TOPLINE:
US hospitalizations related to cervical artery dissection (CeAD) increased more than fourfold between 2005 and 2019, suggested a new study that also showed vertebral artery dissection was associated with a significant increase in acute ischemic stroke risk.
METHODOLOGY:
- Researchers included more than 125,000 patients with spontaneous CeAD (mean age, 51.4 years; 54% men).
- All participants were identified through the National Inpatient Sample database between 2005 and 2019 to determine national trends in CeAD admissions and examine post-CeAD risk for ischemic stroke.
- About 65% of participants were White, 10% were Black, 8% were Hispanic, 3% were Asian or Pacific Islander, and 14% were of other races.
- The National Readmission Database and State Inpatient Database of New York and Florida were used to track outcomes of acute ischemic stroke among patients and verify national estimates.
TAKEAWAY:
- The incidence of CeAD increased dramatically from 2005 to 2019 (10.7-45.6 cases per million population), showing an average annual percent change (AAPC) of 10% nationally and 9% at the state level.
- Black populations showed the greatest increase in CeAD-related hospitalization (AAPC, 17.9%), followed by Asian or Pacific Islander (AAPC, 14.1%), Hispanic (AAPC, 13.4%), and White (AAPC, 12.6%) populations.
- The increase in incidence of CeAD was greater among patients aged 65 years or older than among their younger counterparts (AAPCs, 12% vs 8%, respectively).
- In patients with CeAD but without acute ischemic stroke, vertebral artery dissection was the sole major predictor of increased risk for a subsequent stroke within 90 days (adjusted subdistribution hazard ratio, 1.8; P = .006).
IN PRACTICE:
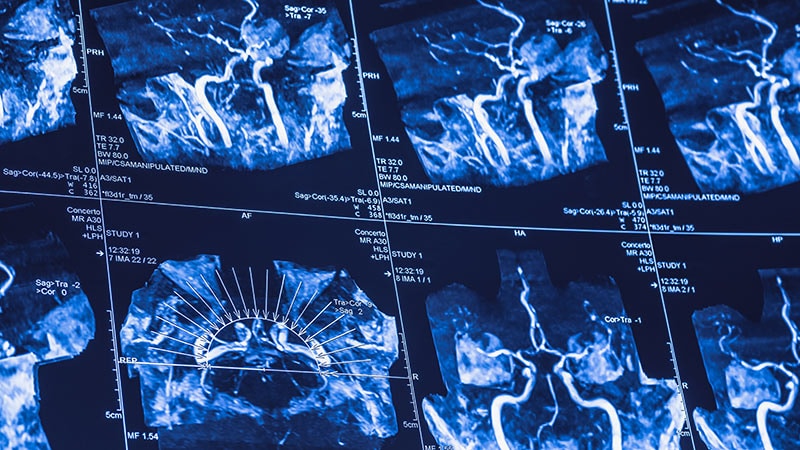
“Possible reasons for this nearly fivefold increase over 15 years include greater awareness of cervical artery dissection by healthcare professionals, better access to imaging to help identify it, and an overall increase in this condition for which a cause has yet to be determined,” corresponding investigator Shadi Yaghi, MD, said in a press release.
SOURCE:
The study was led by Liqi Shu, MD , The Warren Alpert Medical School of Brown University, Providence, Rhode Island. It was published online on April 02 in Neurology.
LIMITATIONS:
The study’s reliance on hospital admission records may have led to the underestimation of the incidence of CeAD due to undiagnosed or nonadmitted cases being missed. Diagnostic coding errors may have led to a potential bias. Inconsistencies in racial classification and lack of core lab diagnostic confirmation may have affected result accuracy. Missing data on medications, diagnostic workup, dissection laterality, and antithrombotic use further limited the analyses of risk factors and outcomes. Additionally, incomplete patient tracking and the absence of imaging predictors of stroke may have reduced precision.
DISCLOSURES:
The study was funded by the National Institute of Neurological Disorders and Stroke. Several investigators reported financial or professional ties with various sources. Full details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.