Seventy-five percent of U.S. adults would be considered obese under a new index that combines body measurements with body mass index (BMI), which has historically been the sole gauge for determining unhealthy weight ranges.
The researchers applied an updated obesity index put forward last January by the Lancet Diabetes and Endocrinology Commission, a group formed in 2022 to better define obesity, a rapidly growing issue worldwide.
According to a JAMA study published last week, the new index combines measurements like waist circumference, waist-to-hip ratio and waist-to-height with an individual’s BMI to more accurately capture body fat distribution and distinguish body fat from muscle mass.
When body measurements were incorporated, the researchers found that 4 in 5 U.S. adults who had a BMI classified as overweight would actually be considered obese. An additional 38% of people with a “healthy” BMI would also be reclassified as obese.
Just looking at BMI, the prevalence of obesity among U.S. adults was 40% from 2021-2023, according to the U.S. Centers for Disease Control and Prevention. Whether the updated figure is truly a better reflection of the obesity epidemic in the U.S. or reason for the commission to tweak its index is up for debate.
“I was shocked,” said Dr. Maria Escobar-Vasco, an endocrinologist and program director of UT Health San Antonio’s Endocrinology, Diabetes and Metabolism Training program. “Obesity is certainly an epidemic, and we’re seeing rising incidence and prevalence of obesity, but 75% [seems high].”
Obesity rates in the U.S. have skyrocketed since the early 1970s, when the BMI measurement was introduced and adapted by health care providers. At the same time, a larger conversation has grown around the complex causes of obesity, the stigma surrounding it, and whether obesity is a chronic disease itself (as the CDC and American Medical Association label it) or simply a risk factor for other diseases, like metabolic disease and type 2 diabetes, for example.
Dr. Aaron King, a family medicine physician with the Baptist Health System, said it’s hard to say what the 75% figure truly reflects because obesity still lacks an agreed upon and well-defined definition. The Lancet Commission was created in part to provide a more concrete answer to these questions.
“I think when you draw the line that’s always a question that is up for a little bit of debate,” King said. “But I think if you’re asking the question, ‘Do I think that 75% of U.S. adults have or are at high risk for developing metabolic disease?’ I think what we’re finding in the data is yes, sadly.”
What more researchers agree on is that BMI alone is not a reliable gauge for healthy weight ranges, and updating it would help providers more accurately tease out the interactions between obesity and the diseases that often accompany the condition.
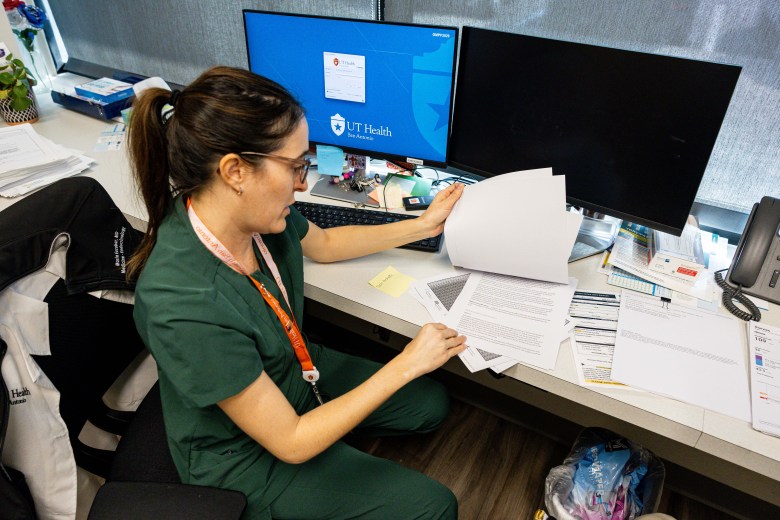 Dr. Maria Escobar-Vasco says medical offices should incorporate waist measurements into standard doctor visits when checking a patient’s BMI to get a more accurate picture of a patient’s health versus going off of BMI alone. Credit: Amber Esparza / San Antonio Report
Dr. Maria Escobar-Vasco says medical offices should incorporate waist measurements into standard doctor visits when checking a patient’s BMI to get a more accurate picture of a patient’s health versus going off of BMI alone. Credit: Amber Esparza / San Antonio Report
The problems with BMI and defining obesity
The BMI formula is simple: your weight (in kilograms) divided by your height (in meters) squared. Anything 30 and above is considered obese, and 40 and above is considered extreme obesity. You can find a full BMI table here.
BMI doesn’t take into account adipose tissue (body fat) versus muscle mass, bone density, and importantly, the distribution of body fat. As a result, BMI both overestimates and underestimates obesity.
“The classic example is, you can have a weightlifter who is 10% body fat or less, and might have a BMI over 30, which will classify as obesity,” King said. “But of course, all that weight is solid muscle, and that person likely doesn’t have any metabolic disease and certainly doesn’t have truncal obesity. And then you can also have people that have a BMI around 25 that have a normal BMI, and yet they might have truncal obesity and be at risk for disease.”
Truncal obesity, or excess stomach fat, also known as visceral fat, is especially associated with insulin resistance, metabolic disease, cardiovascular disease, among other comorbidities. On the other hand, fat stored around the hips, buttocks and thighs known as gluteofemoral fat plays a protective role against metabolic and cardiovascular disease.
The Lancet Commission hopes to address this flaw in BMI by including waist circumference, waist-to-hip ratio and waist-to-height measurements, helping health care providers screen for greater disease risk.
“The distribution of the fat makes a difference,” Escobar-Vasco said. “Inside of our belly, we have a lot of different very important organs that you need to be fully working. The liver, for example. If we don’t have any more fat tissue that can accumulate that extra fat, it’s going to go into the liver. And so that’s when we start having issues with what used to be called fatty liver disease.”
The group of people who fall into the normal BMI range but would otherwise be considered obese may not be able to access needed medications since insurance companies often require that a certain BMI threshold be met. It’s an especially common barrier for Asian Americans, a population for which researchers have recommended lower BMI thresholds to increase access to medications and surgery sooner.
It’s worth noting that the Lancet Commission made distinctions between pre-clinical obesity (defined as excess fat with preserved function of tissues and organs) and clinical obesity (defined as a chronic, systemic illness with alterations in the function of tissues, organs or the individual due to excessive adiposity). The JAMA study combined these two categories together into one, however.
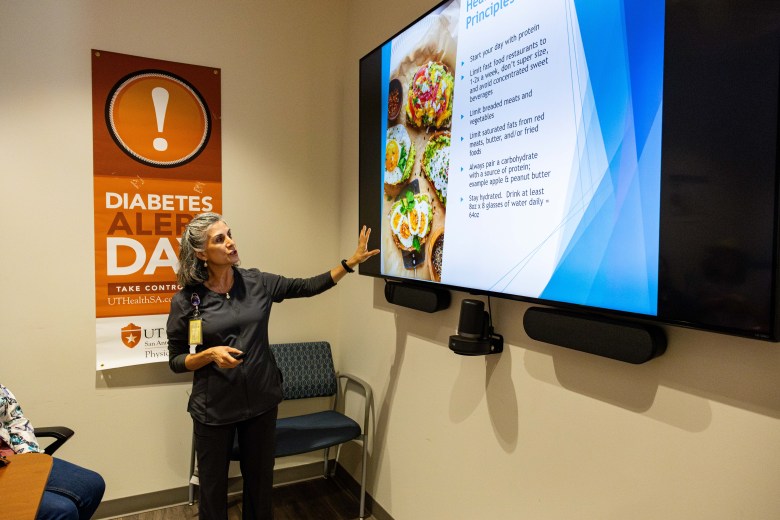 Registered dietician and diabetes educator Elizabeth McKenzie talks to patients about meal planning to manage diabetes at UT Health San Antonio’s office of Endocrinology, Diabetes, Obesity and Metabolic Health on Wednesday. Credit: Amber Esparza / San Antonio Report
Registered dietician and diabetes educator Elizabeth McKenzie talks to patients about meal planning to manage diabetes at UT Health San Antonio’s office of Endocrinology, Diabetes, Obesity and Metabolic Health on Wednesday. Credit: Amber Esparza / San Antonio Report
Looking forward
Despite its flaws, BMI is widely used in medical settings and well known by the public, largely because as a screening tool it’s quick, cheap and easy for clinicians to use.
“It’s mainly a convenience factor,” King said, “because we can get a weight and height really quickly. And so that’s what we all use. But the reality is that it’s probably not a good metric, but it’s just one that has fallen in favor, because it’s better than nothing.”
“BMI can give you an overall idea,” Escobar-Vasco added. “So they still advocate for it as a screening tool. [But] if we want to be really good about this, we should be getting waist-to-hip on everybody. It’s fairly easy.”
The JAMA researchers concluded that more research is likely needed on the new measurement before implementation. Such a change would likely take a period of education, for medical practitioners and the public, local doctors said.
“I think in a perfect world, we would never use BMI, knowing what we know now, but I think we’re kind of stuck with it,” King said. “It’s probably going to be a paradigm shift that will take several years to come off of using it.”
