Sepsis is a life-threatening complication that affects patients in both inpatient and outpatient settings. This study demonstrates several findings regarding sepsis-related mortality rates in the United States from 1999 to 2022. First, men and women both experienced significant increases in mortality rates, with men experiencing higher rates compared to women. Second, the differences in mortality rates among different ethnicities were prevalent, and it was found that African Americans experienced the highest mortality rates overall due to sepsis. Lastly, geographic differences based on census regions were found, with the highest mortality related to sepsis in the South.
Gender
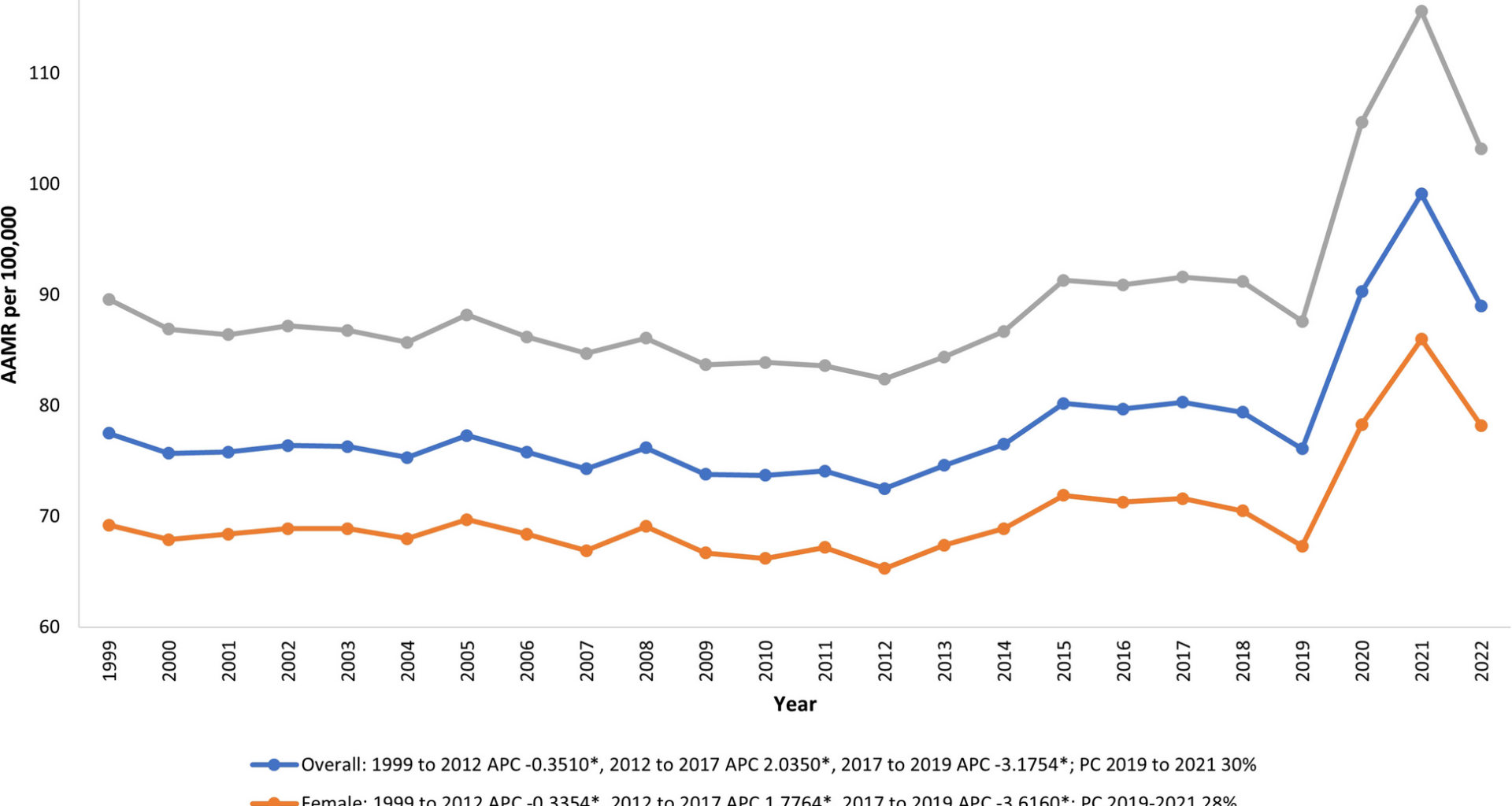
Evaluation of AAMR in sepsis-related mortality demonstrate that men and women had an increase in mortality rates from 1999–2022, but men had overall higher rates of mortality. This can likely be attributed to men being more likely than women to engage in high-risk behaviors, such as smoking, drinking, and using illicit drugs. Men are also less likely to utilize healthcare services such as emergency department visits and preventative health care visits. [7] Another study demonstrates that men are also more likely to have more lethal conditions, such as heart disease, stroke, and diabetes, which could be comorbid with sepsis [8]. This is especially pertinent considering that these lethal conditions can cause greater susceptibility to infection and sepsis or lead to hospitalizations that expose patients to iatrogenic infections. It is important to understand how men and women are both facing increased risk of susceptibility to sepsis as time progresses as well as address the behaviors that may put members of both sexes at risk for sepsis, particularly men more so than women.
Race
The AAMR in sepsis-related deaths closely mirror the racial inequalities in the United States. Minority racial groups such as the African American, the Native American, and the Hispanic populations had the highest AAMRs between the years of 1999 to 2019 compared to the NH White population. All racial groups experienced an increased in AAMR during the COVID- 19 pandemic. Between 1999 and 2019, minority groups with the highest AAMR could be explained by socioeconomic status, in which minorities in the United States are generally in a lower socioeconomic status (SES) [9, 10]. Perhaps the additional strain of the pandemic on United States’ social support systems as well as the strain to the hospital system resources may have led to diminishing health outcomes in regards that go beyond COVID- 19 itself, including sepsis [11, 12]
Previously published epidemiological studies have demonstrated that NH White patients experience disproportionately better outcomes with sepsis compared to other racial groups. The NH White population had the lowest overall AAMR of all racial groups during the study period; however, this population experienced a significant APC from 2012 to 2019 [13]. The APC from 2012 to 2019 likely cannot be explained by a single factor [14]. Some factors that may play a role in this increase in sepsis-related deaths in the NH White population include the opioid pandemic and other substance abuse. In one study conducted from epidemiological data in Michigan, 74.7% of sepsis cases in the setting of substance abuse were attributed to the NH White population [15].
Age groups
In our analysis of varying age groups, the elderly group (≥ 75 years) had the highest AAMR, followed by the middle-aged group (45–75 years), and lastly, the young age group (25–44 years). This trend in increased mortality with advanced age is not surprising. Interestingly, there was an increase in APC from 2014 to 2022 for the young age group. The rise in sepsis mortality in the younger adult populations may be in part due to an increase in IV drug usage (IVDU). One study investigating the relationship between drug abuse and infective endocarditis found that drug abuse-related cases of infective endocarditis essentially doubled between 2002 and 2016 [16]. The average age of those with drug abuse-related endocarditis was 38 years old compared to non-drug abuse-related endocarditis at 70 years old [16]. IVDU can serve as a nidus for bacteremia and, by extension, sepsis in the young population. This increase in drug abuse-related infective endocarditis cases could be an indicator that rising drug abuse in young people has contributed to a rise in sepsis mortality in the young age range.
Regional variations
We evaluated AAMR in the setting of sepsis based on the four major United States regions: the South, Midwest, West, and Northeast. The region with the greatest AAMR was the South. A previously published study that investigated sepsis-related deaths also found that mortality was highest in the American South, particularly in non-metropolitan areas [17]. This adds to our understanding that those who reside in more rural areas, the American South, for example, are at a disadvantage in terms of access to healthcare. However, this concept is challenged by our data, which shows that the Northeast region has the second highest AAMR of all the US regions. The Northeast is a region with a high density of major metropolitan areas; however, limited access to care in more rural areas, such as in the Appalachian states, could contribute to the high AAMR. Another contributing factor could be low-income areas in large metropolitan areas. For example, the same study found that in Baltimore, Maryland, sepsis-related deaths were significantly higher in low-income areas compared to high-income regions [17]. These findings demonstrate that socioeconomic status is an essential factor in sepsis-related outcomes, including mortality.
COVID- 19
Across the different demographics analyzed in this study, there was a universal increase in sepsis-related mortality from 2019 to 2022. This timeframe coincides with the recent COVID- 19 pandemic, which likely magnified the number of patients passing away from sepsis. This is consistent with our sensitivity analysis, in which the COVID- 19 pandemic appeared to contribute to the increase in sepsis-related deaths from 2019–2022. One study identified COVID- 19 as an independent risk factor for increased in-hospital mortality in septic patients [18]. Another study, however, discusses that the occurrence of sepsis among decedents with COVID- 19 in the US may be vastly underestimated as so many cases of sepsis may not have been accounted for. This may be due to the clinicians being less certain about their diagnostic skills in the face of the novel COVID- 19 pandemic [19].
Sepsis and associated causes of death
In our analysis of sepsis mortality and associated causes of death, several findings emerged, including an increase in contribution from pneumonia both before and during the pandemic from 20.77% in 1999–2001 to 23.71% in 2017–2019 and further to 27.63% in 2020–2022. Perhaps the rise in COVID- 19 infections, in conjunction with the strain the pandemic imposed on the US healthcare system, led to an increase in deaths from sepsis in the setting of pneumonia [11]. This rise parallels the contribution from heart failure, which rose from 8.08% from 1999–2001, 9.64% from 2017–2019, and 9.87% from 2020–2022. In the United States, there has been an increase in both heart failure deaths and heart failure deaths with concurrent sepsis over the past two decades [20, 21]. Interestingly, there was a sharp decline in deaths due to sepsis associated with chronic lower respiratory tract diseases in 2020–2022 at 1.50% of all sepsis deaths compared to 2017–2019 at 7.49% of all sepsis deaths. It can be speculated that this sharp decline in deaths due to sepsis associated with chronic lower respiratory tract diseases was due to those with chronic lower respiratory tract diseases are at a higher risk of severe COVID- 19 infection and likely dying from a severe COVID- 19 infection rather than from their chronic disease [22]. In addition, there was an initial increase in mortality of urinary tract infections (UTI) in the setting of sepsis from 7.75% in 1999–2001 to 11.26% in 2017–2019, followed by a slight decrease to 11.02% from 2020–2022.
Strengths and limitations
This study’s strengths were primarily based on the utilization of the CDC WONDER database, which captures almost all US mortality, thus allowing us to provide a comprehensive analysis of trends and differences in mortality rates due to sepsis, associated comorbidities and causes of deaths, and the changes due to pandemic. The limitations include misclassification bias due to its reliance on ICD- 10 codes. It also lacks information on potential confounders. Lastly, the data regarding Asians and Pacific Islanders as separate racial groups were available only from 2018 onward.