Genetic testing may be the only way to differentiate between common and more rare subtypes of renal cell carcinoma (RCC) to prevent misdiagnoses, according to the results of a study published in Human Pathology.
Mucinous tubular and spindle cell carcinoma (MTSCC) was found to share many morphological features with papillary renal cell carcinoma (PRCC) that could not easily be differentiated with a biopsy alone. The study authors recommended using chromosomal microarray or fluorescence in situ hybridization testing to confirm diagnoses.
“We want to stress that molecular testing is very useful to distinguish MTSCC from PRCC on a small specimen, and an accurate diagnosis means a better, more effective treatment plan for the patient,” urged senior study author Shuanzeng “Sam” Wei, MD, PhD, Associate Professor in the Department of Pathology and Medical Director of the Clinical Genomics Laboratory at Fox Chase Cancer Center.
Study Methods and Rationale
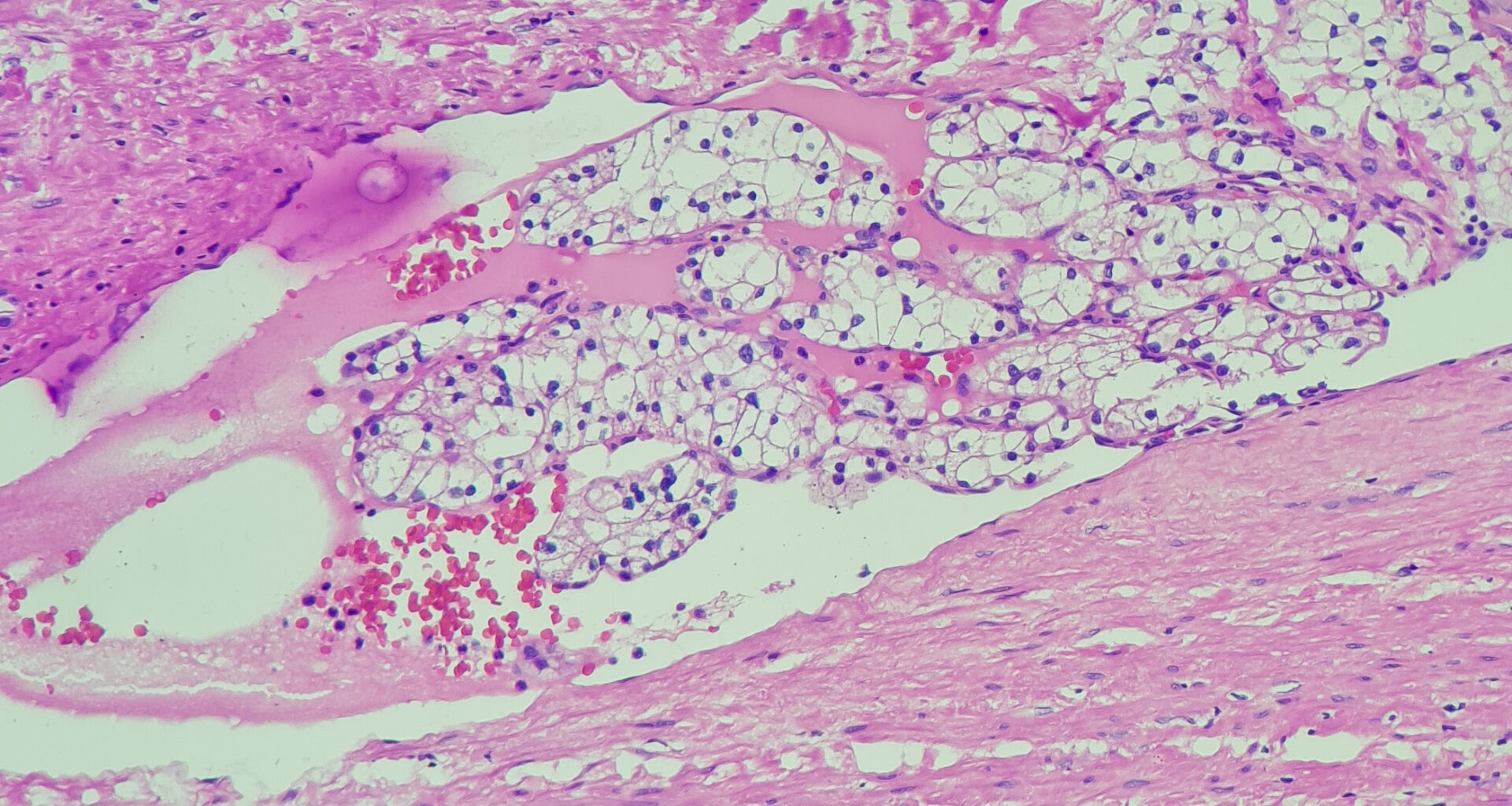
MTSCC is a rare subtype of RCC characterized by tubules, spindle cells, and extracellular mucinous stroma, but its rarity makes it a challenge to accurately diagnose, especially as the spindle cells can often incorrectly suggest sarcomatoid RCC. Additionally, papillary architecture in MTSCC was previously considered to be a rare finding.
The study authors compared five cases of MTSCC with papillary formation with 18 cases of former type 1 PRCC to determine if there was overlap or possible misdiagnosis between the cases. They conducted chromosomal microarray analysis to confirm each diagnosis and analyzed morphological features of each patient’s disease.
Key Study Findings
Investigators observed that focal papillary formation or more could be found in all five cases of MTSCC tumors, but the fibrovascular cores were predominantly mucinous with low cellularity and sparse vasculature. They also found psammoma bodies in two cases and foamy macrophages in four.
“Typically, papillary formation in mucinous tubular and spindle cell carcinoma is not a common finding. However, in this study we found papillary formation in all five cases of MTSCC,” Dr. Wei said.
On the other hand, classical papillary architecture was noted in all 18 cases of PRCC without bland spindled tumor cells. Focal mucinous stroma was found in 7 cases of PRCC (39%), foamy macrophages were seen in 15 (83%), and psammoma bodies in 5 (28%).
MTSCCs showed the typical monosomy of multiple chromosomes, but these tumors did not show the trisomy of 7, 17, and loss of Y usually found in PRCCs.
The overall shared features of papillary formation, foamy macrophages, psammoma bodies, and mucinous stroma make further genetic testing helpful for confirming these diagnoses.
Disclosure: For full disclosures of the study authors, visit sciencedirect.com.