WASHINGTON — Keith Joung knows better than a lot of people what, exactly, it might require to prove to regulators and patients that CRISPR could be safely used to alter the genome of a human embryo. If, of course, society decided that was a good idea.
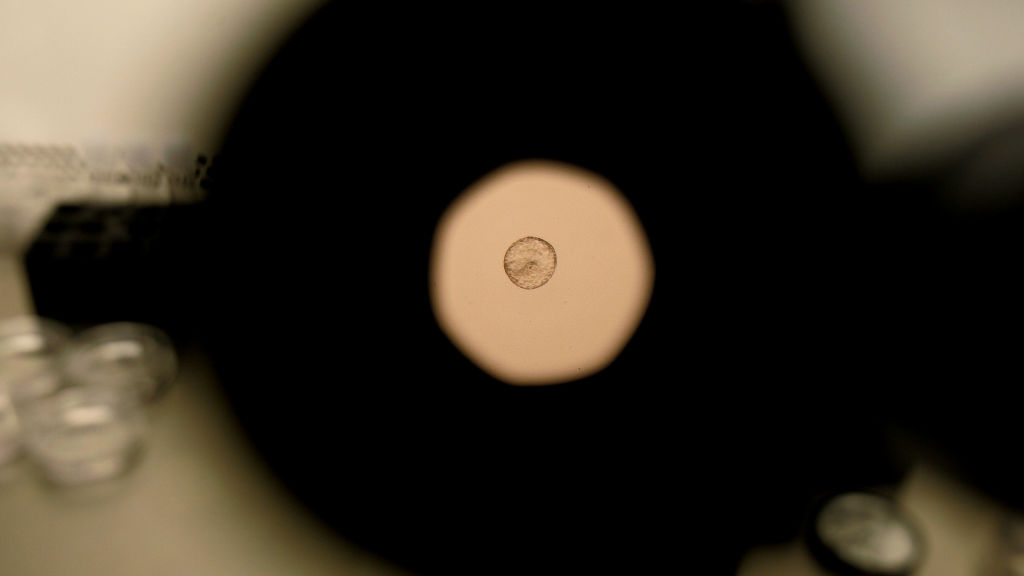
Joung, an early pioneer of the gene-editing technology, was the first to show CRISPR could target and cut DNA inside an embryo — in zebrafish — back in 2013. Not long after, his group was among the earliest to discover that CRISPR could get a bit sloppy — inadvertently slicing up unintended regions of the genome in all sorts of cells — complicating hopes it might be used to cure illnesses from cancer to muscular dystrophy.
A pathologist by training, Joung has spent much of the intervening decade designing ever-more sensitive methods for detecting these so-called off-target effects and finding ways to minimize the chances they occur. Such methods have, in the last two years, proved pivotal in the decisions by regulators to approve the first CRISPR-based medicine — an infusion of gene-edited blood stem cells called Casgevy — for treating sickle cell disease. Which is why, on Wednesday, at a gathering of a few dozen academics, physicians, industry experts, disease advocates, and religious leaders, many were surprised to hear Joung say that science was still a long, long way from having similar sorts of visibility into what happens inside a human embryo when it’s gene-edited.
“It’s very, very challenging, if not impossible,” Joung said to those gathered in Washington, D.C. for the meeting, which was organized by the American Society of Gene & Cell Therapy, the International Society of Cell & Gene Therapy and the Alliance for Regenerative Medicine.
Joung, currently on leave from Massachusetts General Hospital while he works at Arena Bioworks, offered one of many perspectives represented at the one-day event, dubbed “Advancing Guardrails on Heritable Human Editing.” The meeting was an attempt to pick up where the National Academies and the Royal Society left off two years ago in London, where the Third International Summit on Human Genome Editing closed with a call for more debate about whether the technique should ever be used, even as organizers encouraged research in the area of heritable editing to push forward.
Unlike so-called somatic gene editing, where one type of cell or tissue (the one where a mutation is wreaking the most havoc and causing disease) is targeted for modification, editing an embryo would mean all the cells of the resulting person would carry the genetic change. Different cells express different sets of genes, so if CRISPR screwed up, it would be hard to predict what the impact of that error would be in the brain versus, say, the heart. That’s even assuming there isn’t mosaicism — where CRISPR stays active after an embryo starts dividing, causing different types of mutations in the cells that give rise to different types of tissues.
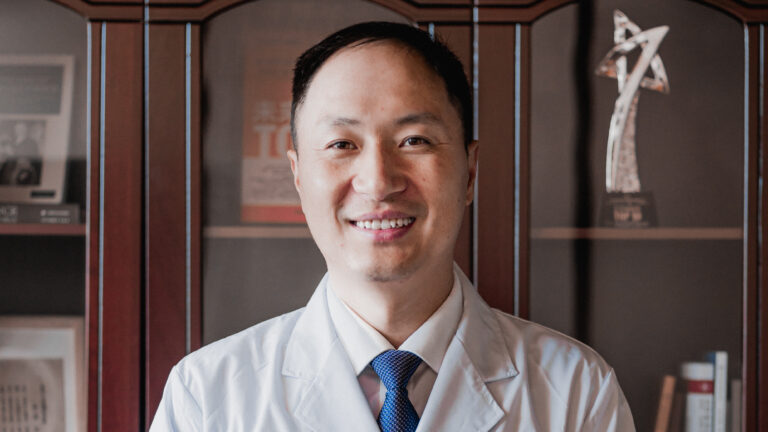
This is what happened to the twin girls born in 2018 as part of the now-globally renounced experiment undertaken by He Jiankui to make the first CRISPR children. In addition to all the ethical and legal issues with how the trial was conducted, sequencing showed the babies’ cells carried a mess of random edits, the health consequences of which are still unknown today. At the end of the 2nd International Summit on Human Genome Editing in Hong Kong, where He presented this data, organizers of the meeting condemned the experiment but said it showed “that it is time to define a rigorous, responsible translational pathway” toward trials that would test the impact of using CRISPR and other tools to edit the germline — the DNA of sperm, eggs, or embryos.

But scientists still lack the tools necessary for understanding what kinds of risks germline editing poses to future generations of humans, Joung said on Wednesday. “I don’t think we can define a regulatory pathway at this point because we don’t even have the assays or the experience to try to account for these safety-related issues,” he said. “At present, and for some fairly lengthy period of time going forward, we’re not going to have great insights into what the potential safety issues are for doing this type of editing.”
Notably, at this meeting, there were people in the room from the biotech industry, like Joung, who is also a co-founder of Editas Medicine and Beam Therapeutics, among other companies. That was important to Tim Hunt, head of the Alliance for Regenerative Medicine and one of the organizers. Back when he was himself working at Editas, Hunt rounded up executives from all the other major gene-editing companies working to bring the technology to patients — CRISPR Therapeutics, Intellia Therapeutics, Sangamo Therapeutics — and pitched a panel to the organizers of the 2018 Summit in Hong Kong. It was rejected. Twice. “Not enough time in the schedule,” Hunt said he was told.
That’s not uncommon for the National Academies, which tends to center science from academic institutions and is sensitive to potential conflicts of interest. But it still left a gap into which speculation about commercial interest in heritable human editing flowed. On Wednesday, those in attendance made it clear that altering the DNA of embryos is not a treatment modality the biotech industry is setting its sights on.
“It’s just completely infeasible from a financial perspective as opposed to a therapeutic that allows you to treat many, many patients,” said Devyn Smith, CEO of Arbor Biotechnologies, which is developing CRISPR treatments for rare diseases. But aside from the economics, Smith said it was hard to imagine diseases that could only be addressed through embryo editing. “I can’t think of a single indication that would be justified.”
This was frustrating to some of the rare disease advocates in the room. Sierra Phillips, whose son Jack was born with Warsaw Breakage Syndrome — an ultra-rare inherited developmental disorder — said if embryo editing to fix their mutations had been available during her experience with IVF, she would have opted for it, “1,000 percent.” “Don’t let fear of this being hard, or expensive, or a long timeline, get in the way,” she urged the industry representatives. “We don’t know if we don’t try.”
But Carrie Wolinetz, a former senior adviser to the director of the National Institutes of Health, who lost a child to a rare genetic disease 12 years ago, cautioned against moving to cross the embryo-editing Rubicon, maybe ever. “Nothing I’ve heard today has convinced me we can get to the safety standard that I would personally feel comfortable with,” she said.
For people like Wolinetz, who’ve been speaking and thinking about some of these issues for more than a decade, there was a certain sense of déjà vu in spending a day immersed in the latest state of the science and having that drive discussions about when or how embryo editing could move into human studies. “In all these years of conversations, we dance around the question of should we do this at all?” she said. “We call the question and then don’t really answer it.“
That’s something Benjamin Hurlbut, a biomedical historian at the University of Arizona, is hoping to change with an organization he co-founded called the Global Observatory for Genome Editing. In May, it will be convening a three-day event in Boston that’s open to the public and will take a human-first, rather than a technology-centric approach to trying to answer the question of “should we?”
Wednesday’s meeting, with its focus on envisioning guardrails for the technology and mechanisms for robust public dialogue regarding its potential future use, felt far removed from the political and economic realities of the present. Despite the National Institutes of Health’s main campus being located less than 10 miles away, the cascading cuts to jobs and grants and training programs that for the last two months have been roiling the NIH — the world’s largest public funder of biomedical research — earned barely more than a glancing mention.
The omission seemed to highlight the fact that the NIH and other federal agencies have long been prohibited from funding research involving the genetic manipulation of human embryos, through the Dickey-Wicker Amendment. The Food and Drug Administration is also not allowed to consider any clinical trials that would involve putting gene-edited embryos into a human with the intention of creating a baby.
Congressman Robert Aderholt, a Republican from Alabama, first introduced that ban in 2015. He joined the meeting briefly on Wednesday to voice his continued support for its renewal, adding that advancing safe and effective technologies while preserving the dignity of human life should never be a partisan issue.
Aderholt did not take any questions but described statements made by the National Academies, the Royal Society, and the World Health Organization as normalizing the pathways for heritable genome engineering. “Perhaps now is the time to renew a call for an international moratorium on human germline genome manipulation and to refocus our energy on ethical and effective gene and cell therapies that offer real solutions without crossing that dangerous ethical line,” he said.
Paula Cannon, a geneticist and virologist at the University of Southern California, and the president of ASGCT, didn’t go so far as to call for a moratorium. But she did appeal to those gathered to consider that they were lending legitimacy to a technology that isn’t ready for prime time. “The use cases are vanishingly small if not zero; we don’t have the safety, we don’t have the efficacy.” she said. “Therefore, what are we actually addressing? We’re addressing rogue actors — people who will use this not for unmet medical needs, but for enhancements… I think it’s OK to say there actually aren’t that many legitimate medical uses for this. There are only rogue uses. And so all the guardrails we’re talking about should reflect that.”