Northern Ireland residents are projected to live two years less than in the Republic, a new report has suggested.
The average life expectancy of 80.4 in Northern Ireland compares to 82.4 in the Republic for children aged under one in 2021, according to an island-wide economic comparison.
With the gap widening in recent years, the report from Ireland’s Economic & Social Research Institute stated: “Historically, there has been a perception that healthcare services in Northern Ireland are superior relative to those in Ireland. However, this is no longer the case.”
It suggests that regional disparities in the NHS and a series of austerity budgets in the UK have contrasted with increased health spending in the Republic.
A stark example was inpatient and outpatient waiting lists, where seven times as many people in Northern Ireland waited 18 months or more (86 per 1,000 people) compared to the Republic (12 per 1,000 people).
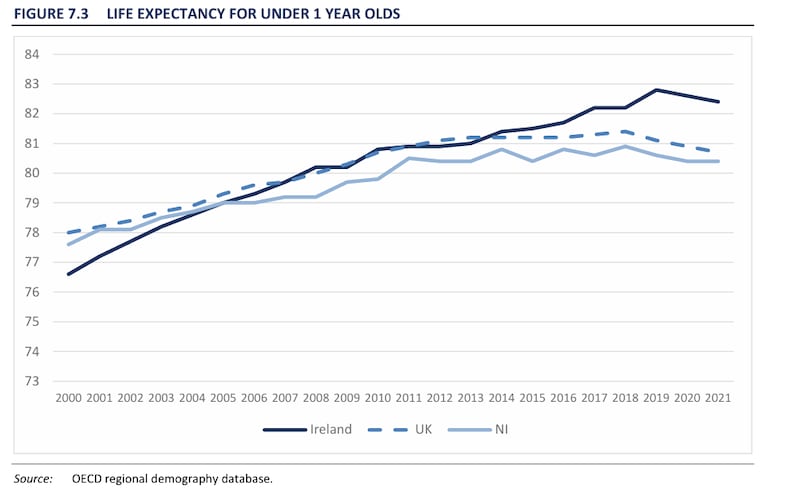 Life expectancy in Northern Ireland has dropped behind the Republic in recent years. PICTURE: ESRI
Life expectancy in Northern Ireland has dropped behind the Republic in recent years. PICTURE: ESRI
Another “extremely worrying development” was Northern Ireland’s rising infant mortality rates.
In 2012, the report said that infant mortality rates in the Republic and Northern Ireland were broadly equivalent (around 3.5 per 1,000 live births) and below the UK average (just over four per 1,000).
By 2021, Ireland and the UK’s figures had fallen to 2.8 and 3.6 respectively, but increased in Northern Ireland to a rate of 4.8, described as a “substantial infant mortality rate gap”.
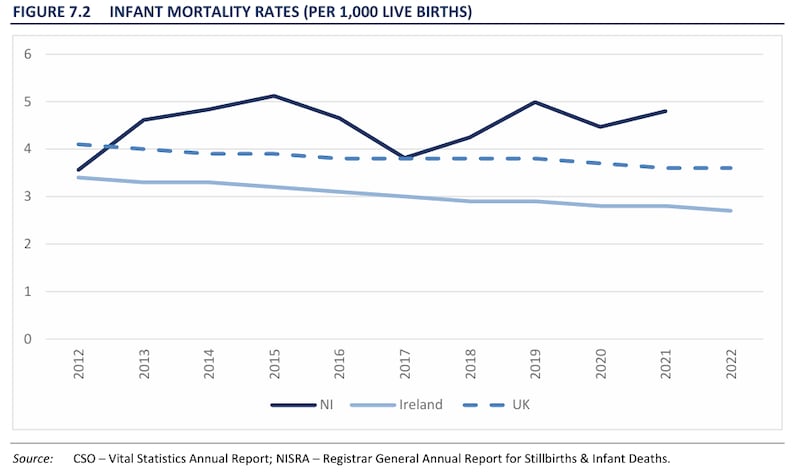 Infant mortality rates in Northern Ireland have increased as rates in the UK and Ireland have reduced. PICTURE: ESRI
Infant mortality rates in Northern Ireland have increased as rates in the UK and Ireland have reduced. PICTURE: ESRI
While Northern Ireland had enjoyed a “substantially higher” availability of hospital beds in 2009 (4.05 beds per 1,000 compared to 2.83) , this gap has gradually narrowed over time due to decreased provision in Northern Ireland, (close to three beds per 1,000 in both jurisdictions).
As another key indicator of wellbeing, education enrolment was also a fifth higher in the Republic, with 94% of 15-19 year-olds in education compared to 71% in Northern Ireland.
Adele Bergin, an author of the report and an Associate Research Professor at the ESRI, said: “Ireland has experienced stronger economic growth, higher wages, and higher living standards in recent years. The gap in economic performance and well-being indicators between Ireland and Northern Ireland is widening.”
In a written Assembly question, the SDLP’s MLA Daniel McCrossan called on Stormont health minister Mike Nesbitt to outline any action his department was taking to address the growing disparity.
“Given my focus on health inequalities, I welcome any evidence and information that helps support us in tackling this important issue,” he said.
Noting that there were different methodologies in compiling life expectancy figures on either side of the border, he admitted that improving healthy life expectancy and tackling health inequalities remained “a particular challenge.”
 Stormont Health Minister Mike Nesbitt has made tackling health inequalities in deprived areas one of his priorities. (Brian Lawless/PA)
Stormont Health Minister Mike Nesbitt has made tackling health inequalities in deprived areas one of his priorities. (Brian Lawless/PA)
He said the Executive’s Making Life Better strategy noted that health and wellbeing was shaped by “many factors” outside of his department’s control, such as age, family, community, workplace, beliefs and traditions, economics and physical and social environments.
“MLB is underpinned by a range of public health strategies and policies which focus on specific issues, such as substance use, suicide prevention, tobacco use and obesity prevention. These policies also have a focus on health inequalities and are implemented on the ground by the Public Health Agency.”
He added that a “targeted, place-based approach” called Live Better was designed to address health inequalities, by bringing targeted health support to communities which need it most – for which his department was “working collaboratively” with officials in the Republic.
The Health Minister is encouraging people to take care of their health and wellbeing, to help health and social care services 🏥
Minister Nesbitt was speaking at a charity walking football event in Lisburn ⚽
➡️Read more: https://t.co/pbtyBnAHaI pic.twitter.com/1xJXtHdY2f
— Department of Health (@healthdpt) May 19, 2025

