It was the kind of message doctors go into medicine to receive: ‘Thank you,’ it read, ‘for saving my life.’
Its author was Kelly Owens, then 29. From the age of 13, Kelly had lived with the crippling symptoms of two autoimmune conditions: Crohn’s disease – an incurable condition that causes severe inflammation in the bowel, leading to pain, fatigue and diarrhoea – as well as inflammatory arthritis.
Kelly had been hospitalised more than once and spent years on potent steroids in an attempt to control the inflammation that drove her symptoms.
Eventually, after more than 15 years of taking these drugs, their side-effects caught up with her and, in her late-20s, she was diagnosed with osteoporosis (a common effect of the steroid prednisone, as it affects the body’s absorption of calcium and increases the rate that bone breaks down).
The medics who were treating her, though, were out of answers. Prednisone, they said, was all they could offer her.
Kelly had to give up her career as a teacher as her symptoms worsened, with her legs becoming so swollen she couldn’t walk far – her husband became accustomed to carrying her on his back if they ventured out and she took a turn.
The doctor who turned her life around – the recipient of that heartfelt email sent in 2017 – was neurosurgeon Dr Kevin Tracey, a world expert in the vagus nerve.
The vagus nerve is the longest nerve in our body. Running between the base of the brain down to the lower torso, it carries signals between the brain and every major organ, including the heart, lungs and the digestive system, helping to regulate important bodily processes including our heart and breathing rates.

Within weeks of having the device fitted beneath her collarbone as part of her treatment, Kelly Owens was walking without a cane for the first time since she was a teenager
The vagus nerve has become known as the ‘super highway’ of the nervous system
Thanks to its length and reach, the vagus nerve has become known as the ‘super highway’ of the nervous system.
But as Dr Tracey told Good Health, its workings are ‘much more mysterious and beautiful than traffic – they’re more like the strings, reeds, percussion and soundboards of an orchestra, the 200,000 or so nerve fibres of your vagus vibrate in tune with health’.
It was Dr Tracey who, in a landmark discovery in the early 1990s, showed that the immune system and brain are linked through our vagus nerve, and that by stimulating the nerve it is possible to treat inflammation.
He now believes that this technique could also replace weight-loss jabs such as Mounjaro – but more on that later.
In autoimmune illnesses, such as Crohn’s, the immune system can ‘overreact’ to threats, producing too much of a molecule called a cytokine. Put simply, while cytokines are a vital part of our immune response, an excess can tip the body into an inflammatory state and some make people ill.
Dr Tracey was researching this cytokine response in 1992, in his newly set up lab at the Feinstein Institutes in New York. He and his colleagues were studying an artificial anti-inflammatory molecule they’d developed, CNI-1493.
Clinical trials had shown that CNI-1493 injections had positive effects on patients with inflammatory bowel disease, reducing inflammation and tissue damage.
But Dr Tracey and his team then discovered – unexpectedly – in studies on rodents, that administering CNI-1493 in the brain also reduced inflammatory cytokines throughout the body. This was despite the fact that the dose administered in the brain was too low to enter the bloodstream.
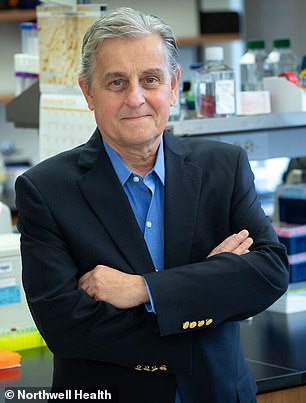
Dr Kevin Tracey is a vagus nerve expert
So how was this happening?
On a hunch, Dr Tracey repeated the process, but severed the vagus nerve of the mouse they were experimenting on. And this time, despite administering CNI-1493 into the brain, there was no reduction of inflammation in the body.
The conclusion was a radical one: the vagus nerve regulates the immune system ‘through an anti-inflammatory healing reflex’, as Dr Tracey writes in his book, The Great Nerve: The New Science Of The Vagus Nerve.
This in turn meant that ‘it should be possible to regulate inflammation with devices that stimulate the vagus nerve in patients’.
This was a groundbreaking thought at the time, for while nerve stimulation devices have been used since the 1980s to prevent seizures in people with severe epilepsy (by dampening down irregular electrical activity in the brain), this was the first time it had been suggested for inflammatory diseases.
Dr Tracey then set up a company, Setpoint Medical, to develop a device to stimulate the vagus nerve using electrical impulses to treat inflammation.
Kelly, who lives in New Jersey in the US, came across Dr Tracey’s work online and contacted him following a flare-up of her Crohn’s in 2015 that left her so malnourished and emaciated she had to be admitted to hospital for 12 days, receiving fluids, nutrients, steroids and morphine via a drip.
She’d seen a video of Dr Tracey discussing his research on the vagus nerve and how it could be used to treat people with autoimmune conditions – and, in 2017, she joined a clinical trial his research company was running.
A small device – about the size of a muffin – was implanted in the chest wall beneath her collarbone, with a lead threaded up her neck and attached to the vagus nerve: it was programmed to be activated two or three times a day for several minutes only to dial down the inflammation. (Essentially it inhibits inflammation in the spleen with the effect then spreading throughout the body, including the joints, Dr Tracey explains.)
Within weeks, Kelly was walking without a cane for the first time since she was a teenager. Eight weeks later, her gastrointestinal symptoms had vanished. A few months later, she was steroid-free.
‘Kelly still has the device and is doing extraordinarily well, both personally and professionally,’ Dr Tracey says, describing Kelly’s hobby of building custom guitars – an astonishing achievement for someone who previously suffered crippling pain in her hands, fingers, elbows, jaw, shoulders, back, hips, knees, toes and ankles.
And he is emphatic: ‘Kelly’s remarkable clinical improvements are due to vagus nerve stimulation (VNS) and underscore the promise of bioelectronic medicine.’
It’s a promise that’s been recently recognised by the US medical regulator, the FDA, which approved the Setpoint implant for people whose rheumatoid arthritis is not being controlled well enough by medication.
This followed a landmark trial that showed significantly more patients given the implant experienced improved symptoms compared with a control group.
In fact, it could be said that the vagus nerve is having something of a ‘moment’, as millions of social media hashtags proclaiming its importance testify.
Meditation, Wim Hof-style ice baths and deep breathing to achieve a sense of calm are all based on vagus nerve stimulation.
However, less well known, perhaps, is research such as Dr Tracey’s which has identified a link between vagus nerve stimulation and easing digestive conditions such as Crohn’s and IBS.
And he now believes VNS, rather than GLP-1 injections, is the future for weight loss.
As he told Good Health: ‘GLP-1 injectable drugs such as Mounjaro and Ozempic have changed the field of medical weight loss, but [the] underlying mechanism actually relies on neural signalling through the vagus nerve.’
So how does this work?
Each fibre of the vagus nerve plays a part in co-ordinating our bodily processes, including digestion and the absorption of nutrients – in this case, via receptors in the stomach and intestines.
The vagus also helps the liver regulate blood sugar levels, courtesy of the portion of the nerve that connects to it. At the same time, another part of the nerve linked to the pancreas regulates the release of insulin.
These all contribute to our body maintaining a healthy weight and blood sugar levels.
Dr Tracey explains that while research is ongoing, the evidence already points to ‘GLP-1 injections’ ability to curb appetite and decrease blood glucose depends on activating vagus nerve circuits that tell the brain and liver to regulate metabolism.’
He points to a key trial involving patients who’d undergone surgery where the vagus nerve is cut to reduce the production of stomach acid (used to treat people with stomach ulcers, for instance).
When they were then given GLP-1s, the drugs had no effect on their food intake, unlike a control group of patients who’d also been given the drugs but not had the surgery.
Similarly, while GLP-1s work by slowing down stomach emptying (which helps people feel full sooner), the surgery group did not experience this, unlike the control group.
‘I expect in future some patients will swap their injections for bioelectronic devices,’ says Dr Tracey.
The great advantage of such devices, he says, is that they are almost entirely free of side-effects, unlike GLP-1 injections which can cause digestive problems such as constipation, nausea, diarrhoea – and, in extreme cases, pancreatitis.
‘When you take a drug it goes everywhere, hence side-effects,’ adds Dr Tracey. ‘Nerve fibres, however, are specific and go in one direction to a specific place for a specific function. So it should be possible to selectively stimulate the vagus nerve fibres someday, to have the benefits without the side-effects.
‘Where GLP-1s require life- long administration and have been linked to muscle loss and unpleasant symptoms, activating the vagus nerve may address obesity without those adverse effects.’
(The risk of overstimulating the nerve is minimal, says Dr Tracey, who points out that such treatment has been effectively used for epilepsy for many years. Potential side-effects include changes in the patient’s voice during the active stimulation and twitching of the lip or neck muscles.)
‘My clinical vision is for devices to supplant GLP-1 injections altogether,’ he says.
‘Realistically, such vagus nerve activating devices for obesity and weight management could be widely available within the next five to ten years, given current progress and investment in bioelectronic medicine.’
Indeed, in terms of targeting the vagus nerve to harness these effects, it may not require an implantable device at all.
In 2021, Dr Tracey published a study in the journal Scientific Reports which, excitingly, showed VNS could potentially help tackle obesity – but instead of a pacemaker-style device like Kelly had, in their experiments on mice they used focused ultrasound.
This is a type of ultrasound directed into the body in a concentrated manner towards a precise target – in this case, where the vagus nerve meets the liver.
After experimenting on 100 mice for 16 weeks, their study showed that focused ultrasound not only caused significant weight loss and reduced inflammatory cytokines, but also tackled belly fat.
(Little wonder that this paper is among the top 2 per cent of scientific papers read or cited by other researchers.)
Dr Tracey explains that the focused ultrasound appears to activate vagus nerve fibres in the liver ‘that convey satiety signals to the brain. Enhancing these signals induces a feeling of fullness more quickly’.
Dr Ahmed Albusoda, a consultant gastroenterologist at Royal London and Whipps Cross Hospital, also has high hopes for the use of VNS in treating gut conditions. A review of studies, which he published in the Journal of Anatomy in 2020, found that VNS can reduce pain, including in the gut.
His team also ran experiments showing that stimulating the vagus nerve could potentially ease IBS pain. He sees VNS as potentially being ‘like physiotherapy for the nervous system’.
He, though, is cautious about the benefits for weight loss: ‘The vagus nerve does play a role in satiety – the sense of fullness after eating – and early research suggests that stimulating certain branches of it can influence gut hormones,’ he says.
‘But at the moment, VNS isn’t remotely as powerful or predictable as GLP-1s. And while there’s research into stimulating parts of the bowel to trigger the body’s own GLP-1 release, sometimes using electrical impulse, this remains experimental.’
That said, it appears that VNS is potentially a very powerful tool. So why isn’t it being widely used?
Part of this is down to the fact that the research into it is ongoing – Dr Tracey says that ‘an avalanche of promising new data is barrelling down the mountain’ – and approval from regulatory bodies such as the FDA will not happen without further proof.
There is also the fact that there is little profit motive for drug companies to push this new technology, he adds.
Dr Albusoda sees further challenges, including the ‘dose’.
‘How strong the pulse should be, how long it should last and where exactly to apply it,’ he says. ‘Until studies become standardised, comparisons are difficult.’
And ‘it is imperative we map the vagus nerve fibres, establishing which parts affect each part of the body’, adds Dr Tracey.
Dr Albusoda says that, despite the hurdles and significant research still to conclude, ‘the evidence is building that the vagus nerve influences pain, inflammation and digestion’.
He believes that even now: ‘I’d like more clinicians to consider vagal function when treating conditions such as IBS, anxiety-related gut symptoms and chronic pain – rather than seeing these problems as purely “in the head” or “in the gut”,’ he says.
‘But with artificial intelligence helping to fine-tune stimulation patterns, I expect the next decade to bring personalised electroceuticals – gentle, data-guided electrical therapies that could sit alongside medicines rather than replace them.’
The future of medicine, then, could lie not in treating symptoms with drugs, but tackling a cause that potentially lies with our vagus nerve.
DIY vagus nerve stimulation
How do you know if your vagus nerve is happy? One key sign, says neurosurgeon Dr Kevin Tracey, is a healthy heart rate, which you can check by checking your pulse (healthy is 60-100 beats per minute). This is known as having high vagal tone.
Signs of ‘low vagal tone’ include being stressed or anxious; you could also have digestive issues such as acid reflux, or raised blood pressure, fatigue and brain fog.
Another way to assess ‘vagal tone’ is by measuring heart rate variability (HRV) – this is the variation in time between individual beats.
This can be done in a hospital setting with an ECG machine, or with a smartwatch or similar (however, experts note that the accuracy of a watch depends on the fit to your wrist). The higher your HRV, the happier your vagus nerve, and – generally – the healthier you are, it seems.
Dr Tracey is evangelical about the impact of exercise on the vagus nerve, suggesting it may help by ‘increasing the vagus nerve signals that activate brain regions associated with enhanced positive emotions – and suppressing depression-causing inflammation’.
He also says that cold-water exposure, meditation and deep breathing all contribute to a healthy vagus nerve, possibly by their impact on the diaphragm, which affects the nerve.
