Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and Longer-Term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STAR*D Report. AJP. 2006;163:1905–17.
Garcia-Marin LM, Mulcahy A, Byrne EM, Medland SE, Wray NR, Chafota F, et al. Discontinuation of antidepressant treatment: a retrospective cohort study on more than 20,000 participants. Ann Gen Psychiatry. 2023;22:49.
Tansey KE, Guipponi M, Hu X, Domenici E, Lewis G, Malafosse A, et al. Contribution of common genetic variants to antidepressant response. Biol Psychiatry. 2013;73:679–82.
Jukić MM, Haslemo T, Molden E, Ingelman-Sundberg M. Impact of CYP2C19 Genotype on Escitalopram Exposure and Therapeutic Failure: A Retrospective Study Based on 2,087 Patients. Am J Psychiatry. 2018;175:463–70.
Islam F, Marshe VS, Magarbeh L, Frey BN, Milev RV, Soares CN, et al. Effects of CYP2C19 and CYP2D6 gene variants on escitalopram and aripiprazole treatment outcome and serum levels: results from the CAN-BIND 1 study. Transl Psychiatry. 2022;12:1–11.
Calabrò M, Fabbri C, Kasper S, Zohar J, Souery D, Montgomery S, et al. Metabolizing status of CYP2C19 in response and side effects to medications for depression: Results from a naturalistic study. Eur Neuropsychopharmacol. 2022;56:100–11.
Campos AI, Byrne EM, Mitchell BL, Wray NR, Lind PA, Licinio J, et al. Impact of CYP2C19 metaboliser status on SSRI response: a retrospective study of 9500 participants of the Australian Genetics of Depression Study. Pharmacogenomics J. 2022;22:130–5.
Fabbri C, Tansey KE, Perlis RH, Hauser J, Henigsberg N, Maier W, et al. Effect of cytochrome CYP2C19 metabolizing activity on antidepressant response and side effects: Meta-analysis of data from genome-wide association studies. Eur Neuropsychopharmacol. 2018;28:945–54.
Mrazek DA, Biernacka JM, O’Kane DJ, Black JL, Cunningham JM, Drews MS, et al. CYP2C19 variation and citalopram response. Pharmacogenet Genomics. 2011;21:1–9.
Joković D, Milosavljević F, Stojanović Z, Šupić G, Vojvodić D, Uzelac B, et al. CYP2C19 slow metabolizer phenotype is associated with lower antidepressant efficacy and tolerability. Psychiatry Res. 2022;312:114535.
Brandl EJ, Tiwari AK, Zhou X, Deluce J, Kennedy JL, Müller DJ, et al. Influence of CYP2D6 and CYP2C19 gene variants on antidepressant response in obsessive-compulsive disorder. Pharmacogenomics J. 2014;14:176–81.
Hodgson K, Tansey K, Dernovšek MZ, Hauser J, Henigsberg N, Maier W, et al. Genetic differences in cytochrome P450 enzymes and antidepressant treatment response. J Psychopharmacol. 2014;28:133–41.
Kamp M, Lo CWH, Kokkinidis G, Chauhan M, Gillett AC, AMBER Research Team, et al. Sociodemographic, clinical, and genetic factors associated with self-reported antidepressant response outcomes in the UK Biobank [Internet]. [cited 2024 Nov 1]. Available from: http://medrxiv.org/lookup/doi/10.1101/2024.10.23.24315970 (2024).
Li D, Pain O, Chiara F, Wong WLE, Lo CWH, Ripke S, et al. Metabolic activity of CYP2C19 and CYP2D6 on antidepressant response from 13 clinical studies using genotype imputation: a meta-analysis. Transl Psychiatry. 2024;14:1–8.
Peters EJ, Slager SL, Kraft JB, Jenkins GD, Reinalda MS, McGrath PJ, et al. Pharmacokinetic genes do not influence response or tolerance to citalopram in the STAR*D sample. PLoS One. 2008;3:e1872.
Maggo S, Kennedy MA, Barczyk ZA, Miller AL, Rucklidge JJ, Mulder RT, et al. Common CYP2D6, CYP2C9, and CYP2C19 Gene Variants, Health Anxiety, and Neuroticism Are Not Associated With Self-Reported Antidepressant Side Effects. Front Genet. 2019;10:1199.
Crisafulli C, Fabbri C, Porcelli S, Drago A, Spina E, De Ronchi D, et al. Pharmacogenetics of antidepressants. Front Pharm. 2011;2:6.
Campos AI, Mulcahy A, Thorp JG, Wray NR, Byrne EM, Lind PA, et al. Understanding genetic risk factors for common side effects of antidepressant medications. Commun Med. 2021;1:1–10.
Choi SW, Mak TSH, O’Reilly PF. A guide to performing Polygenic Risk Score analyses. Nat Protoc. 2020;15:2759–72.
Johnson CF, Maxwell M, Williams B, Dougall N, MacGillivray S. Dose-response effects of selective serotonin reuptake inhibitor monotherapy for the treatment of depression: systematic review of reviews and meta-narrative synthesis. bmjmed [Internet]. Dec [cited 2025 Apr 28];1. Available from: https://bmjmedicine.bmj.com/content/1/1/e000017 (2022).
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29:385–96.
Legge SE, Pardiñas AF, Woolway G, Rees E, Cardno AG, Escott-Price V, et al. Genetic and Phenotypic Features of Schizophrenia in the UK Biobank. JAMA Psychiatry. 2024;81:681–90.
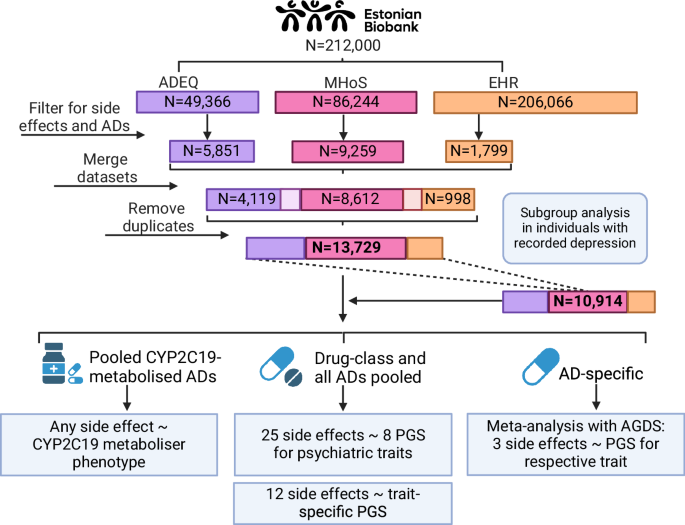
Milani L, Alver M, Laur S, Reisberg S, Haller T, Aasmets O, et al. The Estonian Biobank’s journey from biobanking to personalized medicine. Nat Commun. 2025;16:3270.
Ojalo T, Haan E, Kõiv K, Kariis HM, Krebs K, Uusberg H, et al. Cohort Profile Update: Mental Health Online Survey in the Estonian Biobank (EstBB MHoS). Int J Epidemiol. 2024;53:dyae017.
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc: Ser B (Methodol). 1995;57:289–300.
Byrska-Bishop M, Evani US, Zhao X, Basile AO, Abel HJ, Regier AA, et al. High-coverage whole-genome sequencing of the expanded 1000 Genomes Project cohort including 602 trios. Cell. 2022;185:3426–3440.e19.
Collins RL, Brand H, Karczewski KJ, Zhao X, Alföldi J, Francioli LC, et al. A structural variation reference for medical and population genetics. Nature. 2020;581:444–51.
Golder S, Loke YK, Wright K, Norman G. Reporting of Adverse Events in Published and Unpublished Studies of Health Care Interventions: A Systematic Review. PLOS Med. 2016;13:e1002127.
Bousman CA, Stevenson JM, Ramsey LB, Sangkuhl K, Hicks JK, Strawn JR, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6, CYP2C19, CYP2B6, SLC6A4, and HTR2A Genotypes and Serotonin Reuptake Inhibitor Antidepressants. Clin Pharm Ther. 2023;114:51–68.
Brouwer JMJL, Nijenhuis M, Soree B, Guchelaar HJ, Swen JJ, van Schaik RHN, et al. Dutch Pharmacogenetics Working Group (DPWG) guideline for the gene-drug interaction between CYP2C19 and CYP2D6 and SSRIs. Eur J Hum Genet. 2022;30:1114–20.
Alomar MJ. Factors affecting the development of adverse drug reactions (Review article). Saudi Pharm J. 2014;22:83–94.
Webster RK, Weinman J, Rubin GJ. A systematic review of factors that contribute to nocebo effects. Health Psychol. 2016;35:1334–55.
Zhou Y, Mkrtchian S, Kumondai M, Hiratsuka M, Lauschke VM. An optimized prediction framework to assess the functional impact of pharmacogenetic variants. Pharmacogenomics J. 2019;19:115–26.
Zhou Y, Lauschke VM. Computational Tools to Assess the Functional Consequences of Rare and Noncoding Pharmacogenetic Variability. Clin Pharm Therapeutics. 2021;110:626–36.
Johansson I, Lu Y, Zhou Y, Krebs K, Akcan M, Milani L et al. Proof of principle concept for the analysis and functional prediction of rare genetic variants in the CYP2C19 and CYP2D6 genes. Hum Genomics 2025;19:62.
Adams MJ, Howard DM, Luciano M, Clarke TK, Davies G, Hill WD, et al. Genetic stratification of depression by neuroticism: revisiting a diagnostic tradition. Psychological Med. 2020;50:2526–35.
Romero C, Werme J, Jansen PR, Gelernter J, Stein MB, Levey D, et al. Exploring the genetic overlap between twelve psychiatric disorders. Nat Genet. 2022;54:1795–802.
Tang NKY, Salkovskis PM, Hodges A, Wright KJ, Hanna M, Hester J. Effects of mood on pain responses and pain tolerance: an experimental study in chronic back pain patients. Pain. 2008;138:392–401.
So HC, Sham PC. Exploring the predictive power of polygenic scores derived from genome-wide association studies: a study of 10 complex traits. Bioinformatics. 2017;33:886–92.
Trubetskoy V, Panagiotaropoulou G, Awasthi S, Braun A, Kraft J, Skarabis N, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502.
Alver M, Mancini V, Läll K, Schneider M, Romano L, Mägi R, et al. Contribution of schizophrenia polygenic burden to longitudinal phenotypic variance in 22q11.2 deletion syndrome. Mol Psychiatry. 2022;27:4191–200.
Jones HJ, Stergiakouli E, Tansey KE, Hubbard L, Heron J, Cannon M, et al. Phenotypic Manifestation of Genetic Risk for Schizophrenia During Adolescence in the General Population. JAMA Psychiatry. 2016;73:221–8.
Fanelli G, Benedetti F, Kasper S, Zohar J, Souery D, Montgomery S, et al. Higher polygenic risk scores for schizophrenia may be suggestive of treatment non-response in major depressive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;108(Jun):110170.
Pain O, Hodgson K, Trubetskoy V, Ripke S, Marshe VS, Adams MJ, et al. Identifying the Common Genetic Basis of Antidepressant Response. Biol Psychiatry Glob Open Sci. 2021;2(Aug):115.
Chen B, Choi H, Hirsch LJ, Legge A, Buchsbaum R, Detyniecki K. Cross-sensitivity of psychiatric and behavioral side effects with antiepileptic drug use. Seizure. 2018;62:38–42.
Alonso-Pedrero L, Bes-Rastrollo M, Marti A. Effects of antidepressant and antipsychotic use on weight gain: A systematic review. Obes Rev. 2019;20:1680–90.
Mortensen JK, Andersen G. Safety considerations for prescribing SSRI antidepressants to patients at increased cardiovascular risk. Expert Opinion on Drug Safety [Internet]. Apr [cited 2024 Oct 19]; Available from: https://www.tandfonline.com/doi/abs/10.1080/14740338.2022.1986001 (2022).
Pillinger, Osimo T, Marvao EF, de A, Shah M, Francis C, et al. Effect of polygenic risk for schizophrenia on cardiac structure and function: a UK Biobank observational study. Lancet Psychiatry. 2023;10:98–107.
Rødevand L, Bahrami S, Frei O, Lin A, Gani O, Shadrin A, et al. Polygenic overlap and shared genetic loci between loneliness, severe mental disorders, and cardiovascular disease risk factors suggest shared molecular mechanisms. Transl Psychiatry [Internet]. Jan [cited 2024 Sep 17];11. Available from: https://www.nature.com/articles/s41398-020-01142-4 (2021).
Solmi F, Mascarell MC, Zammit S, Kirkbride JB, Lewis G. Polygenic risk for schizophrenia, disordered eating behaviours and body mass index in adolescents. Br J Psychiatry. 2019;215:428–33.
Meer D van der, Shadrin AA, Stinson SE, Koch E, Rokicki J, Rahman Z, et al. Divergent patterns of genetic overlap between severe mental disorders and metabolic markers [Internet]. medRxiv; [cited 2024 Dec 11]. p. 2024.11.04.24316693. Available from: https://www.medrxiv.org/content/10.1101/2024.11.04.24316693v1 (2024).
Alver M, Kasela S, Haring L, Luitva LB, Fischer K, Möls M, et al. Genetic predisposition and antipsychotic treatment effect on metabolic syndrome in schizophrenia: a ten-year follow-up study using the Estonian Biobank. Lancet Reg Health Eur. 2024;41:100914.
Li D, Lin Y, Davies HL, Zvrskovec JK, Wang R, Armour C, et al. Prediction of antidepressant side effects in the Genetic Link to Anxiety and Depression Study [Internet]. medRxiv; [cited 2024 Jun 10]. p. 2024.05.01.24306668. Available from: https://www.medrxiv.org/content/10.1101/2024.05.01.24306668v1 (2024).
Corfitsen HT, Drago A. Insight gained from genome-wide interaction and enrichment analysis on weight gain during citalopram treatment. Neurosci Lett. 2017;637:38–43.
Eesti Haigekassa. Migreeni esmane diagnostika ja farmakoteraapia täiskasvanutel [Internet]. Tallinn, Estonia; [cited 2024 Nov 12]. Report No.: Ravijuhend. RJ-E/xx-2022. Available from: https://www.ravijuhend.ee/tervishoiuvarav/juhendid-gp/22/Migreeni%20esmane%20diagnostika%20ja%20farmakoteraapia%20t%C3%A4iskasvanutel (2022).
Ruderfer DM, Charney AW, Readhead B, Kidd BA, Kähler AK, Kenny PJ, et al. Polygenic overlap between schizophrenia risk and antipsychotic response: a genomic medicine approach. Lancet Psychiatry. 2016;3:350–7.