‘My arms end up black and blue and really sore’ says patient who welcomes the change
Kirstie McCrum Network Content Editor
14:55, 13 May 2025
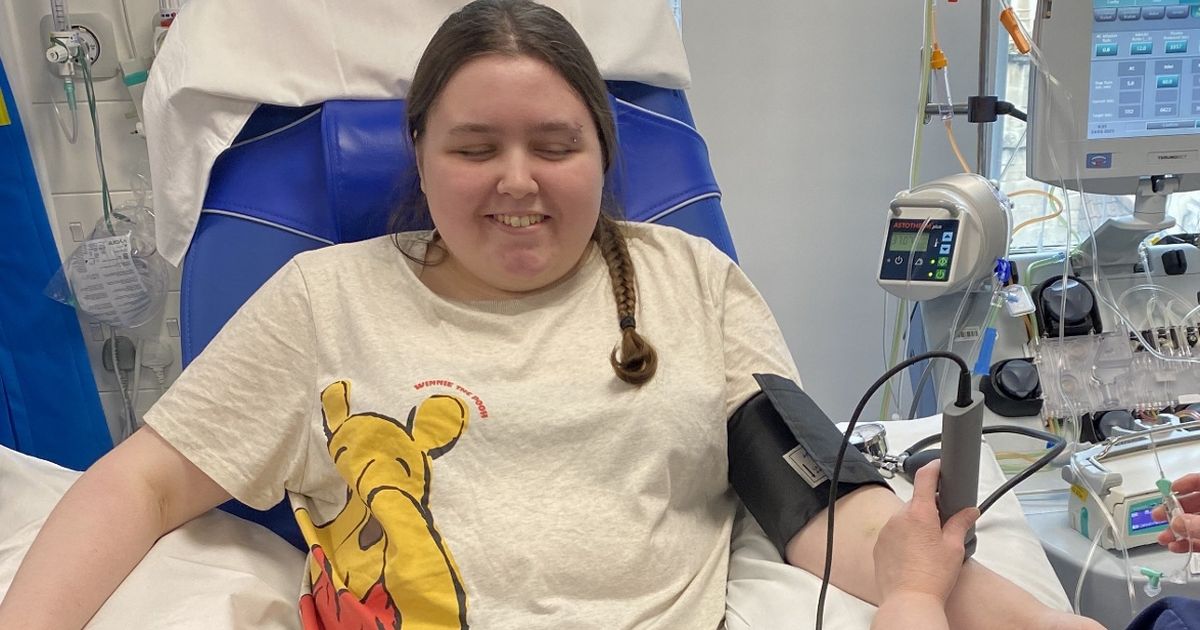
 A TAS nurse using ultrasound to canulate Tegan Rendell ahead of her plasma exchange(Image: NHSBT)
A TAS nurse using ultrasound to canulate Tegan Rendell ahead of her plasma exchange(Image: NHSBT)
A new ultrasound service which will see fewer patients need to go into surgery has proven a success for the NHS in Bristol. The NHS Blood and Transplant (NHSBT) Therapeutic Apheresis Services (TAS) unit has been providing the service which is also said to reduce the time patients spend in hospital, improves patient safety and experiences and saves the NHS money.
The team, housed in the Bristol Haematology and Oncology Centre, used ultrasound guided canulation so successfully that the system was rolled out among the eight other TAS units across England. The technique can help patients with a number of illnesses including sickle cell disease and blood cancers.
In a statement, the NHS said: “In an eight-month period, ultrasound guided canulation was used 177 times for 57 different patients or donors within the Bristol TAS unit. All of the canulations were successful and 96 central lines were avoided, saving the NHS approximately £43,000.”
This success inspired the rollout of an ultrasound guided canulation training programme across the eight other TAS units across the country. It is thought over 200 central lines have been avoided since the training began in May 2023.
In addition, patients save up to half a day of time spent in hospital on every visit and avoid needing to go into theatre for line insertion and removals. In ultrasound guided canulation, a nurse will use an ultrasound machine to find a vein which cannot normally be found.
 TAS nurses Sam Ntakirutimana (left) and Daniel Putensen (right) rolled out the training(Image: NHSBT)
TAS nurses Sam Ntakirutimana (left) and Daniel Putensen (right) rolled out the training(Image: NHSBT)
The nurse is then able to see the cannula being placed into the vein in real-time, avoiding the need for multiple attempts at canulation and reducing discomfort for patients.
Tegan Rendell, 20, attends Bristol’s Therapeutic Apheresis Services every eight weeks, for a plasma exchange to treat Autoimmune Limbic Encephalitis, an autoimmune disease that attacks her brain.
She says: “My illness mean I need to undergo a lot of medical procedures and it can be really traumatic as my veins are so difficult to find. There have been occasions where medics have tried to cannulate nine times and still not been successful, it’s awful.
“My arms end up black and blue and really sore. Having regular plasma exchanges is life changing for me – my quality of life is so much better after each one. I have fewer seizures, less headaches and generally feel so much better within myself.
“Even so, if I knew I faced the trauma of repeated cannulation attempts every time I needed a plasma exchange, I would really struggle. But ultrasound guided cannulation – and the incredible nurses who do it – make my experience so much better than it might otherwise be.
“The cannulation is quick and easy and I don’t spend the whole eight weeks dreading the next appointment. I’ve been visiting the wonderful TAS Bristol team every eight weeks for three years now and I can see just how widely used the ultrasound guided canulation is and how many people it helps. I’m so glad it’s been successfully rolled out across all of the units and can help so many more patients.”
 A Bristol NHS team has been used as a blueprint for the roll out of a service that means fewer patients need surgery, improving patient experience and saving the NHS money(Image: NHSBT)
A Bristol NHS team has been used as a blueprint for the roll out of a service that means fewer patients need surgery, improving patient experience and saving the NHS money(Image: NHSBT)
Teresa Baines, Head of Therapeutic Apheresis Services at NHS Blood and Transplant, says: “Ultrasound guided canulation is a complex, technical skill and we’re proud to have rolled it out, via a programme of training, across all nine of our units. The benefits to the patient are profound and the feedback from them has been extremely positive.
“A lot of our patients come to us for regular treatments and so to be able to avoid multiple attempts at canulation or being taken to surgery for line insertion (and later removal) on every visit, makes a huge difference to the quality of their care. They’re reporting feeling much more comfortable, spending less time in hospital and generally having less dread around upcoming procedures and that is all that we can ask for.
“Bristol is one of our busiest units and yet had the lowest rate of central line insertions thanks to this method and so we knew that theirs was a formula we wanted to roll out across the whole of TAS. We’re so grateful to everybody involved in making it such a success and we look forward to continuing to train and develop our teams to ensure our patients are the most comfortable they can be when with they’re with us.”
Sam Ntakirutimana, Education and Training Lead Nurse at TAS, who routinely uses ultrasound guided canulation in patient care and rolled out the training to all nine units, says: “Rolling out this training throughout all of our units, has made a huge difference for our patients. Though our teams are highly skilled in cannulation, there are occasions where you cannot see or feel a vein, meaning a patient would need to have a central line inserted.
“Using the ultrasound to find veins, that are sometimes even just a few millimetres below the skin, ensures that our patients have a better overall experience – the feedback from them has been fantastic and as their care team, that’s delightful to hear. Ultrasound guided cannulation is something that our Bristol team is highly skilled in and has been using with great success, so it was only right that we expanded the service throughout all of our sites.
“It took one year of intensive training, but we are proud to say that every one of our units now has at least one team member who can use the ultrasound to cannulate when veins are harder to find and that this has led to a huge reduction in the number of patients needing to have a central line fitted. Our aim now is to get every TAS nurse trained up in the skill, to continue to improve patient experience, reduce numbers of central lines being fitted and save the NHS money.”
Ultrasound guided canulation is now being used at all nine TAS units across England. The rollout will continue with an ambition to train all NHSBT TAS nurses over the coming year. For more information on TAS, visit nhsbt.nhs.uk.