Oral care often feels limited to brushing teeth or visiting a dentist. Many people view mouth health as separate from brain health.
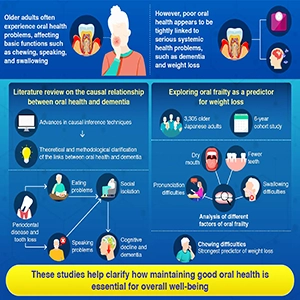
New research from the Institute of Science Tokyo is challenging that idea. The experts have found strong links between oral problems, social life, nutrition, and dementia risk.
Poor chewing or speech may quietly shape daily habits, social contact, and long-term brain health.
Oral problems grow with age
Aging often leads to tooth loss, dry mouth, weak jaw muscles, and swallowing problems. Such changes reduce chewing strength and make speech less clear.
Eating can become slow and uncomfortable, while speaking may feel tiring or embarrassing.
Modern dentistry can treat many oral problems. However, limited access, low awareness, or high costs still prevent many older adults from receiving proper care.
Poor oral function can reduce food intake and lower diet quality. Soft foods may replace protein-rich meals. Speech difficulty can lead to avoiding conversations.
Over time, daily activities become limited and social contact gradually decreases.
Oral health and dementia risk
Many population studies report a clear link between poor oral health and dementia risk. Dementia affects memory, language, judgment, and daily independence.
Researchers debate the direction of cause. Cognitive decline can weaken oral hygiene habits. At the same time, oral problems may increase dementia risk through several pathways.
Earlier research focused mainly on biology. Scientists studied mouth bacteria, gum disease, inflammation, and nerve signals from chewing. Some animal studies support such pathways.
Human intervention studies show mixed results. Gum treatment does not always improve broader health outcomes. Such findings raise questions about whether biology alone explains dementia risk.
Oral health in early life
The current study, led by Professor Jun Aida, highlights an important challenge in dementia research. Early life cognitive ability can influence education, health behavior, and oral care habits later in life.
Lower cognitive ability during childhood links with poorer dental care during adulthood and higher tooth loss during old age. Early cognitive differences also relate to dementia risk many decades later.
Such early factors can confuse cause and effect. Tooth loss may signal early vulnerability rather than act as a direct cause. Modern epidemiology uses advanced methods to address such issues.
Long-term repeated surveys, fixed effects analysis, and instrumental variable approaches help separate oral health effects from lifelong background factors.
Several studies using such methods still show oral decline predicting later cognitive decline.
Eating shapes social connection
The most important contribution of recent research lies in social mechanisms. Oral function supports daily social life. Eating and speaking allow shared meals, conversation, and emotional connection.
“These functions have a social aspect that facilitates interpersonal interactions and can reduce social isolation,” explained Aida.
“When we consider the multilayered direct and indirect mechanisms leading to dementia throughout life, we find that poor oral health possibly increases the risk of dementia through social isolation via eating and speaking problems.”
Difficulty chewing often leads to eating alone, which raises weight loss risk. Weight loss contributes to frailty.
Frailty increases dementia risk, while speech difficulty reduces conversation frequency and confidence.
Reduced interaction increases loneliness. Social isolation ranks among the major modifiable dementia risk factors worldwide.
Nutrition, oral health, and dementia
Chewing ability strongly shapes diet quality. Tooth loss and jaw weakness limit intake of protein, vegetables, and textured foods.
Long-term poor nutrition weakens muscle, immunity, and brain resilience. Protein intake shows an inverse association with dementia risk in older adults.
The six-year Japanese study, involving more than 3,000 older adults, showed chewing difficulty as the strongest predictor of weight loss among oral frailty signs.
Dry mouth and missing teeth played roles, yet chewing difficulty showed the strongest effect. Weight loss increases frailty, and frailty raises dementia risk.
 Insights into the links between oral health, systemic issues, and dementia. Credit: ISCT. Click image to enlarge.Prevention may start orally
Insights into the links between oral health, systemic issues, and dementia. Credit: ISCT. Click image to enlarge.Prevention may start orally
Dementia develops through combined biological, behavioral, and social pathways across life.
Education, physical activity, hearing, vision, diet, and social contact all matter. Oral health interacts with many of these factors.
Unlike childhood education or genetics, oral health can improve even during later life. Dentures, oral rehabilitation, and preventive dental care can restore eating ability and social participation.
Observational studies show denture use reducing social isolation and weakening links between tooth loss and cognitive impairment.
Oral diseases remain among the most common conditions worldwide. High prevalence means even modest risk effects can influence population health. Improving oral care may support nutrition, social life, and cognitive resilience.
More than a healthy smile
Oral health supports far more than smiles. Eating, speaking, and social connection depend on healthy oral function.
Strong evidence now shows oral care as part of dementia prevention strategies.
Protecting teeth and oral function may help protect memory, independence, and quality of life during aging.
The study is published in the Journal of Dental Research.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–

