NEED TO KNOW
-
A father of two died from sepsis after not being given the right medication for 34 hours, a new investigation has found
-
The man, who had disabilities, had been referred to Bassetlaw Hospital in Worksop, England, by a primary care physician after contracting a urinary infection.
-
“The Parliamentary and Health Service Ombudsman (PHSO) found that his death was avoidable,” a release from the organization noted. “The man lived in supported accommodation in Ollerton, Nottinghamshire, and had a rare, incurable disorder called Alexander’s Disease, which affects the nervous system”
A father of two died from sepsis after not being given the right medication for 34 hours, a new investigation has found.
On Wednesday, Dec. 10, the Parliamentary and Health Service Ombudsman (PHSO) revealed in a statement that a 45-year-old man could have survived if he had received antibiotics earlier at Bassetlaw Hospital in Worksop, England, in November 2022.
The man, who had disabilities, had been referred to the hospital by a primary care physician after contracting a urinary infection.
Despite being prescribed intravenous (IV) antibiotics, he ended up waiting 34 hours for the medication while at the hospital.
“The Parliamentary and Health Service Ombudsman (PHSO) found that his death was avoidable,” the release read. “The man lived in supported accommodation in Ollerton, Nottinghamshire, and had a rare, incurable disorder called Alexander’s Disease, which affects the nervous system.”
PEOPLE reached out to the Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust and the Bassetlaw Hospital for comment, but they did not immediately respond.

Never miss a story — sign up for PEOPLE’s free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from juicy celebrity news to compelling human interest stories.
“He had respiratory and mobility issues and needed 24-hour care and help with feeding and personal hygiene,” PHSO continued. “Due to his condition, the man had a permanent catheter and was susceptible to Urinary Tract Infections (UTI).”
The man struggled with communicating his needs with medical staff due to his disabilities. While his mother expressed her concerns with the staff at the hospital, she did not realize he had not yet been given the antibiotics prescribed to him.
The hospital was also told by the paramedics and care home staff that the Nottinghamshire resident needed IV antibiotics.
Though the primary care physician had entered the man’s test results into an online system, the hospital did not use it, due to the request not being in writing.

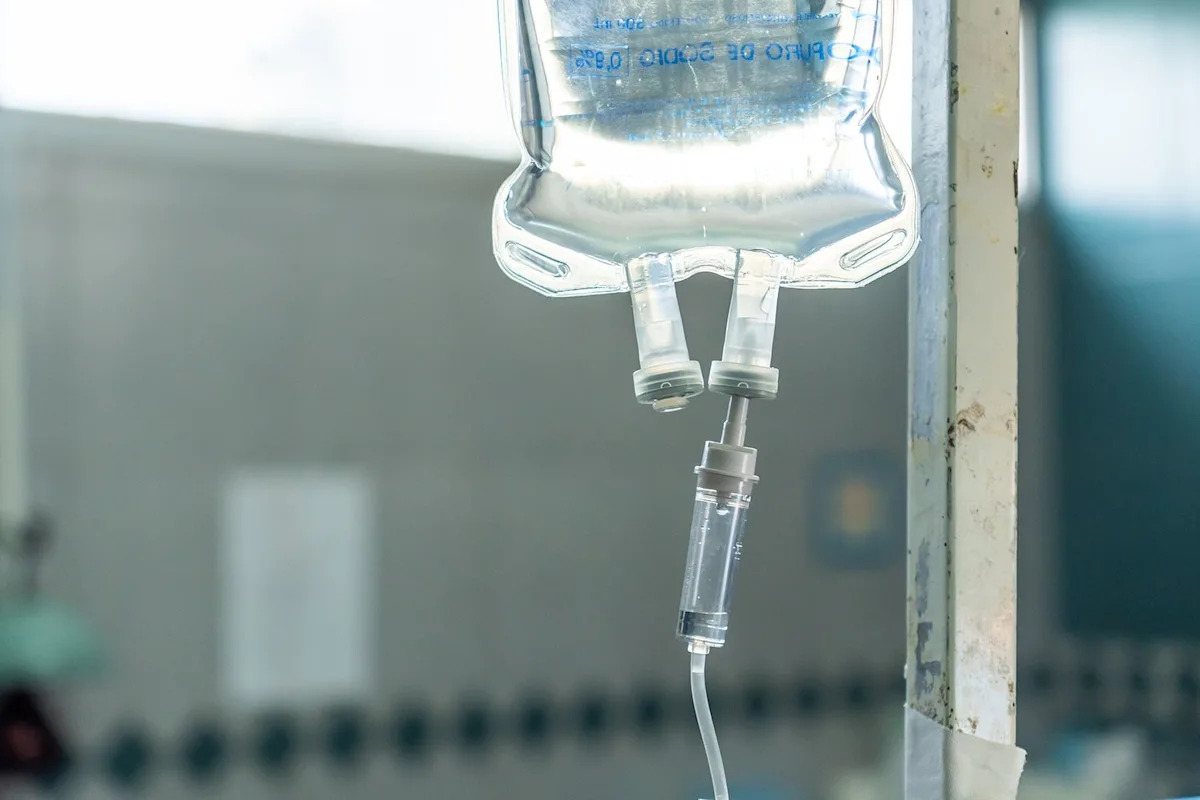
Getty
Stock image of hospital waiting room
“Instead, following consultation with a microbiologist, staff decided to try an oral antibiotic, but the requested drug was unavailable,” the release read. “At that point, the Ombudsman found that doctors should have requested further advice, and it is likely that IV antibiotics would have been advised and available.”
The IV antibiotic ended up being given to the man “34 hours after he arrived at [the] hospital, and at half the dosage it should have been,” according to the release.
There was also a three-hour delay from when the doctors asked for the medication to when it was given to the patient.
He had then become septic by the time the second dose was given, before passing away a week later.
“In this case, a man who was unable to advocate [for] himself and completely reliant on clinicians to look after him did not receive the care he needed. Tragically, this meant he unnecessarily lost his life,” Rebecca Hilsenrath KC (Hon), Chief Executive Officer of PHSO, said in a statement.
“Losing a life through sepsis should not be an inevitability,” she added. “But we are seeing the same failings repeated time and time again, and complaints about sepsis have more than doubled over the past five years. We also see poor communication between patients and clinicians and we are focusing our efforts to help improve this throughout the NHS.”
“Organizations must be held to account so that justice can be provided, and services can be improved for the future,” Hilsenrath continued. “The NHS needs to have a culture that is open, listens to patients and their families, accepts mistakes when they happen and learns from them.”
The man’s mother also said, “I knew my son better than anyone, and I was trying to help the doctors by telling them the oral antibiotic wouldn’t work and that the GP had a microbiologist’s report that said he wouldn’t respond to that drug.”
“But they just totally dismissed me. Their attitude was they were the doctors, and I was just his mum,” she added.
“It was heartbreaking to finally understand the truth,” the mother continued. “I was given the impression he had at least been given some antibiotics, even if they weren’t the right ones. But to find out he was in hospital for all that time with no treatment was very hard.”
In a statement to PEOPLE, the Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust said they were “truly sorry for what happened in this case and for the loss experienced by the patient’s family.”
“We reviewed the information and care provided at the time through our Patient Safety Panel,” the statement continued. “Immediate actions were implemented to strengthen how antibiotics were prescribed, escalated and given.”
Read the original article on People