Yang J, Endo Y, Munir MM, Woldesenbet S, Altaf A, Limkemann A, et al. Waitlist time, age, and social vulnerability: impact on the survival benefit of deceased donor kidney transplantation versus long-term dialysis among patients with end-stage renal disease. Transplantation. 2025;109(1):e64.
Malyala R, Tam-Vi Nguyen AL, Escamilla E, Ng A, Hammond L, Vozynuk S, et al. Establishing targets for goal-directed anesthesia in renal transplantation: a cohort analysis of high-saliency surgical time-courses. Am J Transpl. 2024;24(11):2055–65.
Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011;11(11):2279–96.
Perico N, Cattaneo D, Sayegh MH, Remuzzi G. Delayed graft function in kidney transplantation. Lancet. 2004;364(9447):1814–27.
Phillips BL, Ibrahim M, Greenhall GHB, Mumford L, Dorling A, Callaghan CJ. Effect of delayed graft function on longer-term outcomes after kidney transplantation from donation after circulatory death donors in the United Kingdom: a national cohort study. Am J Transplant. 2021;21(10):3346–55.
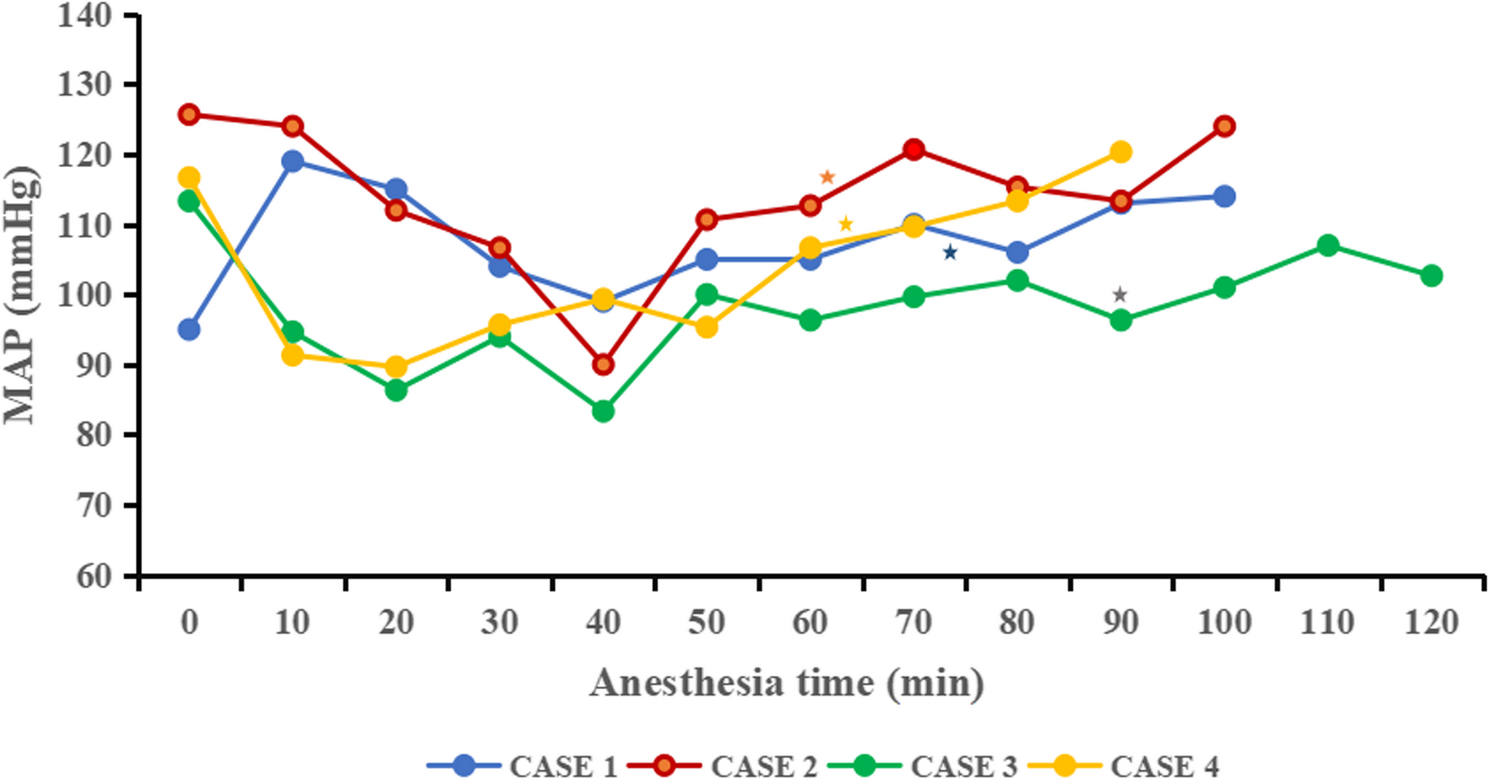
Kinoshita K, Yamanaga S, Kaba A, Tanaka K, Ogata M, Fujii M, et al. Optimizing intraoperative blood pressure to improve outcomes in living donor renal transplantation. Transplant Proc. 2020;52(6):1687–94.
Kawasaki S, Kiyohara C, Karashima Y, Yamaura K. Blood pressure management after reperfusion in living-donor kidney transplantation. Transplant Proc. 2020;52(10):3009–16.
Choi JM, Jo JY, Baik JW, Kim S, Kim CS, Jeong SM. Risk factors and outcomes associated with a higher use of inotropes in kidney transplant recipients. Medicine. 2017;96(1):e5820.
Sandid MS, Assi MA, Hall S. Intraoperative hypotension and prolonged operative time as risk factors for slow graft function in kidney transplant recipients. Clin Transpl. 2006;20(6):762–8.
Thomas R, Benken J, Belcher RM, Palmer ME, Benedetti E, Benken ST. Catecholamine vasopressor exposure is associated with early poor allograft function and adverse events in living donor kidney transplant recipients. Transplant Proc. 2023;55(7):1543–50.
Morelli A, Tritapepe L, Rocco M, Conti G, Orecchioni A, De Gaetano A, et al. Terlipressin versus norepinephrine to counteract anesthesia-induced hypotension in patients treated with renin-angiotensin system inhibitors: effects on systemic and regional hemodynamics. Anesthesiology. 2005;102(1):12–9.
Boccara G, Ouattara A, Godet G, Dufresne E, Bertrand M, Riou B, et al. Terlipressin versus norepinephrine to correct refractory arterial hypotension after general anesthesia in patients chronically treated with renin-angiotensin system inhibitors. Anesthesiology. 2003;98(6):1338–44.
Eyraud D, Brabant S, Nathalie D, Fléron MH, Gilles G, Bertrand M, et al. Treatment of intraoperative refractory hypotension with terlipressin in patients chronically treated with an antagonist of the renin-angiotensin system. Anesth Analg. 1999;88(5):980–4.
Nedel WL, Rech TH, Ribeiro RA, Pellegrini JAS, Moraes RB. Renal outcomes of vasopressin and its analogs in distributive shock: a systematic review and meta-analysis of randomized trials. Crit Care Med. 2019;47(1):e44-51.
Wong F, Pappas SC, Curry MP, Reddy KR, Rubin RA, Porayko MK, et al. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021;384(9):818–28.
Ginès P, Solà E, Angeli P, Wong F, Nadim MK, Kamath PS. Hepatorenal syndrome. Nat Rev Dis Primers. 2018;4(1):23.
Wong F, Pappas SC, Boyer TD, Sanyal AJ, Bajaj JS, Escalante S, et al. Terlipressin improves renal function and reverses hepatorenal syndrome in patients with systemic inflammatory response syndrome. Clin Gastroenterol Hepatol. 2017;15(2):266–e2721.
Wang J, Shi M, Huang L, Li Q, Meng S, Xu J, et al. Addition of terlipressin to norepinephrine in septic shock and effect of renal perfusion: a pilot study. Ren Fail. 2022;44(1):1207–15.
Mukhtar A, Salah M, Aboulfetouh F, Obayah G, Samy M, Hassanien A, et al. The use of terlipressin during living donor liver transplantation: effects on systemic and splanchnic hemodynamics and renal function. Crit Care Med. 2011;39(6):1329–34.
Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, et al. Perioperative quality initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019;122(5):563–74.
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121(4):706–21.
Morita K, Seki T, Nonomura K, Koyanagi T, Yoshioka M, Saito H. Changes in renal blood flow in response to sympathomimetics in the rat transplanted and denervated kidney. Int J Urol. 1999;6(1):24–32.
Kaufmann KB, Baar W, Silbach K, Knörlein J, Jänigen B, Kalbhenn J, et al. Modifiable risk factors for delayed graft function after deceased donor kidney transplantation. Prog Transplant. 2019;29(3):269–74.
Sicova M, McGinn R, Emerson S, Perez P, Gonzalez R, Li Y, et al. Association of intraoperative hypotension with delayed graft function following kidney transplant: a single centre retrospective cohort study. Clin Transpl. 2024;38(10):e70000.
Pongpruksa C, Khampitak N, Chang D, Bunnapradist S, Gritsch H, Xia VW. Intraoperative mean arterial pressure and postoperative delayed graft function in kidney transplantation: evaluating three commonly used thresholds. Clin Transpl. 2024;38(9):e15458.
Campos L, Parada B, Furriel F, Castelo D, Moreira P, Mota A. Do intraoperative hemodynamic factors of the recipient influence renal graft function? Transplant Proc. 2012;44(6):1800–3.
Aulakh NK, Garg K, Bose A, Aulakh BS, Chahal HS, Aulakh GS. Influence of hemodynamics and intra-operative hydration on biochemical outcome of renal transplant recipients. J Anaesthesiol Clin Pharmacol. 2015;31(2):174–9.
Wagener G, Bezinover D, Wang C, Kroepfl E, Diaz G, Giordano C, et al. Fluid management during kidney transplantation: a consensus statement of the committee on transplant anesthesia of the American society of anesthesiologists. Transplantation. 2021;105(8):1677–84.
Denton MD, Chertow GM, Brady HR. Renal-dose dopamine for the treatment of acute renal failure: scientific rationale, experimental studies and clinical trials. Kidney Int. 1996;50(1):4–14.
Friedrich JO, Adhikari N, Herridge MS, Beyene J. Meta-analysis: low-dose dopamine increases urine output but does not prevent renal dysfunction or death. Ann Intern Med. 2005;142(7):510–24.
Dönmez A, Karaaslan D, Sekerci S, Akpek E, Karakayali H, Arslan G. The effects of diltiazem and dopamine on early graft function in renal transplant recipients. Transplant Proc. 1999;31(8):3305–6.
Kadieva VS, Friedman L, Margolius LP, Jackson SA, Morrell DF. The effect of dopamine on graft function in patients undergoing renal transplantation. Anesth Analg. 1993;76(2):362–5.
Zhang X, Hu Y, Luo T. Low-dose dopamine for renal transplantation: a brief PRISMA-compliant meta-analysis. J Clin Anesth. 2020;67:110031.
Huh J, Kwon H, Park H, Park SC, Yun SS, Chae MS. Impact of norepinephrine and dopamine infusion on renal arterial resistive index during pre-emptive living donor kidney transplantation: propensity score matching analysis. Medicina (Kaunas). 2024;60(7):1066.
Schnuelle P, Benck U, Yard BA. Dopamine in transplantation: written off or comeback with novel indication? Clin Transpl. 2018;32(7):e13292.
De Backer D, Aldecoa C, Njimi H, Vincent JL. Dopamine versus norepinephrine in the treatment of septic shock: a meta-analysis*. Crit Care Med. 2012;40(3):725–30.
Saugel B, Sander M, Katzer C, Hahn C, Koch C, Leicht D, et al. Association of intraoperative hypotension and cumulative norepinephrine dose with postoperative acute kidney injury in patients having noncardiac surgery: a retrospective cohort analysis. Br J Anaesth. 2025;134(1):54–62.
Lankadeva YR, Kosaka J, Evans RG, Bailey SR, Bellomo R, May CN. Intrarenal and urinary oxygenation during norepinephrine resuscitation in ovine septic acute kidney injury. Kidney Int. 2016;90(1):100–8.
Benken J, Lichvar A, Benedetti E, Behnam J, Kaur A, Rahman S et al. Perioperative vasopressors are associated with delayed graft function in kidney transplant recipients in a primarily black and Hispanic cohort. Prog Transpl. 2022:15269248221087433. https://doi.org/10.1177/15269248221087433.
Levy B, Vallée C, Lauzier F, Plante GE, Mansart A, Mallie JP, et al. Comparative effects of vasopressin, norepinephrine, and L-canavanine, a selective inhibitor of inducible nitric oxide synthase, in endotoxic shock. Am J Physiol Heart Circ Physiol. 2004;287(1):H209–215.
Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA. 2016;316(5):509–18.
Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, Rhodes A, Landoni G, Osawa EA, et al. Vasopressin versus norepinephrine in patients with vasoplegic shock after cardiac surgery: the VANCS randomized controlled trial. Anesthesiology. 2017;126(1):85–93.
Jan MY, Moe SM, Adebiyi O, Chen J, Powelson J, Burney HN, et al. Vasopressin for post-kidney transplant hypotension. Kidney Int Rep. 2022;7(6):1364–76.
Glavaš M, Gitlin-Domagalska A, Dębowski D, Ptaszyńska N, Łęgowska A, Rolka K. Vasopressin and its analogues: from natural hormones to multitasking peptides. Int J Mol Sci. 2022;23(6):3068.
Leithead JA, Hayes PC, Ferguson JW. Review article: advances in the management of patients with cirrhosis and portal hypertension-related renal dysfunction. Aliment Pharmacol Ther. 2014;39(7):699–711.
Fayed N, Refaat EK, Yassein TE, Alwaraqy M. Effect of perioperative terlipressin infusion on systemic, hepatic, and renal hemodynamics during living donor liver transplantation. J Crit Care. 2013;28(5):775–82.
Zheng D, Liu G, Chen L, Xie W, Sun J, Wang S, et al. Effects of terlipressin on management of hypotensive brain-dead patients who are potential organ donors: a retrospective study. Front Pharmacol. 2021;12:716759.
Kidney Disease. Improving global outcomes (KDIGO) blood pressure work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99(3S):S1-87.
Legrand M, Falcone J, Cholley B, Charbonneau H, Delaporte A, Lemoine A, et al. Continuation vs discontinuation of renin-angiotensin system inhibitors before major noncardiac surgery: the Stop-or-Not randomized clinical trial. JAMA. 2024;332(12):970–8.
Legrand M. Should renin-angiotensin system inhibitors be held prior to major surgery? Br J Anaesth. 2024;132(5):831–4.
Shang Y, Wang C, Lu H, Chai L, Xu W, Bernardi M, et al. Incidence and type of adverse events in patients with cirrhosis receiving terlipressin: a systematic review and meta-analysis. Hepatol Commun. 2024;8(10):e0526.