The number of NHS-funded IVF cycles in certain areas of Greater Manchester could drop from three to one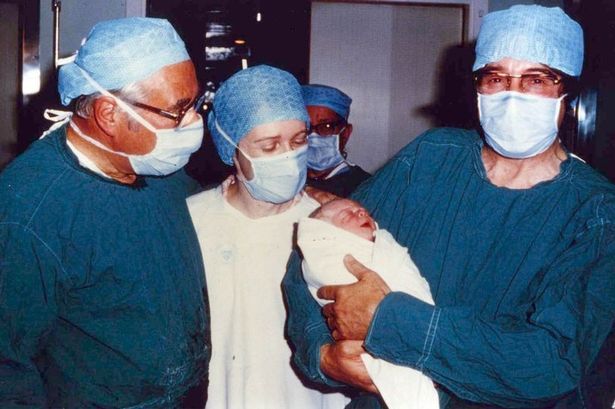 (Left to right) Gynaecologist Patrick Steptoe, embryologist Jean Purdy and physiologist Robert Edwards at the birth the first IVF baby, Louise Brown ,(Image: Copyright Unknown)
(Left to right) Gynaecologist Patrick Steptoe, embryologist Jean Purdy and physiologist Robert Edwards at the birth the first IVF baby, Louise Brown ,(Image: Copyright Unknown)
For many, including one mother-to-be, watching their chances of having a baby be slashed by a third would be ‘absolutely gutting’.
But this week, Greater Manchester health bosses have said they are trying to end a postcode lottery that can see people in one borough have triple the chance at IVF, while others only get one round of the treatment.
To end the disparity, the number of NHS-funded IVF cycles in certain areas of Greater Manchester could drop from three to one.
Greater Manchester’s NHS claims this is to create a ‘consistent approach’ that’s ‘fair for everyone’ across the city-region – saying it is fairer if all patients going through IVF get the same offer.
Yet some say that getting just one chance at having a child, through a process that is already a ‘minefield’, can make the pressure ‘absolutely horrendous’.
The Manchester Evening News spoke to a 36-year-old woman, due to give birth soon after going through one cycle of IVF in Manchester. From the very start of the journey, only being able to have one round for free on the NHS can have major consequences, she explains.
“You get one egg harvest session, we got six viable eggs from, and those six eggs were classed as the one cycle,” she told the M.E.N.
“In my head, that meant it felt like we got six chances. But if a couple only has just one egg, it’s the one chance they have.”
 The NHS offer is already an ‘absolute minefield’, said the expectant mother(Image: PA)
The NHS offer is already an ‘absolute minefield’, said the expectant mother(Image: PA)
This couple knows all-too-well the joys, setbacks, crushing blows and frustrations that can unfold in just one cycle. Finally, after three years of IVF treatment, their sixth egg out of six is hoped to arrive safely as a happy and healthy baby in just a few weeks.
But experiencing the feeling of running out of options piled on pressure to a process where stress can work against success.
“There’s massive pressure. Even when we were on egg four, we started thinking ‘we’ve only got two more eggs after this. I can’t lie, there are times that have been pretty horrendous, constantly thinking if you’re just wasting your time, wondering whether it’s going to work,” said the mum-to-be, who wishes to remain anonymous.
“You’ve just got to have blind faith that it will work. You’re being told that stress is the enemy in this process, but you can’t help but think about the situation which is inherently stressful.
“We had two miscarriages along the way – so we found that if you do get pregnant, that positive pregnancy test is just the start of the road.
“Then if you miscarry, you can’t have any treatment for the next egg until there’s been a six month break.
“In one breath, you’re being told to have a six month break, but after 35 your success with IVF can really decline, and at 40 it then becomes really difficult. I had moments where I was really frustrated that we were back waiting again, meanwhile I was just getting older.”
Three cycles of in-vitro fertilisation (IVF) are currently on offer for those who live in Tameside, while two cycles are available in Salford, Wigan, and Stockport. The other six boroughs of Greater Manchester – including Oldham, where the first IVF baby Louise Brown was born in 1978 – offer one cycle free to patients on the NHS.
The region’s NHS is encouraging people to take part in a six-week public consultation about the proposed changes – which include one full IVF cycle to eligible women aged 39 and under, along with an additional attempt known as a ‘1+’ round if the first cycle is cancelled or abandoned.
NHS Greater Manchester, which plans and pays for the region’s health services, says the ‘inconsistency stems from historic commissioning arrangements’.
The organisation added that it was reviewing the policies to ‘ensure a consistent and fair approach for everyone, regardless of where they live’, and that the change would be ‘affordable for the NHS now and in the future’.
 The site in Oldham where the original IVF cycle was carried out in 1978(Image: M.E.N.)
The site in Oldham where the original IVF cycle was carried out in 1978(Image: M.E.N.)
The Manchester IVF patient said: “I know the NHS doesn’t have endless purse strings, but speaking from personal experience, it would have made a massive difference [to have more than one cycle available].
“This last egg was our last roll of the dice, one more go. I had started pricing up private options because we had to approach it on the basis that it wasn’t going to work.
“On the surface of it, some private providers appear to offer you one round for around £3,500 – but it’s incredibly misleading because there’s hidden costs in lots of scans and tests to see which medications you need to be on.
“By the end of all that, it was looking more like £10,000 per round. For so many people, that’s just not an option.”
The NHS offer is already an ‘absolute minefield’, said the expectant mother. At the start of their IVF treatment the husband and wife lived in Manchester, but in the three-year-long process moved to Yorkshire.
It planted fears that they may have to start again because they fell under a different hospital trust, facing the prospect of ‘having to start at the back of the queue somewhere else’.
“You have to do an insane amount of paperwork. If one of you has a child from a previous relationship, you don’t qualify for free IVF – but that could be under any circumstances, you might be estranged from that side of your family, anything could have happened,” said the 36-year-old.
“There are lots of rules and hoops we had to jump through, it’s a really strict and slow process. We had six egg transfers and it’s taken us about three years.
“But we’re just so grateful that we got six eggs in the first place, because there are so many others who might only get one or even none at all.”
 NICE recommends people should be able to get three IVF cycles on the NHS(Image: Getty Images/iStockphoto)
NICE recommends people should be able to get three IVF cycles on the NHS(Image: Getty Images/iStockphoto)
The National Institute of Health and Care Excellence (NICE), which makes recommendations to the NHS about what care it should give to patients while ensuring the best value for money for the taxpayer.
NICE recommends people should be able to get three IVF cycles on the NHS, but the number of cycles that are actually on offer is at the discretion of local NHS organisations that run the services for their geographical areas.
Many NHS organisations around the country only offer one round..
“If you were in a trust that offered three rounds and were just starting off to be told you’d have those chances cut to one round, it would be absolutely gutting,” said the Manchester IVF patient.
“We knew from the start that we would just have the one round that was on offer. I’d definitely feel different if I had three rounds in front of me and then it was cut to one. Going from trebling your chances to just one round is hugely different.
“Hopefully all will be well with this baby. If we’d had more eggs, we’d have hoped to have a second child.
“Realistically speaking, we’ll have to call it a day now and stop at one.”
NHS Greater Manchester continued that one-cycle proposal comes because ‘this is the current policy in the majority of Greater Manchester, meaning no change for most residents; and it aligns with offers in most other parts of England’.
Katherine Sheerin, Chief Commissioning Officer at NHS Greater Manchester, said: “We know that fertility is a deeply personal and often emotional topic, which is why this consultation is so important. We want to ensure that everyone has the chance to contribute to the conversation about how these services are delivered fairly in Greater Manchester.
“Whether you’ve had experience with IVF, are considering fertility treatment, or simply want to share your perspective, please take part and share your views.”
The consultation runs from Wednesday, 18 June to Tuesday, 29 July 2025. You can take part by completing the online survey found on this website, attending one of NHS Greater Manchester’s local workshops or focus groups, or by contacting NHS GM to request information in a different format or language.
The consultation is not proposing changes to the eligibility criteria or the current offer of one cycle for women aged 40-42, which follows national guidance.
“So many people across Greater Manchester have been on deeply personal IVF journeys – or are just beginning one – and we completely understand there will be strong views about what’s being proposed,” added the organisation.
“That’s why we are running the public consultation on the proposed changes. We want to find out the public’s views on whether people agree with our current proposal of standardising to the offer across Greater Manchester to 1+ cycles, as well as asking who on their IVF journey any change would affect.”
A report summarising the feedback will be published to make the final decision, which will be made at a public NHS Greater Manchester board meeting later this year.
Email: gmhscp.engagement@nhs.net
Text/call/WhatsApp: 07786 673762
Freepost: NHS Greater Manchester Engagement Team, Chorley Road, Swinton, Salford, M27 5AS
