The prevalence of autism and autism spectrum disorder (ASD) has increased sharply during the past 50 years. In 1978, the population prevalence of infantile autism, diagnosed using the Rutter criteria, was 0.02% among children in the city of Gothenburg, Sweden.1 In contrast, in 2021–2022, the weighted population prevalence of ASD, diagnosed using DSM-5 criteria, was 170 times higher (at 3.42%) among children and adolescents in the US.2 A systematic review and meta-analysis found that the global pooled point prevalence of ASD rose from 0.25% in 1994–1999 to 0.99% in 2015–2019.3
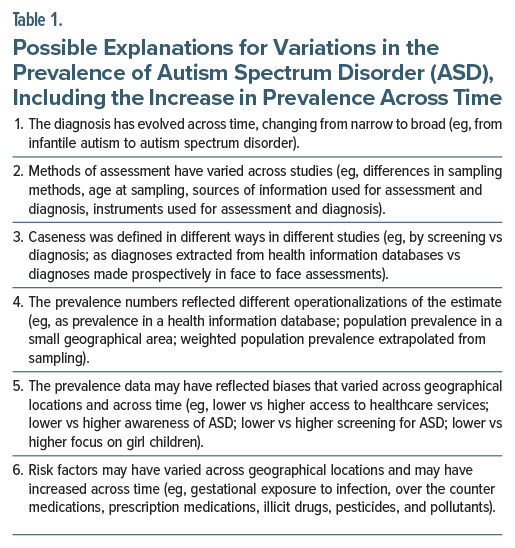
The prevalence of ASD has varied widely across studies. There are many possible explanations for this, including for the increase in prevalence across time4–8; a nonexhaustive list is provided in Table 1.
ASD is considered to be multifactorial in origin, with contributions from both genes and environment. This article considers genetic and environmental risk factors for ASD, with especial focus on environmental risk factors. The interpretation of risks is briefly discussed.
Genetic Risk Factors for Autism Spectrum Disorder
There is little doubt that ASD is a highly heritable, polygenic disorder. At least 12 single nucleotide polymorphisms on 5 candidate genes have been identified in meta-analyses.9 However, hundreds of genes are also likely to be associated with the disorder10,11; in fact, more than a hundred genes are suggested to be shared between ASD and congenital heart disease, alone.12 Furthermore, many of the genetic risk factors associated with ASD are also associated with other neuropsychiatric disorders, including schizophrenia and depression13; this is important because pharmacological agents used in the treatment of these disorders during pregnancy may be associated with (or blamed for) ASD in offspring when the shared genes drive the risk for both maternal mental illness and offspring ASD.14
Environmental Risk Factors for Autism Spectrum Disorder
Many sociodemographic, clinical, gestational, and other environmental risk factors have been associated with an increased risk of ASD; these are at least 50 in number, and total to 100 or more, depending on how one defines the concept of risk; whether one interprets a significant finding to represent a causal variable, a marker variable, or a mediator variable; and how one counts risk factors that tend to go together. For convenience, these will all be listed separately and referred to, generically, as risk factors.
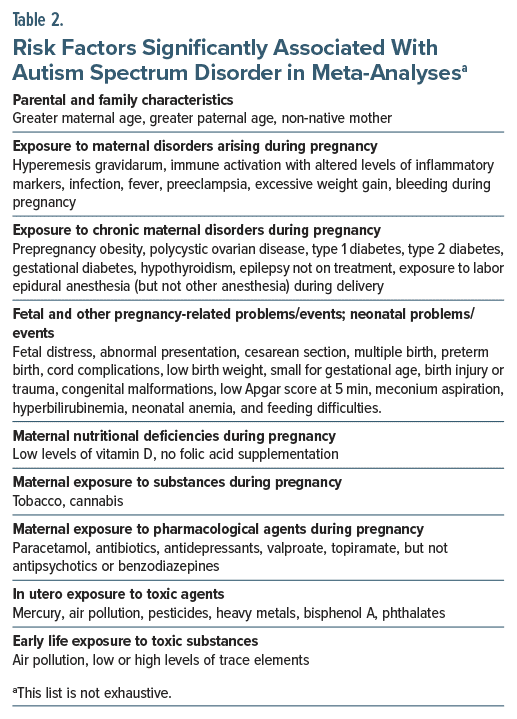
Many risk factors have consistently been associated with increased risk of ASD, where consistent association is operationalized as statistically significant findings obtained from systematic review and meta-analysis (Table 2). These risk factors include parental and family characteristics such as greater maternal age15,16 and greater paternal age15,16; exposure to maternal disorders arising during pregnancy, including hyperemesis gravidarum,17 immune activation with altered levels of inflammatory markers,18 infection,19 fever,20 preeclampsia,21 and excessive weight gain22; exposure to chronic maternal disorders during pregnancy, including (prepregnancy) obesity,23 polycystic ovarian disease,24,25 type 1 diabetes, type 2 diabetes, and gestational diabetes,26 hypothyroidism,27 and epilepsy not on treatment28; exposure to labor epidural anesthesia but not other anesthesia during delivery29; exposure to cesarean section30; pregnancy-related fetal adversities, including preterm birth, low birth weight, and small for gestational age31; possible maternal nutritional deficiencies during pregnancy, including low levels of vitamin D32 and no folic acid supplementation33; exposure to substances such as tobacco34 and cannabis35; exposure to pharmacological agents during pregnancy, including acetaminophen (paracetamol),36 antibiotics,37 antidepressants,38 valproate,39 and topiramate,40 but not antipsychotics41 or benzodiazepines42; in utero exposure to mercury,43 air pollution,44 pesticides,45 heavy metals,46 bisphenol A,47 and phthalates48; and early life exposure to air pollution49 and low or high levels of trace elements.50
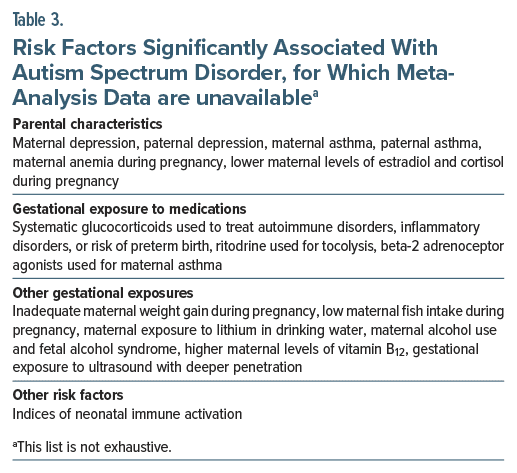
Many recent studies have identified increased risks for which data from meta-analysis are unavailable. These risks (Table 3) include maternal and paternal depression, regardless of time of pregnancy,51 maternal and paternal asthma,52 gestational exposure to ultrasound with deeper penetration,53 gestational exposure to systematic glucocorticoids used to treat autoimmune disorders, inflammatory disorders, or risk of preterm birth,54 gestational exposure to ritodrine used for tocolysis55 and beta-2 adrenoceptor agonists used to treat asthma,56 gestational exposure to maternal anemia,57 lower maternal levels of estradiol and cortisol,58 inadequate weight gain during pregnancy,59 low maternal fish intake during pregnancy,60 maternal exposure to lithium in drinking water,61 maternal alcohol use and fetal alcohol syndrome,62 (surprisingly) higher maternal levels of vitamin B12,63 and indices of neonatal immune activation.64 This is a nonexhaustive list.
Other Risk Factors: Meta-Analyses
Two meta-analyses merit special attention. The first study65 was a meta-analysis of 50 prenatal risk factors extracted from 40 eligible studies. Among these, risk factors significantly associated with offspring ASD were non-native mother, older maternal and paternal age, earlier birth order, and gestational exposure to medications, diabetes, and bleeding during pregnancy. Many of these risk factors were validated in later meta analyses, referenced in a previous section in this article. The other study66 was a meta-analysis of 60 perinatal and neonatal risk factors extracted from the same 40 eligible studies. Among these, risk factors significantly associated with offspring ASD were summer birth, multiple birth, blood group incompatibilities, fetal distress, abnormal presentation, cord complications, birth injury or trauma, maternal hemorrhage, low birth weight, small for gestational age, congenital malformations, low Apgar score at 5 minutes, meconium aspiration, hyperbilirubinemia, neonatal anemia, and feeding difficulties.
These 2 meta-analyses examined data extracted from the same set of studies. One concern with these meta analyses is that many of the risk factors examined (both within and between the 2 meta-analyses) may have been simultaneously present in the same pregnancy; that is, they may not have been independent risk factors. Another concern is that, despite the very large number of risk factors tested (110 in all), no corrections were applied to protect against false positive errors.
Other Risk Factors: an Omnibus Cohort Study
An extraordinary Danish nationwide cohort study67 examined the association of 236 maternal ICD-10 level 3 diagnosis codes (exposures) with ASD in offspring (outcome); the analysis was conducted in several steps and included sibling studies, discordant sibling pair analysis, and paternal negative control analyses.
The sample comprised 648,901 women with 1,131,899 children born in Denmark during 1998–2015; data were drawn from national health registers. Across a median follow-up of 9.7 years, 18,374 (1.6%) children were diagnosed with ASD.
There were 168 maternal nonchronic diagnoses with a prevalence of at least 0.05% during the 12 months before childbirth and 68 maternal chronic diagnoses with a prevalence of at least 0.1% in the 48 months before childbirth. In Cox regression analyses that adjusted for a wide range of sociodemographic variables, 37 of 168 nonchronic and 32 of 68 chronic diagnoses were significantly associated with ASD. After adjusting for multiple hypothesis testing, these numbers reduced to 20 and 22, respectively. These 42 diagnoses included psychiatric, neurological, cardiometabolic, oncological, orthopedic, and other conditions.
In the next step of analysis, all 42 diagnoses along with the sociodemographic covariates were examined together in a single analysis; thus, each diagnosis adjusted for the rest in an exploratory analysis. In this multidiagnosis model, 30 diagnoses, that is, 15 nonchronic and 15 chronic diagnoses, remained significantly associated with ASD.
In the direct sibling analyses, after adjusting for covariates, about three-quarters of the 42 diagnoses were significantly associated with ASD. However, in the exposure-discordant sibling pair analysis, only 3 diagnoses (fracture of the skull and facial bones, maternal care for other fetal problems, and mental disorder, not otherwise specified) remained significantly associated with ASD, suggesting that almost all the associations between maternal diagnoses and ASD could be explained by genetic and environmental risk factors shared between mother and child.
Finally, in the paternal negative control analysis, for 13 out of 17 diagnoses studied, the relationship between parental diagnosis and ASD in offspring was closely similar between mothers and fathers. These results also suggested that almost all the associations between maternal diagnoses and ASD could be explained by genetic and environmental risk factors shared between parents and offspring.
The take-home message from this study67 is that many maternal diagnoses are associated with the risk of ASD in offspring, but the risks appear to be driven by genetic and environmental variables rather than by the diagnoses, themselves. The most important limitation of this study is that it examined maternal diagnoses with no a priori hypotheses based on theoretical cause-effect considerations.
Importantly, the identities of the shared genetic and environmental variables could not be determined in this study.67 Also importantly, the take-home message of this study (see above) cannot be generalized to most of the other risk factors for ASD considered in earlier sections of this article because these risk factors were not maternal diagnoses that were studied by the authors.67
Not Risk Factors
Despite widespread fear in the lay population, data from meta-analyses show that thimerosal in vaccines,43 vaccines in general,68 and the MMR vaccine, in particular,69 are not associated with an increased risk of ASD.
Risk Factors: General Comments
The risk factors listed in this article are not exhaustive; there are exposures examined in occasional studies, not all of which have been associated with increased risk, and these are too many to list. There are also risk factors within a group that have been studied separately (eg, different pollutants or pesticides under the general umbrella of air pollution or pesticides) that, with a view to reducing information overload, have deliberately not been separately presented in this article.
Many risk factors aggregate, such as low socioeconomic status, maternal malnutrition, inadequate maternal weight gain during pregnancy, low levels of nutrients in maternal blood, etc; or, preterm birth, small for gestational age, and low birthweight. Such groupings can perhaps be represented by a single construct. It may also not be meaningful to deconstruct gestational, labor, or neonatal adversities into individual events and experiences unless there is a theoretical reason to do so; it is possible that physiological stresses increase the risk of ASD through shared or overlapping mediatory pathways.
Many risk factors studied are not necessarily risk factors; they may be either markers of risk or mediators of risk. As an example, maternal autoimmune disease, maternal infection, and fever during pregnancy; maternal use of antibiotics and acetaminophen during pregnancy; changes in levels of immune and inflammatory molecules; and changes in the gut microbiome have all been associated with ASD risk. However, although speculation is possible, it cannot be asserted with certainty which of these are the primary risk factors, which are merely markers, and which are mechanisms. It is also uncertain to what extent significant findings are due to confounding by genetic factors, confounding by indication or the severity thereof, and confounding by unmeasured and unknown risk factors. Readers may wish to refer to general reviews on the subject.70,71
The referencing of meta-analyses and studies in previous sections is not an endorsement of infallibility. No meta-analysis, no study in a meta-analysis, and no standalone study is perfect. Every study needs to be understood in the context of its sample and the population that the sample represents; in its methodological context, and in the context of its strengths and limitations. As a special point, there is much difference between the concept of autism in early studies and the concept of ASD in current research. Therefore, the interpretation of all findings must necessarily be nuanced. This, of course, is true of all research but is especially important in the context of the etiopathogenesis of ASD because of the enormous heterogeneity evident herein.
Furthermore, on the subject of nuanced interpretations, in meta-analysis,38 gestational exposure to antidepressants was associated with an increased risk of ASD in offspring; however, in the same meta-analysis, prepregnancy exposure to antidepressants was also associated with increased risk. This implies that genetic or environmental factors, shared between mother and child, rather than antidepressant exposure, drive the ASD risk. As another example, evidence associating maternal smoking with ASD risk is indirect. In a meta-analysis,34 maternal smoking during pregnancy increased the risk of ASD in offspring, but the risk narrowly missed statistical significance. However, when population-level smoking metrics were included in meta-regression, the risk was statistically significant. Separately, in a large cohort study,72 the risk of ASD associated with gestational exposure to cannabis was reduced by about 60% in tobacco smokers, suggesting that tobacco use also plays a substantial role as a risk factor for ASD.
Parting Notes
This article has made no attempt to speculate on how different risk factors can be integrated in the etiopathogenesis of ASD; current understanding of ASD is insufficient to undertake such a task. This article has deliberately refrained from presenting values for risk for individual risk factors; that is, odds ratios, hazard ratios, and their 95% confidence intervals. This is deliberate because the subject is important and will be addressed in the next article in this column.
Article Information
Published Online: April 14, 2025. https://doi.org/10.4088/JCP.25f15878
© 2025 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Autism spectrum disorder, 1: genetic and environmental risk factors. J Clin Psychiatry 2025;86(2):25f15878.
Author Affiliations: Department of Psychiatry, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India; Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India.
Corresponding Author: Chittaranjan Andrade, MD, Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore 560029, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India. Please contact Chittaranjan Andrade, MD, at Psychiatrist.com/contact/andrade.
Financial disclosure and more about Dr Andrade.