The fertility market in the U.S. is exploding as venture capital and private equity pour money into clinics treating infertility through assisted reproductive technologies like IVF. But these procedures remain prohibitively expensive for many, and more doctors, laboratory specialists and other practitioners are needed to support the growing field.
One fertility training program in San Antonio is aiming to fill that gap.
IVF Academy USA, launched in 2024 and located off Loop 1604 on the North Side, is an accredited training school teaching doctors, nurse practitioners and physician assistants how to perform and assist in egg retrievals and transfers during in vitro fertilization procedures.
The for-profit program also has a laboratory school for aspiring embryologists, responsible for managing sperm and egg cells.
The school, which offers six and 12-month courses for clinicians, graduated its first cohort of seven doctors and nurse practitioners on Dec. 5.
According to Dr. Paul Magarelli, a reproductive endocrinologist and infertility specialist who was recently appointed as dean of the program’s clinical arm, the training program is turning San Antonio into the epicenter of the growing fertility market.
“There’s no place in the world that has a business school, a lab school and a clinical school specifically focused on access to care by providing trained people in the IVF industry,” Magarelli said.
Growing fertility market
In vitro fertilization is by far the most common procedure of the growing list of assisted reproductive technologies that treat infertility, accounting for 99% of such procedures.
In 2023, nearly 100,000 babies were born in the U.S. with the help of IVF, accounting for 2.6% of births, according to the Society for Assisted Reproductive Technology. The technology was developed in the ’70s, and the first IVF baby was born in 1978.
 Katie Balloch, director of embryological training and education at IVF Academy USA, reviews a video feed from an embryoscope of embryo development from fertilization to the blastocyst stage over five days. Credit: Amber Esparza / San Antonio Report
Katie Balloch, director of embryological training and education at IVF Academy USA, reviews a video feed from an embryoscope of embryo development from fertilization to the blastocyst stage over five days. Credit: Amber Esparza / San Antonio Report
One cycle of IVF involves a number of steps generally performed over the course of two weeks. First, the patient takes fertility medications that increase the number of eggs produced by their ovaries. The eggs are then retrieved and fertilized with sperm in a lab.
If successfully fertilized, the eggs divide and become embryos, which are then placed back inside the ovaries. Pregnancy rates from IVF vary depending on a number of factors, of which age is the most significant. Between 45% and 55% of women under 35 achieve pregnancy through IVF, but many of them will require several cycles.
Even one cycle, though, is financially out of reach for many people experiencing infertility challenges. Including the cost of required medications, one cycle of IVF in Texas can cost anywhere from $16,000 to $30,000, according to CYN Fertility. Fertility medications and procedures are typically not covered by health insurance, making it inaccessible to many in the U.S., according to KFF, a nonprofit health policy group.
A history of infertility, defined as the inability to conceive after one year of trying, is typically necessary to receive IVF treatment, although the procedure is also less commonly used to avoid passing on genetic defects.
President Donald Trump, who earlier this year said he’d be known as “the fertilization president,” has promised to bring down the costs of IVF, a contentious topic among some of his conservative and religious supporters.
The $9 billion U.S. fertility market is estimated to grow to nearly $20 billion by 2034.
Behind the curve
IVF procedures are performed by reproductive endocrinologists, OB-GYNs who have completed an advanced fertility fellowship. Embryologists, responsible for managing sperm and egg cells in the lab to create a viable embryo, are also crucial, as are a number of support staffers in the weeks-long process.
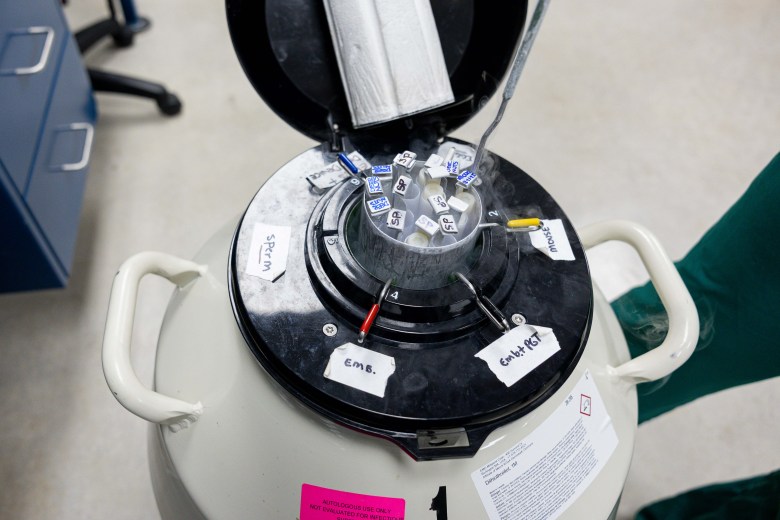 Katie Balloch, director of embryological training and education at IVF Academy USA, examines egg, sperm and embryo samples from a liquid nitrogen tank. Credit: Amber Esparza / San Antonio Report
Katie Balloch, director of embryological training and education at IVF Academy USA, examines egg, sperm and embryo samples from a liquid nitrogen tank. Credit: Amber Esparza / San Antonio Report
These specialties are in high demand given the multi-billion dollar explosion in the U.S. fertility market over the last few decades. The program gives OB-GYNs and other health providers certificates showcasing training in IVF procedures that is on par and often more intensive than many academic training programs, Magarelli said, allowing them to assist reproductive endocrinologists in the procedures.
“We’re so far behind the curve that the amount of graduates that we graduate equals the amount of folks who retire or die or leave the practice,” Magarelli said. “We’re at a net zero, and yet the need is hundreds and hundreds and hundreds and hundreds.”
IVF Academy USA’s solution: offer specialized training to OB-GYNs, nurse practitioners and physician assistants specifically in the IVF procedure. The practitioners who go through the 6-month training program gain more experience on IVF egg retrievals and transfers via hands-on training and simulations than in an average academic fellowship, Magarelli said.
“They’re not substitutes for reproductive endocrinologists,” Magarelli said, adding that the program has received some pushback from these practitioners. “They are additions. It’s a brand-new field of medicine. We’re adding to help because the need is so great.”
There are roughly 1,250 board-certified reproductive endocrinologists in the U.S. in active practice. In 2020, almost 300,000 IVF cycles were completed in the country, an average volume of 233 cycles per board-certified reproductive endocrinologist annually. The average REI provider would need to oversee approximately 1,600 IVF cycles per year to meet demand, according to a 2023 Science Direct article.
“We’re up for the challenge … we’re making the best adjuncts and supporters of the reproductive endocrinology and infertility community and the IVF industry out there,” he added.
