Lawton E. The history of the medical legal partnership movement. Community Health Forum, National Association of Community Health Centers; 2014. https://medical-legalpartnership.org/wp-content/uploads/2015/01/NACHC-Magazine-A-History-of-the-Medical-Legal-Partnership-Movement.pdf.
National Center for Medical Legal Partnership. Washington, D.C.: Milken Institute School of Public Health, The George Washington University; 2024. https://medical-legalpartnership.org/partnerships/.
Gitterman B. Medical-legal partnership: promoting child health through preventative law. Honolulu, Hawaii: American Academy of Pediatrics Annual Leadership Forum; 2007. https://medical-legalpartnership.org/wp-content/uploads/2014/02/American-Academy-of-Pediatrics-MLP-Resolution.pdf.
DeMuro P. American Bar Association Health Law Section Report to the House of Delegates. Washington, D.C.: National Center for Medical-Legal Partnership, The George Washington University, 2007. https://medical-legalpartnership.org/wp-content/uploads/2014/02/American-Bar-Association-MLP-Resolution.pdf.
Thomson J, Shah SS, Simmons JM, Sauers-Ford HS, Brunswick S, Hall D, et al. Financial and social hardships in families of children with medical complexity. J Pediatr. 2016;172:187–93.e1.
Williams E. 5 Key Facts About Children with Special Health Care Needs and Medicaid. KFF.org; 2025. https://www.kff.org/medicaid/issue-brief/5-key-facts-about-children-with-special-health-care-needs-and-medicaid/
Kuo DZ. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165:1020.
Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133:431–9.
Yama CL, Greenberg RG, Johnson E, Mago-Shah DD. Social needs and healthcare utilization in NICU graduates. J Perinatol. 2024;44:1732–7.
King BC, Mowitz ME, Zupancic JAF. The financial burden on families of infants requiring neonatal intensive care. Semin Perinatol. 2021;45:151394.
Lapcharoensap W, Lee HC, Nyberg A, Dukhovny D. Health care and societal costs of bronchopulmonary dysplasia. NeoReviews. 2018;19:e211–23.
Lakshmanan A, Song AY, Belfort MB, Yieh L, Dukhovny D, Friedlich PS, et al. The financial burden experienced by families of preterm infants after NICU discharge. J Perinatol. 2022;42:223–30.
Shah S, Kuo AA, Brumberg HL. First aid for Medicaid: losses in children’s health insurance. Pediatr Res. 2021;89:8–11.
Ryan AM, Kutob RM, Suther E, Hansen M, Sandel M. Pilot study of impact of medical-legal partnership services on patients’ perceived stress and wellbeing. J Health Care Poor Underserved. 2012;23:1536–46.
Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children: outcomes from a successful partnership between professions. J Health Care Poor Underserved. 2013;24:1063–73.
Sege R, Preer G, Morton SJ, Cabral H, Morakinyo O, Lee V, et al. Medical-legal strategies to improve infant health care: a randomized trial. Pediatrics. 2015;136:97–106.
Beck AF, Henize AW, Qiu T, Huang B, Zhang Y, Klein MD, et al. Reductions in hospitalizations among children referred to a primary care–based medical-legal partnership: study examines hospitalizations among children who are referred to a primary care-based medical-legal partnership. Health Aff. 2022;41:341–9.
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in Black, White, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269.
Boghossian NS, Geraci M, Lorch SA, Phibbs CS, Edwards EM, Horbar JD. Racial and ethnic differences over time in outcomes of infants born less than 30 weeks’ gestation. Pediatrics. 2019;144:e20191106.
Janevic T, Zeitlin J, Auger N, Egorova NN, Hebert P, Balbierz A, et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 2018;172:1061–9.
Wallace ME, Mendola P, Kim SS, Epps N, Chen Z, Smarr M, et al. Racial/ethnic differences in preterm perinatal outcomes. Am J Obstet Gynecol. 2017;21:306.e1–e12.
MacDorman MF, Mathews TJ. Understanding racial and ethnic disparities in U.S. infant mortality rates. NCHS Data Brief. Hyattsville, MD; U.S. Department of Health and Human Services, Center for Disease Control and Prevention, National Center for Health Statistics; 2011.
Matthews TJ, Ely DM, Driscoll AK. State variations in infant mortality by race and hispanic origin of mother, 2013-2015. NCHS Data Brief. 2018;295:1–8.
Willis E, McManus P, Magallanes N, Johnson S, Majnik A. Conquering racial disparities in perinatal outcomes. Clin Perinatol. 2014;41:847–75.
Prepared by Mary C. Slosar, Slosar Research, LLC. The Justice Gap: The Unmet Civil Legal Needs of Low-income Americans. Legal Services Corporation. Washington D.C.: 2022. https://justicegap.lsc.gov/the-report/.
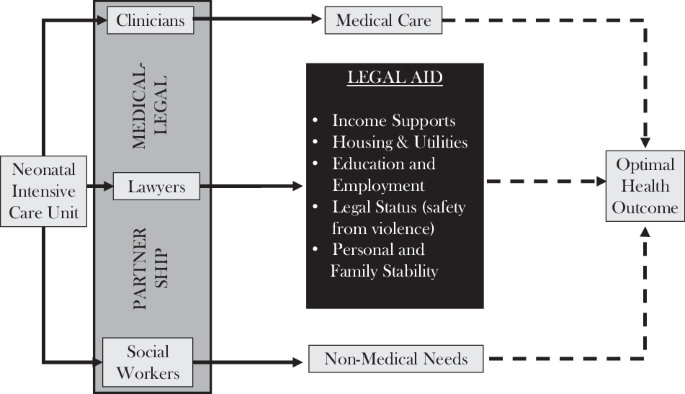
Gievers L, Mutrie L, Klawetter S. Novel perinatal medical-legal partnership development and pilot implementation to address health-harming legal needs. J Perinatol. 2024;44:136–41.
Prouhet PM, Gregory MR, Russell CL, Yaeger LH. Fathers’ stress in the neonatal intensive care unit: a systematic review. Adv Neonatal Care. 2018;18:105–20.
Bernardo J, Rent S, Arias-Shah A, Hoge MK, Shaw RJ. Parental stress and mental health symptoms in the NICU: recognition and interventions. NeoReviews. 2021;22:e496–505.
Haward MF, Lantos J, Janvier A. for the POST Group. Helping parents cope in the NICU. Pediatrics. 2020;145:e20193567.
Medicaid and CHIP Payment and Access Commission. Issue brief: Advising Congress on Medicaid and CHIP policy, prior authorization in Medicaid. 2024. https://www.macpac.gov/wp-content/uploads/2024/08/Prior-Authorization-in-Medicaid.pdf.
Schpero WL, Brahmbhatt D, Liu MX, Ndumele CD, Chatterjee P. Variation in procedural denials of medicaid eligibility across states before the COVID-19 pandemic. JAMA Health Forum. 2023;4:e233892.
Klibanoff E. Despite warnings, Texas rushed to remove millions from Medicaid. Eligible resident lost care. Austin, Texas: The Texas Tribune; 2024. https://www.texastribune.org/2024/09/26/texas-medicaid-unwinding-consequences/.
Mainardi AS, Harris D, Rosenthal A, Redlich CA, Hu B, Fenick AM. Reducing asthma exacerbations in vulnerable children through a medical–legal partnership. J Asthma. 2023;60:262–9.
Regenstein M, Trott J, Williamson A, Theiss J. Addressing social determinants of health through medical-legal partnerships. Health Aff. 2018;37:378–85.
Regenstein M. The state of the medical-legal partnership field. Washington, D.C.: George Washington University; 2017. https://medical-legalpartnership.org/wp-content/uploads/2017/07/2016-MLP-Survey-Report.pdf.
Tsai D. Coverage of services and supports to address health-related social needs in medicaid and the children’s health insurance program [Internet]. Baltimore, Maryland: Department of Health and Human Services, Centers for Medicare and Medicaid Services; 2023. https://www.medicaid.gov/federal-policy-guidance/downloads/cib11162023.pdf.