In late September, Laurel Vincenty got a letter from Blue Cross Blue Shield informing her that the subsidies that covered a big chunk of her health insurance would be expiring at the end of the year, sending her monthly premiums soaring.
Vincenty, 64, and her husband Philip Vincenty, 62, of North Carolina, are covered through the Affordable Care Act. They currently pay about $400 each month in premiums. An additional $1,700 is covered through the soon-expiring subsidies.
Both Vincenty and her husband are self-employed. In 2020, she was diagnosed with breast cancer, and in 2024, Philip had a heart attack — health issues that left them with thousands of dollars in medical debt they’re still paying off. Their monthly medications cost hundreds of dollars.
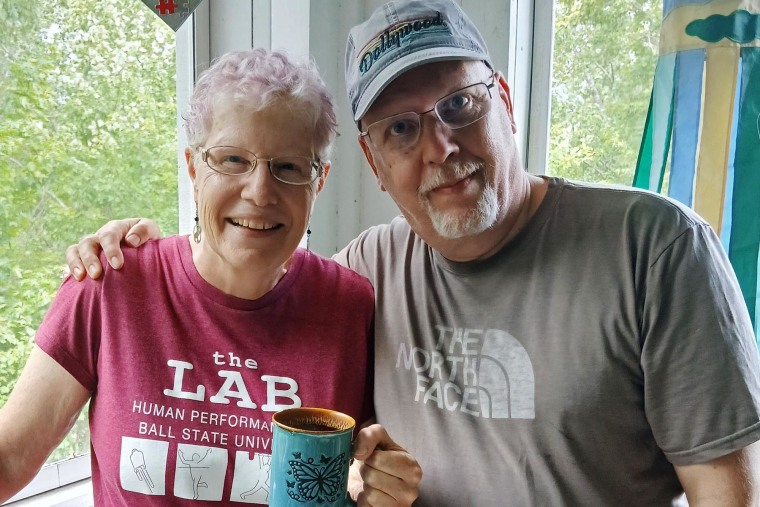 Laurel and Philip Vincenty.Courtesy Laurel Vincenty
Laurel and Philip Vincenty.Courtesy Laurel Vincenty
Vincenty picked up a second job this month in anticipation of their premiums going up next year, but she said she doesn’t know if it’ll be enough.
“It was frustrating receiving the letter,” she said, “knowing that we may lose our subsidies, that we don’t know how we’ll be able to afford our health insurance.”
The enhanced ACA subsidies the Vincentys are set to lose are a key sticking point in the ongoing government shutdown: Democrats in Congress say that in order to secure their votes to reopen the government, the subsidies — first included under the 2021 American Rescue Plan and later extended through 2025 in the 2022 Inflation Reduction Act — must be extended.
Open enrollment for ACA plans begins Nov. 1 in most states, and people already enrolled in plans are starting to get notices about next year’s rates. According to an analysis from the health policy research group KFF, without the subsidies, average out-of-pocket premium payments are expected to double, from $888 a year to $1,904.
 Laurel Vincenty before her breast cancer surgery on New Year’s Eve in 2020.Courtesy Laurel Vincenty
Laurel Vincenty before her breast cancer surgery on New Year’s Eve in 2020.Courtesy Laurel Vincenty
Lawrence Gostin, director of the O’Neill Institute for National and Global Health Law at Georgetown University, said the damage is already starting.
“Even if a deal is done to extend the subsidies, many enrollees will drop out due to the sticker shock,” he said.
‘Unpleasant news’
Insurers are required to send ACA enrollees renewal notices no later than the first day of open enrollment, according to Adrianna McIntyre, an assistant professor at the department of health policy and management at the Harvard T.H. Chan School of Public Health.
The notices typically include information about the next year’s coverage and premiums, though some provide more specifics than others.
“That means we should expect a lot of marketplace enrollees to be receiving unpleasant news about their premiums in mid- and late-October,” McIntyre said.
People may have the option to switch to a plan with lower premiums — going from a silver-tier plan to a bronze-tier plan, for example — but those switches often come with a large increase in deductibles, she said.
Navigators who help people enroll in ACA plans might have been well-situated to help people work through their options, McIntyre added, but earlier this year the Trump administration cut their funding by 90% in states that use the federal HealthCare.gov platform, the online marketplace for ACA plans.
More than 24 million people are enrolled in ACA plans this year, and about 9 out of 10 — 22.3 million people — get enhanced subsidies, according to KFF. If the subsidies expire, almost 4 million people are expected to drop their coverage for 2026, according to an analysis from the Congressional Budget Office.
Jeff Feldman, a 60-year-old musician in Phoenix, is considering dropping his coverage next year.
He got a letter Monday from HealthCare.gov that stated: “The extra financial help that was available because of the COVID pandemic ends on December 31, 2025.”
“Our records show you qualified for financial help in 2025,” the letter read. “If you qualify for financial help in 2026, you’ll likely pay more for your Marketplace plan premium.”
Feldman estimates his monthly premiums will triple — from $300 to $900, while his $9,000 yearly deductible will likely go unchanged.
“They just priced me right out of the market,” he said. “I have two jobs, and I’m going to start driving for Uber and Lyft just to get some extra money. And even with that, I can’t afford $900 a month.”
Instead, he said, he plans to go uninsured next year and put the money that would have gone toward his premium into a savings account for medical emergencies.
For others, the premium increases aren’t as steep but will still have an impact.
Wesley Hartman, of Chatsworth, California, said he and his wife got a letter dated Sept. 17 from Covered California — the state’s ACA marketplace — saying that without the tax credits, their monthly premium will rise from $1,212 to $1,450.
While they can afford the increase, he said, the extra cost will come at a sacrifice to his startup information technology business, which he launched a few years ago.
“I won’t be able to do things like expand my business more, or potentially hire or purchase software that can help me continue to grow my business,” Hartman said.
He described feeling a mix of frustration and resignation the day he got the letter.
“The saying is that America is run by small businesses, right?” Hartman said. “So we’re one of them and just trying to build that. It really feels like there’s nothing I can do about it.”
