Harvey, J. et al. Machine learning-based prediction of cognitive outcomes in de novo Parkinson’s disease. npj Parkinsons Dis. 8, 150 (2022).
Kandiah, N. et al. Montreal cognitive assessment for the screening and prediction of cognitive decline in early Parkinson’s disease. Parkinsonism Relat. Disord. 20, 1145–1148 (2014).
Wilson, H. et al. Predict cognitive decline with clinical markers in Parkinson’s disease (PRECODE-1). J. Neural Transm. 127, 51–59 (2020).
Garcia-Diaz, A. I. et al. Cortical thinning correlates of changes in visuospatial and visuoperceptual performance in Parkinson’s disease: a 4-year follow-up. Parkinsonism Relat. Disord. 46, 62–68 (2018).
Luca, A. et al. Cognitive impairment and levodopa induced dyskinesia in Parkinson’s disease: a longitudinal study from the PACOS cohort. Sci. Rep. 11, 867 (2021).
van Laar, T., De Deyn, P. P., Aarsland, D., Barone, P. & Galvin, J. E. Effects of cholinesterase inhibitors in Parkinson’s disease dementia: a review of clinical data. CNS Neurosci. Ther. 17, 428–441 (2011).
Sun, C. & Armstrong, M. J. Treatment of Parkinson’s disease with cognitive impairment: current approaches and future directions. Behav. Sci. 11, 54 (2021).
Bernini, S. et al. A double-blind randomized controlled trial of the efficacy of cognitive training delivered using two different methods in mild cognitive impairment in Parkinson’s disease: preliminary report of benefits associated with the use of a computerized tool. Aging Clin. Exp. Res. 33, 1567–1575 (2020).
Mantovani, E., Zucchella, C., Argyriou, A. A. & Tamburin, S. Treatment for cognitive and neuropsychiatric non-motor symptoms in Parkinson’s disease: current evidence and future perspectives. Expert Rev. Neurotherapeutics 23, 25–43 (2023).
Loetscher, T. Cognitive training interventions for dementia and mild cognitive impairment in Parkinson’s disease – a cochrane review summary with commentary. NeuroRehabilitation 48, 385–387 (2021).
Carlisle, T. C., Medina, L. D. & Holden, S. K. Original research: initial development of a pragmatic tool to estimate cognitive decline risk focusing on potentially modifiable factors in Parkinson’s disease. Front. Neurosci. 17, 1278817 (2023).
Pavelka, L. et al. Age at onset as stratifier in idiopathic Parkinson’s disease – effect of ageing and polygenic risk score on clinical phenotypes. npj Parkinsons Dis. 8, 102 (2022).
Chung, S. J. et al. Baseline cognitive profile is closely associated with long-term motor prognosis in newly diagnosed Parkinson’s disease. J. Neurol. 268, 4203–4212 (2021).
Yıldız, Z. et al. Relationship between apathy and cognitive functions in Parkinson’s disease. Psychological Appl. Trends https://doi.org/10.36315/2023inpact145 (2023).
Goldman, J. G. et al. Diagnosing PD-MCI by MDS Task Force criteria: how many and which neuropsychological tests?. Mov. Disord.30, 402–406 (2014).
Pan, F.-F., Huang, L., Chen, K.-L., Zhao, Q.-H. & Guo, Q.-H. A comparative study on the validations of three cognitive screening tests in identifying subtle cognitive decline. BMC Neurol. 20, 78 (2020).
Cersonsky, T. E. K. et al. Using the Montreal cognitive assessment to identify individuals with subtle cognitive decline. Neuropsychology 36, 373–383 (2022).
Mills, K. A. et al. Cognitive impairment in Parkinson’s disease: Association between patient-reported and clinically measured outcomes. Parkinsonism Relat. Disord. 33, 107–114 (2016).
Rosenblum, S. et al. The Montreal Cognitive Assessment: Is it suitable for identifying mild cognitive impairment in Parkinson’s disease?. Mov. Disord. Clin. Pract. 7, 648–655 (2020).
Marino, S. E. et al. Subjective perception of cognition is related to mood and not performance. Epilepsy Behav. 14, 459–464 (2009).
Goldman, J. G., Stebbins, G. T., Leung, V., Tilley, B. C. & Goetz, C. G. Relationships among cognitive impairment, sleep, and fatigue in Parkinson’s disease using the MDS-UPDRS. Parkinsonism Relat. Disord. 20, 1135–1139 (2014).
Huang, J. et al. Subjective cognitive decline in patients with Parkinson’s disease: an updated review. Front. Aging Neurosci. 15, 1117068 (2023).
Ren, J. et al. Comparing the effects of GBA variants and onset age on clinical features and progression in Parkinson’s disease. CNS Neurosci. Ther. 30, e14387 (2024).
Wang, Y.-X. et al. Associations between cognitive impairment and motor dysfunction in Parkinson’s disease. Brain Behav. 7, e00719 (2017).
Ikeda, M., Kataoka, H. & Ueno, S. Can levodopa prevent cognitive decline in patients with Parkinson’s disease?. Am. J. Neurodegener. Dis. 6, 9–14 (2017).
Loo, R. T. J. et al. Levodopa-induced dyskinesia in Parkinson’s disease: Insights from cross-cohort prognostic analysis using machine learning. Parkinsonism Relat. Disord. 126, 107054 (2024).
Pavelka, L. et al. Luxembourg Parkinson’s study -comprehensive baseline analysis of Parkinson’s disease and atypical parkinsonism. Front. Neurol. 14, 1330321 (2023).
Marek, K. et al. The Parkinson Progression Marker Initiative (PPMI). Prog. Neurobiol. 95, 629–635 (2011).
Dodet, P. et al. Sleep disorders in Parkinson’s disease, an early and multiple problem. npj Parkinson’s Dis. 10, 46 (2024).
Zhang, Z. et al. Effect of onset age on the levodopa threshold dosage for dyskinesia in Parkinson’s disease. Neurol. Sci. 43, 3165–3174 (2022).
Ciafone, J., Little, B., Thomas, A. J. & Gallagher, P. The neuropsychological profile of mild cognitive impairment in lewy body dementias. J. Int. Neuropsychol. Soc. 26, 210–225 (2020).
Devigili, G. et al. Unraveling autonomic dysfunction in GBA-related Parkinson’s disease. Mov. Disord. Clin. Pract. 10, 1620–1638 (2023).
Kelly, M. J. et al. Predictors of motor complications in early Parkinson’s disease: a prospective cohort study. Mov. Disord. 34, 1174–1183 (2019).
Chen, J. et al. Predictors of cognitive impairment in newly diagnosed Parkinson’s disease with normal cognition at baseline: A 5-year cohort study. Front. Aging Neurosci. 15, 1142558 (2023).
Biundo, R. et al. Cognitive profiling of Parkinson disease patients with mild cognitive impairment and dementia. Parkinsonism Relat. Disord. 20, 394–399 (2014).
Phongpreecha, T. et al. Multivariate prediction of dementia in Parkinson’s disease. npj Parkinson’s Dis. 6, 20 (2020).
Gorji, A. & Jouzdani, A. F. Machine learning for predicting cognitive decline within five years in Parkinson’s disease: comparing cognitive assessment scales with DAT SPECT and clinical biomarkers. PLoS ONE 19, e0304355 (2024).
Palermo, G. et al. Dopamine transporter, age, and motor complications in Parkinson’s disease: a clinical and single-photon emission computed tomography study. Mov. Disord. 35, 1028–1036 (2020).
Xiao, Y. et al. Different associated factors of subjective cognitive complaints in patients with early- and late-onset Parkinson’s disease. Front. Neurol. 12, 749471 (2021).
Zhou, F. et al. Abnormal intra- and inter-network functional connectivity of brain networks in early-onset Parkinson’s disease and late-onset Parkinson’s disease. Front. Aging Neurosci. 15, 1132723 (2023).
Picillo, M. et al. Sex-related longitudinal change of motor, non-motor, and biological features in early Parkinson’s disease. J. Parkinsons Dis. 12, 421–436 (2021).
Beheshti, I., Booth, S. & Ko, J. H. Differences in brain aging between sexes in Parkinson’s disease. npj Parkinsons Dis. 10, 35 (2024).
Iwaki, H. et al. Differences in the presentation and progression of Parkinson’s disease by sex. Mov. Disord. 36, 106–117 (2021).
Chen, H. et al. Performance of the Benton Judgment of Line Orientation test across patients with different types of dementia. J. Alzheimers Dis. 102, 437–448 (2024).
Cholerton, B. et al. Sex differences in progression to mild cognitive impairment and dementia in Parkinson’s disease. Parkinsonism Relat. Disord. 50, 29–36 (2018).
Chiara, P. et al. Cognitive function in Parkinson’s disease: the influence of gender. Basal Ganglia 3, 131–135 (2013).
Bakeberg, M. C. et al. Differential effects of sex on longitudinal patterns of cognitive decline in Parkinson’s disease. J. Neurol. 268, 1903–1912 (2021).
Reekes, T. H. et al. Sex specific cognitive differences in Parkinson disease. npj Parkinsons Dis. 6, 7 (2020).
Almgren, H. et al. Machine learning-based prediction of longitudinal cognitive decline in early Parkinson’s disease using multimodal features. Sci. Rep. 13, 13193 (2023).
Kang, S. H., Lee, J. & Koh, S.-B. Constipation is associated with mild cognitive impairment in patients with de novo Parkinson’s disease. J. Mov. Disord. 15, 38–42 (2021).
Jones, J. D., Rahmani, E., Garcia, E. & Jacobs, J. P. Gastrointestinal symptoms are predictive of trajectories of cognitive functioning in de novo Parkinson’s disease. Parkinsonism Relat. Disord. 72, 7–12 (2020).
Tur, E. K. & Gözke, E. Autonomic symptoms in early-stage Parkinson’s patients and their relationship with cognition and disease parameters. Anatol. Curr. Med J.5, 498–502 (2023).
Nagy, A. V. et al. Cognitive impairment in REM-sleep behaviour disorder and individuals at risk of Parkinson’s disease. Parkinsonism Relat. Disord. 109, 105312 (2023).
Maggi, G., Trojano, L., Barone, P. & Santangelo, G. Sleep disorders and cognitive dysfunctions in Parkinson’s disease: a meta-analytic study. Neuropsychol. Rev. 31, 643–682 (2021).
Cosgrove, J., Alty, J. E. & Jamieson, S. Cognitive impairment in Parkinson’s disease. Postgrad. Med. J. 91, 212–220 (2015).
Ma, C.-H., Ren, N., Xu, J. & Chen, L. Clinical features, plasma neurotransmitter levels and plasma neurohormone levels among patients with early-stage Parkinson’s disease with sleep disorders. Cell Commun. Signal. 23, 144 (2025).
Gibb, W. R. & Lees, A. J. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 51, 745–752 (1988).
Marek, K. et al. The Parkinson’s progression markers initiative (PPMI) – establishing a PD biomarker cohort. Ann. Clin. Transl. Neurol. 5, 1460–1477 (2018).
Rosenblum, S., Meyer, S., Richardson, A. & Hassin-Baer, S. Capturing subjective mild cognitive decline in Parkinson’s disease. Brain Sci. 12, 741 (2022).
Azur, M. J., Stuart, E. A., Frangakis, C. & Leaf, P. J. Multiple imputation by chained equations: what is it and how does it work?. Int. J. Methods Psychiatr. Res. 20, 40–49 (2011).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Soft. 45, 1–67 (2011).
Luo, J. et al. A comparison of batch effect removal methods for enhancement of prediction performance using MAQC-II microarray gene expression data. Pharmacogenomics J. 10, 278–291 (2010).
Bolstad, B. M., Irizarry, R. A., Åstrand, M. & Speed, T. P. A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. Bioinformatics 19, 185–193 (2003).
Kostka, D. & Spang, R. Microarray based diagnosis profits from better documentation of gene expression signatures. PLoS Comput. Biol. 4, e22 (2008).
Johnson, W. E., Li, C. & Rabinovic, A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 8, 118–127 (2007).
Chen, C. et al. Removing batch effects in analysis of expression microarray data: an evaluation of six batch adjustment methods. PLoS One 6, e17238 (2011).
Lazar, C. et al. Batch effect removal methods for microarray gene expression data integration: a survey. Brief. Bioinform. 14, 469–490 (2012).
Stein, C. K. et al. Removing batch effects from purified plasma cell gene expression microarrays with modified ComBat. BMC Bioinforma. 16, 63 (2015).
Bach, M., Werner, A. & Palt, M. The proposal of undersampling method for learning from imbalanced datasets. Proc. Comput. Sci. 159, 125–134 (2019).
Karami, G., Giuseppe Orlando, M., Delli Pizzi, A., Caulo, M. & Del Gratta, C. Predicting overall survival time in glioblastoma patients using gradient boosting machines algorithm and recursive feature elimination technique. Cancers 13, 4976 (2021).
Wood, I. A., Visscher, P. M. & Mengersen, K. L. Classification based upon gene expression data: bias and precision of error rates. Bioinformatics 23, 1363–1370 (2007).
Freund, Y. & Schapire, R. E. A decision-theoretic generalization of on-line learning and an application to boosting. J. Comput. Syst. Sci. 55, 119–139 (1997).
Freund, Y. & Schapire, R. A short introduction to boosting. J. Jpn. Soc. Artif. 14, 1612 (1999).
Berk, R. A. Classification and Regression Trees (CART). In Statistical Learning from a Regression Perspective (ed. Berk, R. A.) 157–211 (Springer International Publishing, 2020). https://doi.org/10.1007/978-3-030-40189-4_3.
Prokhorenkova, L., Gusev, G., Vorobev, A., Dorogush, A. V. & Gulin, A. CatBoost: unbiased boosting with categorical features. In Advances in Neural Information Processing Systems ((NeurIPS, 2018).
Quinlan, J. R. Improved use of continuous attributes in C4.5. J. Artif. Intell. Res. 4, 77–90 (1996).
Tan, Y. S. et al. Fast interpretable greedy-tree sums. Proc. Natl. Acad. Sci. U.S.A. 122, e2310151122 (2025).
McTavish, H. et al. Fast Sparse Decision Tree Optimization via reference ensembles. AAAI 36, 9604–9613 (2022).
Friedman, J. H. Greedy function approximation: a gradient boosting machine. Ann. Stat. 29, 1189–1232 (2001).
Agarwal, A., Tan, Y. S., Ronen, O., Singh, C. & Yu, B. Hierarchical shrinkage: improving the accuracy and interpretability of tree-based models. In International Conference on Machine Learning 111–135 (PMLR, 2022).
Chen, T. & Guestrin, C. XGBoost: a scalable tree boosting system. In ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, 785–794, https://doi.org/10.1145/2939672.2939785 (2016).
He, K. et al. Component-wise gradient boosting and false discovery control in survival analysis with high-dimensional covariates. Bioinformatics 32, 50–57 (2015).
Bertsimas, D., Dunn, J., Gibson, E. & Orfanoudaki, A. Optimal survival trees. Mach. Learn. 111, 2951–3023 (2022).
Geurts, P., Ernst, D. & Wehenkel, L. Extremely randomized trees. Mach. Learn. 63, 3–42 (2006).
Wang, M. et al. Dementia risk prediction in individuals with mild cognitive impairment: a comparison of Cox regression and machine learning models. BMC Med. Res. Methodol. 22, 284 (2022).
Park, M. Y. & Hastie, T. L1-regularization path algorithm for generalized linear models. J. R. Stat. Soc. Ser. B Stat. Methodol. 69, 659–677 (2007).
Simon, N., Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for Cox’s proportional hazards model via coordinate descent. J. Stat. Softw. 39, 1–13 (2011).
Ishwaran, H., Kogalur, U. B., Blackstone, E. H. & Lauer, M. S. Random survival forests. Ann. Appl. Stat. 2, 841–860 (2008).
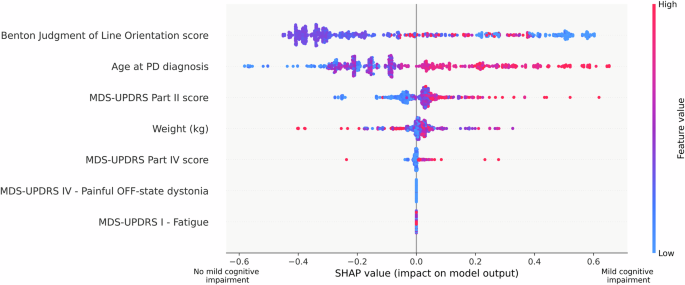
Lundberg, S. M. & Lee, S.-I. A unified approach to interpreting model predictions. In Neural Information Processing Systems (NIPS 2017) 4768–4777 (NIPS, 2017).
Sundrani, S. & Lu, J. Computing the hazard ratios associated with explanatory variables using machine learning models of survival data. JCO Clin. Cancer Inform. 5, 364–378 (2021).
Sun, X. & Xu, W. Fast implementation of DeLong’s algorithm for comparing the areas under correlated receiver operating characteristic curves. IEEE Signal Process. Lett. 21, 1389–1393 (2014).
Kang, L., Chen, W., Petrick, N. A. & Gallas, B. D. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat. Med. 34, 685–703 (2015).
Ferreira, J. A. & Zwinderman, A. H. On the Benjamini–Hochberg method. Ann. Stat. 34, 1827–1849 (2006).
Corani, G. & Benavoli, A. A Bayesian approach for comparing cross-validated algorithms on multiple data sets. Mach. Learn. 100, 285–304 (2015).
Piovani, D., Sokou, R., Tsantes, A. G., Vitello, A. S. & Bonovas, S. Optimizing clinical decision making with decision curve analysis: Insights for clinical investigators. Healthcare 11, 2244 (2023).
Zhang, Z. et al. Decision curve analysis: a technical note. Ann. Transl. Med. 6, 308 (2018).
Trucano, T. G., Swiler, L. P., Igusa, T., Oberkampf, W. L. & Pilch, M. Calibration, validation, and sensitivity analysis: What’s what. Reliab. Eng. Syst. Saf. 91, 1331–1357 (2006).
Bamber, D. Evaluation of the performance of survival analysis models: Discrimination and calibration measures. In Handbook of Statistics vol. 23 1–25 (Elsevier, 2003).