to estimate each item in direct and opportunity costs. Both conditional means – the average of those who paid anything for the specific category – and unconditional means, the average of those who paid anything, including those who paid nothing for a particular category, were calculated. Descriptive statistics were computed as percentages for categorical variables.