Luan, S. & Wang, C. Calcium signaling mechanisms across kingdoms. Annu. Rev. Cell Dev. Biol. 37, 311–340 (2021).
Stock, C. et al. Fast-forward on P-type ATPases: recent advances on structure and function. Biochem. Soc. Trans. 51, 1347–1360 (2023).
Vulpe, C., Levinson, B., Whitney, S., Packman, S. & Gitschier, J. Isolation of a candidate gene for Menkes disease and evidence that it encodes a copper-transporting ATPase. Nat. Genet. 3, 7–13 (1993).
Jacobsen, N. J. et al. ATP2A2 mutations in Darier’s disease and their relationship to neuropsychiatric phenotypes. Hum. Mol. Genet. 8, 1631–1636 (1999).
Odermatt, A. et al. The mutation of Pro789 to Leu reduces the activity of the fast-twitch skeletal muscle sarco(endo)plasmic reticulum Ca2+ ATPase (SERCA1) and is associated with Brody disease. Hum. Genet. 106, 482–491 (2000).
Sudbrak, R. et al. Hailey-Hailey disease is caused by mutations in ATP2C1 encoding a novel Ca2+ pump. Hum. Mol. Genet. 9, 1131–1140 (2000).
De Fusco, M. et al. Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump α2 subunit associated with familial hemiplegic migraine type 2. Nat. Genet. 33, 192–196 (2003).
de Carvalho Aguiar, P. et al. Mutations in the Na+/K+-ATPase α3 gene ATP1A3 are associated with rapid-onset dystonia parkinsonism. Neuron 43, 169–175 (2004).
Brini, M. et al. Plasma-membrane calcium pumps and hereditary deafness. Biochem. Soc. Trans. 35, 913–918 (2007).
Schwinger, R. H., Bundgaard, H., Muller-Ehmsen, J. & Kjeldsen, K. The Na, K-ATPase in the failing human heart. Cardiovasc. Res. 57, 913–920 (2003).
Schubert, M. L. & Peura, D. A. Control of gastric acid secretion in health and disease. Gastroenterology 134, 1842–1860 (2008).
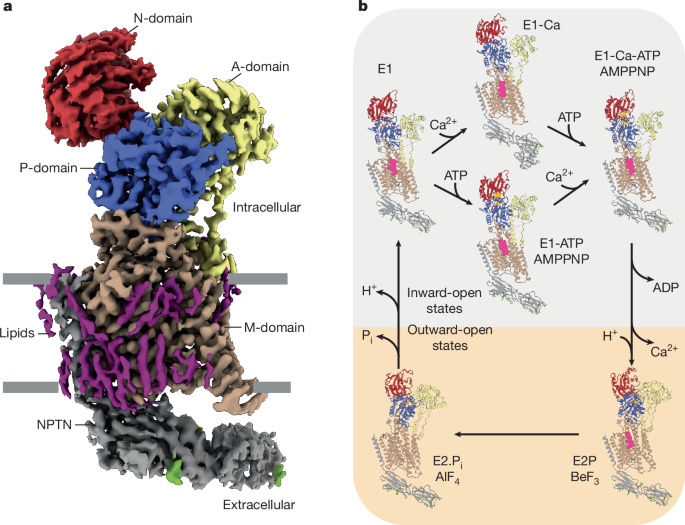
Dyla, M., Basse Hansen, S., Nissen, P. & Kjaergaard, M. Structural dynamics of P-type ATPase ion pumps. Biochem. Soc. Trans. 47, 1247–1257 (2019).
Albers, R. W. Biochemical aspects of active transport. Annu. Rev. Biochem. 36, 727–756 (1967).
Moller, J. V., Olesen, C., Winther, A. M. & Nissen, P. The sarcoplasmic Ca2+-ATPase: design of a perfect chemi-osmotic pump. Q. Rev. Biophys. 43, 501–566 (2010).
Wu, M. et al. Structure and transport mechanism of the human calcium pump SPCA1. Cell Res. 33, 533–545 (2023).
Gong, D. et al. Structure of the human plasma membrane Ca2+-ATPase 1 in complex with its obligatory subunit neuroplastin. Nat. Commun. 9, 3623 (2018).
Berridge, M. J., Lipp, P. & Bootman, M. D. The versatility and universality of calcium signalling. Nat. Rev. Mol. Cell Biol. 1, 11–21 (2000).
Constantin, C. E. et al. Ca2+-pumping by PMCA-Neuroplastin complexes operates in the kiloHertz-range. Nat. Commun. https://doi.org/10.1038/s41467-025-62735-5 (2025).
Schmidt, N. et al. Neuroplastin and basigin are essential auxiliary subunits of plasma membrane Ca2+-ATPases and key regulators of Ca2+ clearance. Neuron 96, 827–838.e9 (2017).
Niggli, V., Adunyah, E. S. & Carafoli, E. Acidic phospholipids, unsaturated fatty acids, and limited proteolysis mimic the effect of calmodulin on the purified erythrocyte Ca2+-ATPase. J. Biol. Chem. 256, 8588–8592 (1981).
Missiaen, L., Wuytack, F., Raeymaekers, L., De Smedt, H. & Casteels, R. Polyamines and neomycin inhibit the purified plasma-membrane Ca2+ pump by interacting with associated polyphosphoinositides. Biochem. J. 261, 1055–1058 (1989).
Peinelt, C. & Apell, H. J. Time-resolved charge movements in the sarcoplasmatic reticulum Ca-ATPase. Biophys. J. 86, 815–824 (2004).
Dode, L. et al. Dissection of the functional differences between human secretory pathway Ca2+/Mn2+-ATPase (SPCA) 1 and 2 isoenzymes by steady-state and transient kinetic analyses. J. Biol. Chem. 281, 3182–3189 (2006).
Liang, M. et al. Identification of a pool of non-pumping Na/K-ATPase. J. Biol. Chem. 282, 10585–10593 (2007).
Schultz, J. M. et al. Modification of human hearing loss by plasma-membrane calcium pump PMCA2. N. Engl. J. Med. 352, 1557–1564 (2005).
Ficarella, R. et al. A functional study of plasma-membrane calcium-pump isoform 2 mutants causing digenic deafness. Proc. Natl Acad. Sci. USA 104, 1516–1521 (2007).
Kabashima, Y., Ogawa, H., Nakajima, R. & Toyoshima, C. What ATP binding does to the Ca2+ pump and how nonproductive phosphoryl transfer is prevented in the absence of Ca2. Proc. Natl Acad. Sci. USA 117, 18448–18458 (2020).
Mintz, E., Mata, A. M., Forge, V., Passafiume, M. & Guillain, F. The modulation of Ca2+ binding to sarcoplasmic reticulum ATPase by ATP analogues is pH-dependent. J. Biol. Chem. 270, 27160–27164 (1995).
Winther, A. M. et al. The sarcolipin-bound calcium pump stabilizes calcium sites exposed to the cytoplasm. Nature 495, 265–269 (2013).
Beesley, P. W., Herrera-Molina, R., Smalla, K. H. & Seidenbecher, C. The neuroplastin adhesion molecules: key regulators of neuronal plasticity and synaptic function. J. Neurochem. 131, 268–283 (2014).
Rathod, N. et al. Nothing regular about the regulins: distinct functional properties of SERCA transmembrane peptide regulatory subunits. Int. J. Mol. Sci. 22, 8891 (2021).
Boudkkazi, S. et al. A noelin-organized extracellular network of proteins required for constitutive and context-dependent anchoring of AMPA-receptors. Neuron 111, 2544–2556.e9 (2023).
Chen, Z. et al. Cryo-EM structures of human SPCA1a reveal the mechanism of Ca2+/Mn2+ transport into the Golgi apparatus. Sci. Adv. 9, eadd9742 (2023).
Hansen, S. B. et al. The crystal structure of the Ca2+-ATPase 1 from Listeria monocytogenes reveals a pump primed for dephosphorylation. J. Mol. Biol. 433, 167015 (2021).
Zhang, Y. et al. Multiple sub-state structures of SERCA2b reveal conformational overlap at transition steps during the catalytic cycle. Cell Rep. 41, 111760 (2022).
Roderer, D., Schubert, E., Sitsel, O. & Raunser, S. Towards the application of Tc toxins as a universal protein translocation system. Nat. Commun. 10, 5263 (2019).
Toyoshima, C., Nakasako, M., Nomura, H. & Ogawa, H. Crystal structure of the calcium pump of sarcoplasmic reticulum at 2.6 Å resolution. Nature 405, 647–655 (2000).
Inesi, G., Kurzmack, M., Coan, C. & Lewis, D. E. Cooperative calcium binding and ATPase activation in sarcoplasmic reticulum vesicles. J. Biol. Chem. 255, 3025–3031 (1980).
Takahashi, K. & Kitamura, K. A point mutation in a plasma membrane Ca2+-ATPase gene causes deafness in Wriggle mouse Sagami. Biochem. Biophys. Res. Commun. 261, 773–778 (1999).
Toyoshima, C. et al. Crystal structures of the calcium pump and sarcolipin in the Mg2+-bound E1 state. Nature 495, 260–264 (2013).
Espinoza-Fonseca, L. M. The Ca2+-ATPase pump facilitates bidirectional proton transport across the sarco/endoplasmic reticulum. Mol. Biosyst. 13, 633–637 (2017).
Bublitz, M. et al. Ion pathways in the sarcoplasmic reticulum Ca2+-ATPase. J. Biol. Chem. 288, 10759–10765 (2013).
Ahmad, S. et al. Structural basis for effector transmembrane domain recognition by type VI secretion system chaperones. eLife 9, e62816 (2020).
Spiden, S. L. et al. The novel mouse mutation Oblivion inactivates the PMCA2 pump and causes progressive hearing loss. PLoS Genet. 4, e1000238 (2008).
Rahimi, M. J. et al. De novo variants in ATP2B1 lead to neurodevelopmental delay. Am. J. Hum. Genet. 109, 944–952 (2022).
Choquette, D. et al. Regulation of plasma membrane Ca2+ ATPases by lipids of the phosphatidylinositol cycle. Biochem. Biophys. Res. Commun. 125, 908–915 (1984).
Iwasaki, H. et al. A voltage-sensing phosphatase, Ci-VSP, which shares sequence identity with PTEN, dephosphorylates phosphatidylinositol 4,5-bisphosphate. Proc. Natl Acad. Sci. USA 105, 7970–7975 (2008).
Sehgal, P. et al. Inhibition of the sarco/endoplasmic reticulum (ER) Ca2+-ATPase by thapsigargin analogs induces cell death via ER Ca2+ depletion and the unfolded protein response. J. Biol. Chem. 292, 19656–19673 (2017).
Espinoza-Fonseca, L. M., Autry, J. M., Ramirez-Salinas, G. L. & Thomas, D. D. Atomic-level mechanisms for phospholamban regulation of the calcium pump. Biophys. J. 108, 1697–1708 (2015).
Driggers, C. M., Kuo, Y. Y., Zhu, P., ElSheikh, A. & Shyng, S. L. Structure of an open KATP channel reveals tandem PIP2 binding sites mediating the Kir6.2 and SUR1 regulatory interface. Nat. Commun. 15, 2502 (2024).
Gao, S., Yao, X. & Yan, N. Structure of human Cav2.2 channel blocked by the painkiller ziconotide. Nature 596, 143–147 (2021).
Hansen, S. B., Tao, X. & MacKinnon, R. Structural basis of PIP2 activation of the classical inward rectifier K+ channel Kir2.2. Nature 477, 495–498 (2011).
Lu, Y. et al. Structural insights into the conformational changes of BTR1/SLC4A11 in complex with PIP2. Nat. Commun. 14, 6157 (2023).
Sun, J. & MacKinnon, R. Structural basis of human KCNQ1 modulation and gating. Cell 180, 340–347.e9 (2020).
Yin, Y. et al. Activation mechanism of the mouse cold-sensing TRPM8 channel by cooling agonist and PIP2. Science 378, eadd1268 (2022).
Zhang, W. et al. Structural and functional insights into the lipid regulation of human anion exchanger 2. Nat. Commun. 15, 759 (2024).
Lindner, P., Christensen, S. B., Nissen, P., Moller, J. V. & Engedal, N. Cell death induced by the ER stressor thapsigargin involves death receptor 5, a non-autophagic function of MAP1LC3B, and distinct contributions from unfolded protein response components. Cell Commun. Signal. 18, 12 (2020).
Denmeade, S. R. et al. Prostate-specific antigen-activated thapsigargin prodrug as targeted therapy for prostate cancer. J. Natl Cancer Inst. 95, 990–1000 (2003).
Denmeade, S. R. et al. Engineering a prostate-specific membrane antigen-activated tumor endothelial cell prodrug for cancer therapy. Sci. Transl. Med. 4, 140ra186 (2012).
Quynh Doan, N. T. & Christensen, S. B. Thapsigargin, origin, chemistry, structure–activity relationships and prodrug development. Curr. Pharm. Des. 21, 5501–5517 (2015).
Murata, Y., Iwasaki, H., Sasaki, M., Inaba, K. & Okamura, Y. Phosphoinositide phosphatase activity coupled to an intrinsic voltage sensor. Nature 435, 1239–1243 (2005).
Tabata, S. et al. Electron microscopic detection of single membrane proteins by a specific chemical labeling. iScience 22, 256–268 (2019).
Lee, L. F. R. & Dall, P. M. Concurrent agreement between ActiGraph® and activPAL® in measuring moderate to vigorous intensity physical activity for adults. Med. Eng. Phys. 74, 82–88 (2019).
Drake, J. C., Allegra, C. J., Curt, G. A. & Chabner, B. A. Competitive protein-binding assay for trimetrexate. Cancer Treat. Rep. 69, 641–644 (1985).
Schulte, U. et al. Mitochondrial complexome reveals quality-control pathways of protein import. Nature 614, 153–159 (2023).
Kabsch, W. Xds. Acta Crystallogr. D Biol. Crystallogr. 66, 125–132 (2010).
McCoy, A. J. et al. Phaser crystallographic software. J. Appl. Crystallogr. 40, 658–674 (2007).
Adams, P. D. et al. PHENIX: a comprehensive Python-based system for macromolecular structure solution. Acta Crystallogr. D Biol. Crystallogr. 66, 213–221 (2010).
Emsley, P., Lohkamp, B., Scott, W. G. & Cowtan, K. Features and development of Coot. Acta Crystallogr. D Biol. Crystallogr. 66, 486–501 (2010).
Stabrin, M. et al. TranSPHIRE: automated and feedback-optimized on-the-fly processing for cryo-EM. Nat. Commun. 11, 5716 (2020).
Zheng, S. Q. et al. MotionCor2: anisotropic correction of beam-induced motion for improved cryo-electron microscopy. Nat. Methods 14, 331–332 (2017).
Rohou, A. & Grigorieff, N. CTFFIND4: fast and accurate defocus estimation from electron micrographs. J. Struct. Biol. 192, 216–221 (2015).
Wagner, T. et al. SPHIRE-crYOLO is a fast and accurate fully automated particle picker for cryo-EM. Commun. Biol. 2, 218 (2019).
Yang, Z., Fang, J., Chittuluru, J., Asturias, F. J. & Penczek, P. A. Iterative stable alignment and clustering of 2D transmission electron microscope images. Structure 20, 237–247 (2012).
Moriya, T. et al. High-resolution single particle analysis from electron cryo-microscopy images using SPHIRE. J. Vis. Exp. https://doi.org/10.3791/55448 (2017).
Punjani, A., Rubinstein, J. L., Fleet, D. J. & Brubaker, M. A. cryoSPARC: algorithms for rapid unsupervised cryo-EM structure determination. Nat. Methods 14, 290–296 (2017).
Zivanov, J. et al. New tools for automated high-resolution cryo-EM structure determination in RELION-3. eLife 7, e42166 (2018).
Pettersen, E. F. et al. UCSF Chimera — a visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Kaur, S. et al. Local computational methods to improve the interpretability and analysis of cryo-EM maps. Nat. Commun. 12, 1240 (2021).
Williams, C. J. et al. MolProbity: more and better reference data for improved all-atom structure validation. Protein Sci. 27, 293–315 (2018).
Meng, E. C. et al. UCSF ChimeraX: tools for structure building and analysis. Protein Sci. 32, e4792 (2023).
Krissinel, E. & Henrick, K. Inference of macromolecular assemblies from crystalline state. J. Mol. Biol. 372, 774–797 (2007).
Krissinel, E. Crystal contacts as nature’s docking solutions. J. Comput. Chem. 31, 133–143 (2010).
de Vries, S. J. et al. HADDOCK versus HADDOCK: new features and performance of HADDOCK2.0 on the CAPRI targets. Proteins 69, 726–733 (2007).
Dominguez, C., Boelens, R. & Bonvin, A. M. HADDOCK: a protein–protein docking approach based on biochemical or biophysical information. J. Am. Chem. Soc. 125, 1731–1737 (2003).
Laskowski, R. A. & Swindells, M. B. LigPlot+: multiple ligand–protein interaction diagrams for drug discovery. J. Chem. Inf. Model. 51, 2778–2786 (2011).
Sondergaard, C. R., Olsson, M. H., Rostkowski, M. & Jensen, J. H. Improved treatment of ligands and coupling effects in empirical calculation and rationalization of pKa values. J. Chem. Theory Comput. 7, 2284–2295 (2011).