KUALA LUMPUR, August 25 — MiCare Sdn Bhd has directed panel health care providers to limit Hong Leong bank employees to generic versions of medicines for chronic conditions.
The third-party administrator (TPA) owned by Zuellig Group, which is based in Hong Kong, said it received instructions to change drug prescriptions for staff of Hong Leong Bank Berhad and Hong Leong Islamic Bank Berhad.
“All panel clinics, hospitals and pharmacies are required to prescribe and dispense generic medications only. It is mandatory that all prescriptions must list only the active ingredient(s). This policy applies exclusively to long-term medication (LTM),” MiCare wrote in a letter dated last August 12 to panel general practitioner (GP) clinics, hospitals, and pharmacies, as sighted by CodeBlue.
This new policy comes into effect on September 1, 2025.
“We truly value the crucial role you play in the care journey of our members. Your understanding and collaboration in supporting this initiative will go a long way in balancing both quality care and long-term sustainability,” added MiCare.
The Federation of Private Medical Practitioners’ Associations Malaysia (FPMPAM) called for a revision of the policy, stressing that employers cannot interfere with the doctor-patient relationship even though they may determine the level of medical benefits provided.
“Clinical decisions must remain with the treating doctor, who ultimately carries the professional and medico-legal responsibility if anything goes wrong,” said FPMPAM president Dr Shanmuganathan Ganeson in a statement to CodeBlue.
“A rigid generics-only policy risks compromising patient outcomes while unfairly exposing doctors to medico-legal liability for decisions they did not freely make.
“FPMPAM is fully aware that this policy is driven by the intention of cost-saving, but doctors must retain the discretion to prescribe branded medicines when clinically indicated. We call on all relevant parties to revise this policy in order to safeguard patient safety, uphold clinical independence, and protect the integrity of medical practice.”
Dr Shanmuganathan explained that while generics are generally safe and effective, branded medicines are clinically necessary in certain circumstances, such as patients with allergies, differences in bioavailability, or the need for treatment stability.
“To illustrate, if generic SGLT2 inhibitors fail to achieve blood sugar targets compared with their originator counterparts, the doctor remains legally obliged to prescribe the originator to ensure safe and effective care.”
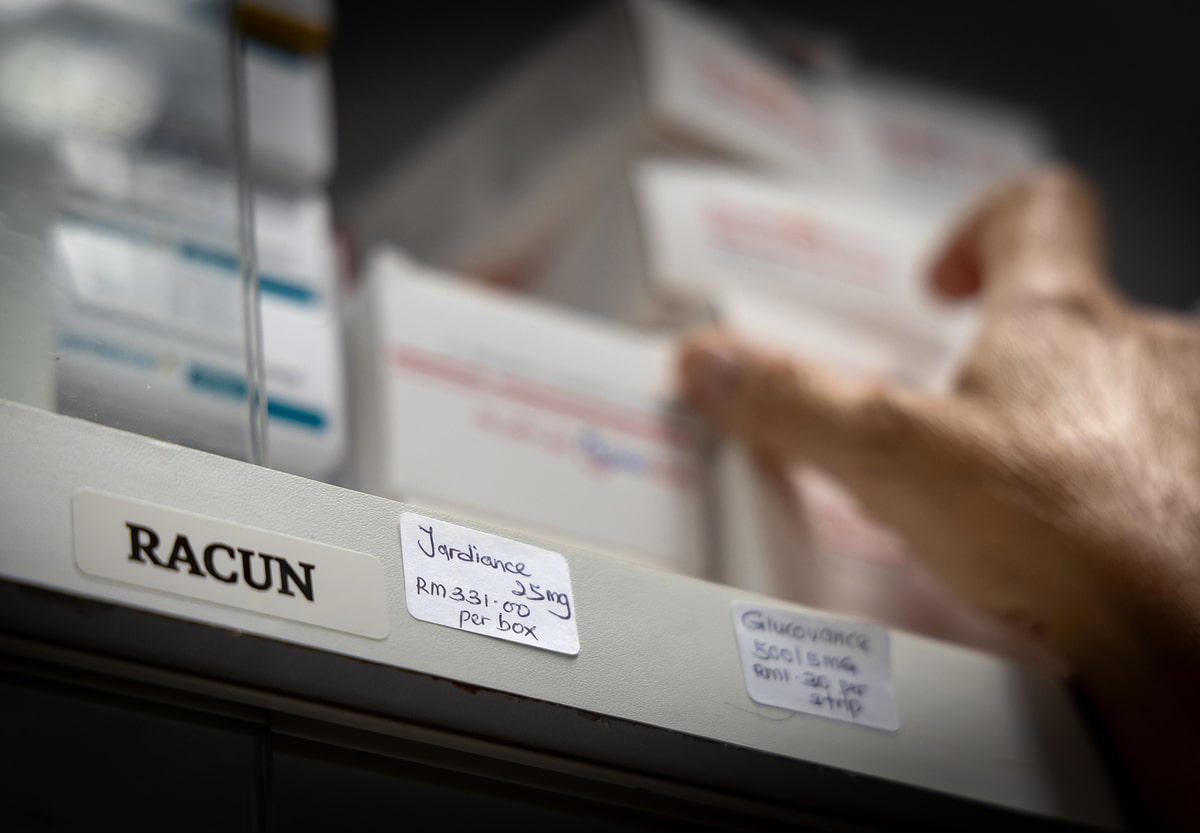
SGLT2 inhibitors, which treat diabetes, eventually reduce the need for insulin as it enables the kidneys to remove sugar from the body through urine. The drug is also used in people with chronic kidney disease (CKD) and heart failure to lower the risk of heart attack, stroke, and heart failure flare-ups; some of these inhibitors aid in slowing the progression of kidney disease.
“While generics are often safe and effective, their performance can vary across different formulations. There are clinical situations where treatment with a generic may not achieve the desired results — as seen in cases where certain generic antifungals failed to clear infections, while patients responded to the originator,” FPMPAM added.
“In such instances, insisting on generics alone is not cost-saving, as ineffective therapy prolongs illness and ultimately increases overall treatment costs.”
Without naming MiCare or Hong Leong, the Association of Private Hospitals Malaysia (APHM) confirmed that several member hospitals have received a policy update from a TPA on behalf of certain employers on a new generic-only policy.
“While APHM recognises the importance of cost-containment measures, we wish to emphasise that the responsibility for communicating such policy changes lies with the employer or insurer,” APHM president Dr Kuljit Singh told CodeBlue in a statement when contacted.
“We strongly urge employers to clearly inform their employees or policyholders that the directive to dispense only generic medications is issued by the employer. This clarity is essential to ensure seamless service delivery at the point of care and to avoid placing the burden on doctors or hospitals to explain or justify a policy that is out of their hands.
“It is also important to note that not all medications have generic alternatives, and such cases will need to be addressed individually.
“APHM member hospitals will gather operational feedback and document challenges arising from the implementation of this policy.”
The Malaysian Medical Association (MMA) similarly condemned the generic-only policy for long-term medications, without naming MiCare or Hong Leong, describing this as “unacceptable” interference by employers and TPAs in clinical decision-making.
“Medical treatment, including the choice of medicines, must always be determined by qualified medical professionals in consultation with their patients. When non-medical parties dictate treatment decisions, it not only undermines doctors’ professional autonomy but also compromises the standard of care patients are entitled to receive,” MMA president Dr Kalwinder Singh Khaira told CodeBlue in a statement.
“The MMA has long cautioned that unethical practices by some TPAs would eventually lead to situations such as this. Unfortunately, despite our repeated calls over the years, there has been little action taken to regulate these entities. We once again urge the government to act swiftly to regulate TPAs to prevent further intrusion into health care decisions.
“We wish to stress that safeguarding doctors’ autonomy is not only a matter of professional ethics, but also a critical component in ensuring patient safety and trust in the health care system. If left unchecked, such interference could lead to poorer treatment outcomes, patient dissatisfaction, and erosion of confidence in the medical profession.”
CodeBlue has requested comments from MiCare.
Doctors’ groups have long called for regulation of TPAs or managed care organisations (MCOs). In an open letter to Prime Minister Anwar Ibrahim in September 2023, thirteen associations representing medical practitioners claimed that cost-containment measures by these “middlemen” have resulted in rationed and restricted care.
They wrote that the business model of MCOs was likely to breach laws regulating the medical profession, such as the Medical Act 1971 and the Private Healthcare Facilities and Services Act 1998, thus undermining the quality of medical care for patients.
As medical inflation became a major issue over the past year, the government has targeted health care providers like GP clinics and private hospitals with policies like drug price display and a planned diagnosis-related groups (DRG) reimbursement model.
However, the government did not propose policy reforms for payers like TPAs or health insurance providers, aside from a 10 per cent cap of premium increases for at least 80 per cent of policyholders until the end of 2026.