Monteiro, C. A. et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 22, 936–941 (2019).
Lane, M. M. et al. Ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses. Br. Med. J. https://doi.org/10.1136/bmj-2023-077310 (2024).
Mendoza, K. et al. Ultra-processed foods and cardiovascular disease: analysis of three large US prospective cohorts and a systematic review and meta-analysis of prospective cohort studies. Lancet Reg. Health Am. 37, 100859 (2024).
Srour, B. et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). Br. Med. J. https://doi.org/10.1136/bmj.l1451 (2019).
Brauer, M. et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203 (2024).
Deveci, G. & Tek, N. A. N-Nitrosamines: a potential hazard in processed meat products. J. Sci. Food Agric. 104, 2551–2560 (2024).
Lee, J.-G. et al. Effects of grilling procedures on levels of polycyclic aromatic hydrocarbons in grilled meats. Food Chem. 199, 632–638 (2016).
Zheng, W. & Lee, S.-A. Well-done meat intake, heterocyclic amine exposure, and cancer risk. Nutr. Cancer 61, 437–446 (2009).
López-Hernández, L. et al. Identifying predictors of the visceral fat index in the obese and overweight population to manage obesity: a randomized intervention study. Obes. Facts 13, 403–414 (2020).
Huang, Y. et al. Associations of visceral adipose tissue, circulating protein biomarkers, and risk of cardiovascular diseases: a Mendelian randomization analysis. Front. Cell Dev. Biol. 10, 840866 (2022).
Marques, M. D. et al. Relation between visceral fat and coronary artery disease evaluated by multidetector computed tomography. Atherosclerosis 209, 481–486 (2010).
Oostindjer, M. et al. The role of red and processed meat in colorectal cancer development: a perspective. Meat Sci. 97, 583–596 (2014).
Bellamri, M., Walmsley, S. J. & Turesky, R. J. Metabolism and biomarkers of heterocyclic aromatic amines in humans. Genes Environ. 43, 29 (2021).
Lala, P. K. & Chakraborty, C. Role of nitric oxide in carcinogenesis and tumour progression. Lancet Oncol. 2, 149–156 (2001).
Moorthy, B., Chu, C. & Carlin, D. J. Polycyclic aromatic hydrocarbons: from metabolism to lung cancer. Toxicol. Sci. 145, 5–15 (2015).
Rao, C. V. Nitric oxide signaling in colon cancer chemoprevention. Mutat. Res. 555, 107–119 (2004).
Sánchez-Pimienta, T. G., Batis, C., Lutter, C. K. & Rivera, J. A. Sugar-sweetened beverages are the main sources of added sugar intake in the Mexican population. J. Nutr. 146, 1888S–1896S (2016).
Vartanian, L. R., Schwartz, M. B. & Brownell, K. D. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am. J. Public Health 97, 667–675 (2007).
Lara-Castor, L. et al. Sugar-sweetened beverage intakes among adults between 1990 and 2018 in 185 countries. Nat. Commun. 14, 5957 (2023).
Stender, S., Astrup, A. & Dyerberg, J. Ruminant and industrially produced trans fatty acids: health aspects. Food Nutr. Res. 52, 1651 (2008).
Mozaffarian, D. et al. Dietary intake of trans fatty acids and systemic inflammation in women. Am. J. Clin. Nutr. 79, 606–612 (2004).
Bendsen, N. T., Christensen, R., Bartels, E. M. & Astrup, A. Consumption of industrial and ruminant trans fatty acids and risk of coronary heart disease: a systematic review and meta-analysis of cohort studies. Eur. J. Clin. Nutr. 65, 773–783 (2011).
Mozaffarian, D., Katan, M. B., Ascherio, A., Stampfer, M. J. & Willett, W. C. Trans fatty acids and cardiovascular disease. N. Engl. J. Med. 354, 1601–1613 (2006).
Naghavi, M. et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
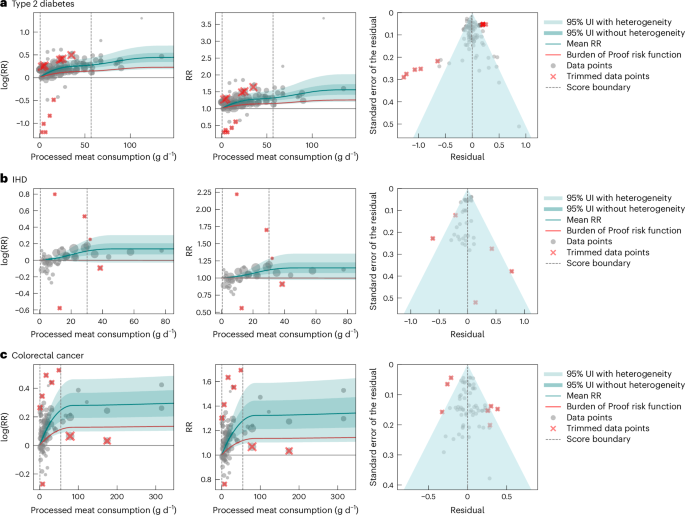
Zheng, P. et al. The Burden of Proof studies: assessing the evidence of risk. Nat. Med. 28, 2038–2044 (2022).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. https://doi.org/10.1136/bmj.n71 (2021).
Ericson, U. et al. Food sources of fat may clarify the inconsistent role of dietary fat intake for incidence of type 2 diabetes. Am. J. Clin. Nutr. 101, 1065–1080 (2015).
Fretts, A. M. et al. Associations of processed meat and unprocessed red meat intake with incident diabetes: the Strong Heart Family Study. Am. J. Clin. Nutr. 95, 752–758 (2012).
Gu, X. et al. Red meat intake and risk of type 2 diabetes in a prospective cohort study of United States females and males. Am. J. Clin. Nutr. 118, 1153–1163 (2023).
Kurotani, K. et al. Red meat consumption is associated with the risk of type 2 diabetes in men but not in women: a Japan Public Health Center-based Prospective Study. Br. J. Nutr. 110, 1910–1918 (2013).
Lajous, M. et al. Processed and unprocessed red meat consumption and incident type 2 diabetes among French women. Diabetes Care 35, 128–130 (2012).
Liu, M. et al. Quantity and variety of food groups consumption and the risk of diabetes in adults: a prospective cohort study. Clin. Nutr. 40, 5710–5717 (2021).
Männistö, S., Kontto, J., Kataja-Tuomola, M., Albanes, D. & Virtamo, J. High processed meat consumption is a risk factor of type 2 diabetes in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention study. Br. J. Nutr. 103, 1817–1822 (2010).
Mari-Sanchis, A. et al. Meat consumption and risk of developing type 2 diabetes in the SUN project: a highly educated middle-class population. PLoS ONE 11, e0157990 (2016).
Montonen, J. et al. Food consumption and the incidence of type II diabetes mellitus. Eur. J. Clin. Nutr. 59, 441–448 (2005).
Papier, K. et al. Meat consumption and risk of 25 common conditions: outcome-wide analyses in 475,000 men and women in the UK Biobank study. BMC Med. 19, 53 (2021).
Son, J., Lee, Y. & Park, K. Effects of processed red meat consumption on the risk of type 2 diabetes and cardiovascular diseases among Korean adults: the Korean Genome and Epidemiology Study. Eur. J. Nutr. 58, 2477–2484 (2019).
Song, Y., Manson, J. E., Buring, J. E. & Liu, S. A prospective study of red meat consumption and type 2 diabetes in middle-aged and elderly women. Diabetes Care 27, 2108–2115 (2004).
Steinbrecher, A., Erber, E., Grandinetti, A., Kolonel, L. & Maskarinec, G. Meat consumption and risk of type 2 diabetes: the Multiethnic Cohort. Public Health Nutr. 14, 568–574 (2011).
Van Woudenbergh, G. J. et al. Meat consumption and its association with C-reactive protein and incident type 2 diabetes. Diabetes Care 35, 1499–1505 (2012).
Villegas, R. et al. The association of meat intake and the risk of type 2 diabetes may be modified by body weight. Int. J. Med. Sci. https://doi.org/10.7150/ijms.3.152 (2006).
The InterAct Consortium. Association between dietary meat consumption and incident type 2 diabetes: the EPIC-InterAct study. Diabetologia 56, 47–59 (2013).
Al-Shaar, L. et al. Red meat intake and risk of coronary heart disease among US men: prospective cohort study. BMJ https://doi.org/10.1136/bmj.m4141 (2020).
Bernstein, A. M. et al. Major dietary protein sources and risk of coronary heart disease in women. Circulation 122, 876–883 (2010).
Burke, V. et al. Health-related behaviours as predictors of mortality and morbidity in Australian Aborigines. Prev. Med. 44, 135–142 (2007).
Haring, B. et al. Dietary protein intake and coronary heart disease in a large community based cohort: results from the Atherosclerosis Risk in Communities (ARIC) study. PLoS ONE 9, e109552 (2014).
Iqbal, R. et al. Associations of unprocessed and processed meat intake with mortality and cardiovascular disease in 21 countries [Prospective Urban Rural Epidemiology (PURE) Study]: a prospective cohort study. Am. J. Clin. Nutr. 114, 1049–1058 (2021).
Key, T. J. et al. Consumption of meat, fish, dairy products, and eggs and risk of ischemic heart disease: a prospective study of 7198 incident cases among 409 885 participants in the Pan-European EPIC Cohort. Circulation 139, 2835–2845 (2019).
Møller, S. P., Mejborn, H., Christensen, A. I., Biltoft-Jensen, A. & Thygesen, L. C. Meat consumption, stratified by dietary quality, and risk of heart disease. Br. J. Nutr. 126, 1881–1887 (2021).
Nagao, M. et al. Meat consumption in relation to mortality from cardiovascular disease among Japanese men and women. Eur. J. Clin. Nutr. 66, 687–693 (2012).
Saito, E. et al. Association between meat intake and mortality due to all-cause and major causes of death in a Japanese population. PLoS ONE 15, e0244007 (2020).
Whiteman, D., Muir, J., Jones, L., Murphy, M. & Key, T. Dietary questions as determinants of mortality: the OXCHECK experience. Public Health Nutr. 2, 477–487 (1999).
Bernstein, A. M. et al. Processed and unprocessed red meat and risk of colorectal cancer: analysis by tumor location and modification by time. PLoS ONE 10, e0135959 (2015).
Bostick, R. M. et al. Sugar, meat, and fat intake, and non-dietary risk factors for colon cancer incidence in Iowa women (United States). Cancer Causes Control 5, 38–52 (1994).
Chao, A. Meat consumption and risk of colorectal cancer. JAMA 293, 172 (2005).
Cross, A. J. et al. A large prospective study of meat consumption and colorectal cancer risk: an investigation of potential mechanisms underlying this association. Cancer Res. 70, 2406–2414 (2010).
English, D. R. et al. Red meat, chicken, and fish consumption and risk of colorectal cancer. Cancer Epidemiol. Biomarkers Prev. 13, 1509–1514 (2004).
Etemadi, A. et al. Anatomical subsite can modify the association between meat and meat compounds and risk of colorectal adenocarcinoma: findings from three large US cohorts. Int. J. Cancer 143, 2261–2270 (2018).
Flood, A. Meat, fat, and their subtypes as risk factors for colorectal cancer in a prospective cohort of women. Am. J. Epidemiol. 158, 59–68 (2003).
Gilsing, A. M. J. et al. Vegetarianism, low meat consumption and the risk of colorectal cancer in a population based cohort study. Sci. Rep. 5, 13484 (2015).
Islam, Z. et al. Meat subtypes and colorectal cancer risk: a pooled analysis of 6 cohort studies in Japan. Cancer Sci. 110, 3603–3614 (2019).
Knuppel, A. et al. Meat intake and cancer risk: prospective analyses in UK Biobank. Int. J. Epidemiol. 49, 1540–1552 (2020).
Larsson, S. C., Rafter, J., Holmberg, L., Bergkvist, L. & Wolk, A. Red meat consumption and risk of cancers of the proximal colon, distal colon and rectum: the Swedish Mammography Cohort. Int. J. Cancer 113, 829–834 (2005).
Lin, J. Dietary fat and fatty acids and risk of colorectal cancer in women. Am. J. Epidemiol. 160, 1011–1022 (2004).
Mehta, S. S. et al. A prospective analysis of red and processed meat consumption and risk of colorectal cancer in women. Cancer Epidemiol. Biomarkers Prev. 29, 141–150 (2020).
Mejborn, H., Møller, S. P., Thygesen, L. C. & Biltoft-Jensen, A. Dietary intake of red meat, processed meat, and poultry and risk of colorectal cancer and all-cause mortality in the context of dietary guideline compliance. Nutrients 13, 32 (2020).
Norat, T. et al. Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J. Natl Cancer Inst. 97, 906–916 (2005).
Ollberding, N. J., Wilkens, L. R., Henderson, B. E., Kolonel, L. N. & Le Marchand, L. Meat consumption, heterocyclic amines and colorectal cancer risk: the Multiethnic Cohort Study. Int. J. Cancer 131, E1125–E1133 (2012).
O’Sullivan, D. E. et al. Combinations of modifiable lifestyle behaviours in relation to colorectal cancer risk in Alberta’s Tomorrow Project. Sci. Rep. 10, 20561 (2020).
Pietinen, P. et al. Diet and risk of colorectal cancer in a cohort of Finnish men. Cancer Causes Control 10, 387–396 (1999).
Bhupathiraju, S. N. et al. Caffeinated and caffeine-free beverages and risk of type 2 diabetes. Am. J. Clin. Nutr. 97, 155–166 (2013).
Dhingra, R. et al. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 116, 480–488 (2007).
Eshak, E. S. et al. Soft drink, 100% fruit juice, and vegetable juice intakes and risk of diabetes mellitus. Clin. Nutr. 32, 300–308 (2013).
Fagherazzi, G. et al. Consumption of artificially and sugar-sweetened beverages and incident type 2 diabetes in the Etude Epidemiologique aupres des femmes de la Mutuelle Generale de l’Education Nationale-European Prospective Investigation into Cancer and Nutrition cohort. Am. J. Clin. Nutr. 97, 517–523 (2013).
Gardener, H., Moon, Y. P., Rundek, T., Elkind, M. S. V. & Sacco, R. L. Diet soda and sugar-sweetened soda consumption in relation to incident diabetes in the Northern Manhattan Study. Curr. Dev. Nutr. 2, nzy008 (2018).
Hirahatake, K. M. et al. Cumulative intake of artificially sweetened and sugar-sweetened beverages and risk of incident type 2 diabetes in young adults: the Coronary Artery Risk Development In Young Adults (CARDIA) Study. Am. J. Clin. Nutr. 110, 733–741 (2019).
Huang, M. et al. Artificially sweetened beverages, sugar-sweetened beverages, plain water, and incident diabetes mellitus in postmenopausal women: the prospective Women’s Health Initiative observational study. Am. J. Clin. Nutr. 106, 614–622 (2017).
Montonen, J., Järvinen, R., Knekt, P., Heliövaara, M. & Reunanen, A. Consumption of sweetened beverages and intakes of fructose and glucose predict type 2 diabetes occurrence. J. Nutr. 137, 1447–1454 (2007).
O’Connor, L. et al. Prospective associations and population impact of sweet beverage intake and type 2 diabetes, and effects of substitutions with alternative beverages. Diabetologia 58, 1474–1483 (2015).
Odegaard, A. O., Koh, W.-P., Arakawa, K., Yu, M. C. & Pereira, M. A. Soft drink and juice consumption and risk of physician-diagnosed incident type 2 diabetes: the Singapore Chinese Health Study. Am. J. Epidemiol. 171, 701–708 (2010).
Palmer, J. R. et al. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch. Intern. Med. 168, 1487–1492 (2008).
Pan, A. et al. Plain-water intake and risk of type 2 diabetes in young and middle-aged women. Am. J. Clin. Nutr. 95, 1454–1460 (2012).
Papier, K. et al. Consumption of sugar-sweetened beverages and type 2 diabetes incidence in Thai adults: results from an 8-year prospective study. Nutr. Diabetes 7, e283 (2017).
Paynter, N. P. et al. Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the Atherosclerosis Risk in Communities Study. Am. J. Epidemiol. 164, 1075–1084 (2006).
Sakurai, M. et al. Sugar-sweetened beverage and diet soda consumption and the 7-year risk for type 2 diabetes mellitus in middle-aged Japanese men. Eur. J. Nutr. 53, 251–258 (2014).
Siqueira, J. H. et al. Consumption of sugar-sweetened soft drinks and risk of metabolic syndrome and its components: results of the ELSA-Brasil study (2008–2010 and 2012–2014). J. Endocrinol. Invest. 46, 159–171 (2022).
Torres-Ibarra, L. et al. Regular consumption of soft drinks is associated with type 2 diabetes incidence in Mexican adults: findings from a prospective cohort study. Nutr. J. 19, 126 (2020).
Viana Dias, J. P. et al. Consumption of sweetened beverages is associated with the incidence of type 2 diabetes in Brazilian adults (CUME project). Nutr. Metab. Cardiovasc. Dis. 33, 789–796 (2023).
The InterAct consortium. Consumption of sweet beverages and type 2 diabetes incidence in European adults: results from EPIC-InterAct. Diabetologia 56, 1520–1530 (2013).
Eshak, E. S. et al. Soft drink intake in relation to incident ischemic heart disease, stroke, and stroke subtypes in Japanese men and women: the Japan Public Health Centre-based study cohort I. Am. J. Clin. Nutr. 96, 1390–1397 (2012).
Warfa, K., Drake, I., Wallström, P., Engström, G. & Sonestedt, E. Association between sucrose intake and acute coronary event risk and effect modification by lifestyle factors: Malmö Diet and Cancer Cohort Study. Br. J. Nutr. 116, 1611–1620 (2016).
Pacheco, L. S. et al. Sugar-sweetened beverage intake and cardiovascular disease risk in the California Teachers Study. J. Am. Heart Assoc. 9, e014883 (2020).
Collin, L. J., Judd, S., Safford, M., Vaccarino, V. & Welsh, J. A. Association of sugary beverage consumption with mortality risk in US adults: a secondary analysis of data from the REGARDS Study. JAMA Netw. Open 2, e193121 (2019).
Yang, B. et al. Added sugar, sugar-sweetened beverages, and artificially sweetened beverages and risk of cardiovascular disease: findings from the Women’s Health Initiative and a network meta-analysis of prospective studies. Nutrients 14, 4226 (2022).
Mullee, A. et al. Association between soft drink consumption and mortality in 10 European countries. JAMA Intern. Med. 179, 1479–1490 (2019).
Keller, A. et al. Substitution of sugar-sweetened beverages for other beverages and the risk of developing coronary heart disease: results from the Harvard Pooling Project of Diet and Coronary Disease. Prev. Med. 131, 105970 (2020).
Pacheco, L. S. et al. Sugar- or artificially-sweetened beverage consumption, physical activity, and risk of cardiovascular disease in US adults. Preprint at medRxiv https://doi.org/10.1101/2023.04.17.23288711 (2023).
Laake, I. et al. A prospective study of intake of trans-fatty acids from ruminant fat, partially hydrogenated vegetable oils, and marine oils and mortality from CVD. Br. J. Nutr. 108, 743–754 (2012).
Li, Y. et al. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease. J. Am. Coll. Cardiol. 66, 1538–1548 (2015).
Oomen, C. M. et al. Association between trans fatty acid intake and 10-year risk of coronary heart disease in the Zutphen Elderly Study: a prospective population-based study. Lancet 357, 746–751 (2001).
Pietinen, P. et al. Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men. the Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Am. J. Epidemiol. 145, 876–887 (1997).
Virtanen, J. K., Mursu, J., Tuomainen, T.-P. & Voutilainen, S. Dietary fatty acids and risk of coronary heart disease in men: the Kuopio Ischemic Heart Disease Risk Factor Study. Arterioscler. Thromb. Vasc. Biol. 34, 2679–2687 (2014).
Xu, J. et al. Dietary fat intake and risk of coronary heart disease: the Strong Heart Study. Am. J. Clin. Nutr. 84, 894–902 (2006).
Bouvard, V. et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 16, 1599–1600 (2015).
Stern, M. C. et al. Genome-wide gene–environment interaction analyses to understand the relationship between red meat and processed meat intake and colorectal cancer risk. Cancer Epidemiol. Biomarkers Prev. 33, 400–410 (2024).
WHO Manual on Sugar-Sweetened Beverage Taxation Policies to Promote Healthy Diets (World Health Organization, 2022).
Andreyeva, T., Marple, K., Marinello, S., Moore, T. E. & Powell, L. M. Outcomes following taxation of sugar-sweetened beverages: a systematic review and meta-analysis. JAMA Netw. Open 5, e2215276 (2022).
World Health Organization Guideline: Sugars intake for adults and children (WHO Department of Nutrition for Health and Development (NHD), 2015).
Dietary Guidelines for Americans, 2020–2025 9th edn (US Department of Agriculture and US Department of Health and Human Services, 2020).
Countdown to 2023: WHO 5-Year Milestone Report on Global Trans Fat Elimination 2023 (World Health Organization, 2024).
Freedman, L. S., Schatzkin, A., Midthune, D. & Kipnis, V. Dealing with dietary measurement error in nutritional cohort studies. J. Natl Cancer Inst. 103, 1086–1092 (2011).
Kipnis, V. et al. Effect of measurement error on energy-adjustment models in nutritional epidemiology. Am. J. Epidemiol. 146, 842–855 (1997).
Dahm, C. C. Correcting measurement error in dietary exposure assessments: no piece of cake. Am. J. Clin. Nutr. 112, 11–12 (2020).
McCullough, L. E. & Byrd, D. A. Total energy intake: implications for epidemiologic analyses. Am. J. Epidemiol. 192, 1801–1805 (2023).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S–1228S (1997).
Day, N. E. et al. Correlated measurement error—implications for nutritional epidemiology. Int. J. Epidemiol. 33, 1373–1381 (2004).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
Kassem, H. et al. Investigation and assessment of AI’s role in nutrition—an updated narrative review of the evidence. Nutrients 17, 190 (2025).
Zheng, J., Wang, J., Shen, J. & An, R. Artificial intelligence applications to measure food and nutrient intakes: scoping review. J. Med. Internet Res. 26, e54557 (2024).
Lo, F. P.-W. et al. AI-enabled wearable cameras for assisting dietary assessment in African populations. npj Digit. Med. 7, 356 (2024).
Burgess, S., Foley, C. N., Allara, E., Staley, J. R. & Howson, J. M. M. A robust and efficient method for Mendelian randomization with hundreds of genetic variants. Nat. Commun. 11, 376 (2020).
Lai, W., Li, G., Peng, D., Li, N. & Wang, W. Mendelian randomization study reveals the relationship between dietary factors and respiratory diseases. Sci. Rep. 13, 22601 (2023).
Lescinsky, H. et al. Health effects associated with consumption of unprocessed red meat: a Burden of Proof study. Nat. Med. 28, 2075–2082 (2022).
Stanaway, J. D. et al. Health effects associated with vegetable consumption: a Burden of Proof study. Nat. Med. 28, 2066–2074 (2022).
Stevens, G. A. et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet 388, e19–e23 (2016).
Pan, A. et al. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch. Intern. Med. 172, 555–563 (2012).
de Souza, R. J. et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. Br. Med. J. 351, h3978 (2015).
Zhang, Y.-B., Jiang, Y.-W., Chen, J.-X., Xia, P.-F. & Pan, A. Association of consumption of sugar-sweetened beverages or artificially sweetened beverages with mortality: a systematic review and dose–response meta-analysis of prospective cohort studies. Adv. Nutr. 12, 374–383 (2021).
Zheng, P., Barber, R., Sorensen, R. J. D., Murray, C. J. L. & Aravkin, A. Y. Trimmed constrained mixed effects models: formulations and algorithms. J. Comput. Graph. Stat. 30, 544–556 (2021).