Cancer patients are experiencing life-threatening waits for scans and treatment due to a “chronic shortage” of radiologists and oncologists, doctors warn.
In some instances patients are waiting so long treatment is no longer possible, causing severe anxiety and leaving people in pain at the end of their life.
The shortage of doctors threatens to derail cancer care across the UK, new data from the Royal College of Radiologists (RCR) shows.
The shortfall has been put down to a combination of factors, including fewer students choosing to study therapeutic radiography, fewer available academic training programmes and wider challenges related to recruitment and retention of NHS staff.
RCR said pledges to reduce waiting lists and improve cancer survival rates cannot be delivered without more recruitment and better retention of specialist staff.
The Government’s 10 Year Health Plan is due to set out ways to meet the three cancer waiting time standards, which are that 75 per cent of patients urgently referred for suspected cancer receive a diagnosis of cancer or have cancer ruled out within 28 days of referral, 85 per cent of patients receive treatment within 62 days of an urgent referral for suspected cancer from a GP or a screening programme, and 96 per cent of patients receive treatment within 31 days of a decision to treat.
Currently, NHS England is failing to meet two of the 62-day referral to treatment standards and the 31-day decision to treat standard.
The RCR is calling on the Government to act urgently to invest in long-term solutions that will future-proof cancer services, by training more radiologists (who diagnose, treat and manage conditions and diseases, including cancer) and oncologists (who treat cancer).
Dr Katharine Halliday, a paediatric radiologist and president of the RCR, told The i Paper the situation is without question the worse she has ever seen.
She said members have reported cases where patients have waited so long for palliative radiotherapy to relieve their symptoms that it is no longer possible to provide the treatment.
“People are waiting in pain, and the thing about cancer treatment is that for every month that treatment is delayed, the mortality rate increases about 10 per cent,” she said.
One consultant radiologist said: “Patients are waiting longer than they should and we have had several delayed cancer diagnoses as a result.”
Safety concerns
A RCR report on oncologist staffing shows seven in 10 heads of service at cancer centres said they were concerned about the impact workforce shortages had on patient safety.
Twenty three per cent of heads of service reported they were not allowed to hire more staff due to a recruitment freeze. This is despite some regions having shortfalls of up to 49 per cent and being in need of hundreds of consultants.
The staffing shortages are making the safe delivery of cancer treatment is increasingly impossible, one oncologist said.
Dr Halliday said: “Staff under pressure don’t necessarily perform as well as they could if they had time.”
She added that while oncologists want to spend time listening to their patients and understanding what their needs really are, when under a lot of pressure they feel they have to move quickly.
“For instance, they might not have the report of the scan available in the clinic, so they whilst they can look at the scan and say, well, has the initial tumour has got smaller? It might be that there are other things on the scan that the radiologist would have picked up which they might not pick up,” she said.
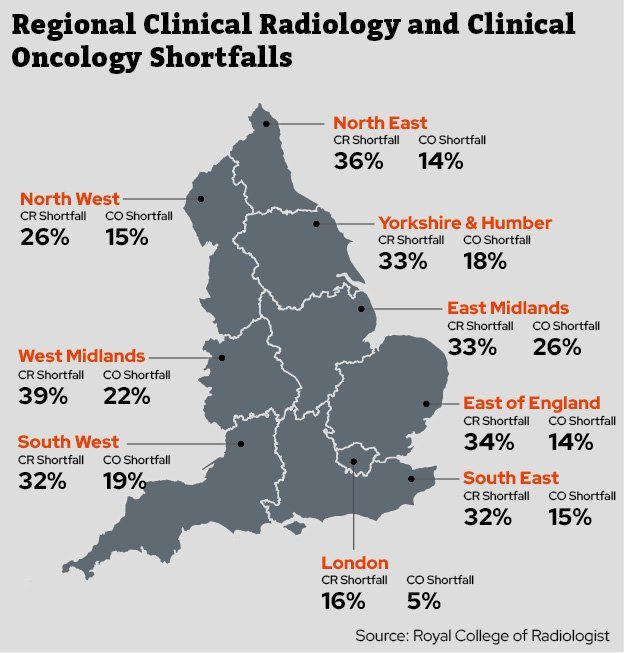 The west and east Midlands had some of the highest numbers of shortfalls
The west and east Midlands had some of the highest numbers of shortfalls
Demand for care continues to outpace the rate of workforce growth, the RCR said. Demand for CT and MRI imaging grew by 8 per cent, while the radiology workforce grew by just 4.7 per cent in 2024.
While staff enter the profession to do a good job, they cannot keep up, Dr Halliday said.
She urged the Government to act “straight away” to avoid the “ticking time bomb” for cancer patients.
The college said workforce pressures are also causing a retention crisis, with the average age of radiologists leaving the NHS workforce now 50 years old, down from 55 in 2020, and the average age a consultant clinical oncologist leaves is now 54, from 59 in 2022.
Postcode lottery
Data shows significant regional variation in relation to waiting times and staffing shortfalls, meaning patients face a postcode lottery for care.
North and West Wales and the north of Scotland have the highest clinical radiology shortfalls – 49 per cent and 47 per cent, respectively. By contrast South East Scotland has a 9 per cent shortfall.
The regions with the largest workforce shortfalls for clinical oncologists are North Wales (39 per cent) and South West Wales (28 per cent). By comparison London has a 5 per cent shortfall.
In five years, the shortfall of radiologists is set to rise from 29 per cent to 39 per cent, the RCR said. While there will be 19 per cent shortfall in oncologists.
In England, the East and West Midlands have the highest shortfall of clinical oncologists at 26 and 22 per cent respectively. Only London and the northwest are the only regions in England with a shortfall of clinical radiologists under 30 per cent.
 The Government has promised to build dozens of new hospitals (Photo: Jeff Moore/PA)
The Government has promised to build dozens of new hospitals (Photo: Jeff Moore/PA)
“Five years is important, because that’s how long it takes to train on radiologist,” Dr Halliday said. She added that while trainees can contribute to the workforce in the interim, in order have enough consultants to sustain the service, it is a five-year timeline.
A Department of Health and Social Care spokesperson said through its Plan for Change, the Government is determined to tackle delays, diagnose cancer earlier and treat it faster.
They added: “We are delivering 40,000 more appointments every week, investing £1.5bn in both new surgical hubs and AI scanners, rolling out cutting-edge radiotherapy machines to every region in the country, and backing our radiologists and oncologists with above inflation pay rises for the second year in a row.
“Later this year we will also publish a refreshed workforce plan to ensure the NHS has the right people in the right places to deliver the care patients need.”
‘Fragility in Service’
Bowel cancer is curable if diagnosed and treated early but patients with the disease face some of the longest waiting times.
Jennifer Bamforth, head of policy and influencing at Bowel Cancer UK, said the long waits leave patients feeling stuck in limbo, cause “a lot of anxiety” and can have a significant impact on their outcomes.
Bamforth said: “We know from data from Cancer Research UK and NHS England that the proportion of patients starting their treatment for lower GI (gastrointestinal) cancers who waited over 104 days from their urgent suspected cancer referral has continually increased over the last five years.
“We do know that around 13 per cent of colorectal clinical oncologists are locum consultants, which indicates a bit of fragility in that service.
“In terms of bowel cancer patients, the 62-day pathway hasn’t been met since its inception and part of that is due to the staff shortages.”
Only just over half (52 per cent) of people treated for bowel cancer received first definitive treatment within 62 days of an urgent referral, NHSE cancer waiting times data for March shows.
Bamforth said the Government’s national cancer plan has the potential – but will only be really impactful with investment in the workforce alongside it.
Have you been affected by long waits for cancer diagnosis or treatment? We would like to hear from you. Please email alannah.francis@theipaper.com
