Wilson DM 3rd, Cookson MR, Van Den Bosch L, Zetterberg H, Holtzman DM, Dewachter I. Hallmarks of neurodegenerative diseases. Cell. 2023;186(4):693–714.
Robinson JL, Lee EB, Xie SX, Rennert L, Suh E, Bredenberg C, Caswell C, Van Deerlin VM, Yan N, Yousef A, et al. Neurodegenerative disease concomitant proteinopathies are prevalent, age-related and APOE4-associated. Brain. 2018;141(7):2181–93.
Kovacs GG. Are comorbidities compatible with a molecular pathological classification of neurodegenerative diseases? Curr Opin Neurol. 2019;32(2):279–91.
Spires-Jones TL, Attems J, Thal DR. Interactions of pathological proteins in neurodegenerative diseases. Acta Neuropathol. 2017;134(2):187–205.
Wang C, Telpoukhovskaia MA, Bahr BA, Chen X, Gan L. Endo-lysosomal dysfunction: a converging mechanism in neurodegenerative diseases. Curr Opin Neurobiol. 2018;48:52–8.
Todd TW, Shao W, Zhang YJ, Petrucelli L. The endolysosomal pathway and ALS/FTD. Trends Neurosci. 2023;46(12):1025–41.
Van Deerlin VM, Sleiman PM, Martinez-Lage M, Chen-Plotkin A, Wang LS, Graff-Radford NR, Dickson DW, Rademakers R, Boeve BF, Grossman M, et al. Common variants at 7p21 are associated with frontotemporal Lobar degeneration with TDP-43 inclusions. Nat Genet. 2010;42(3):234–9.
Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, Snowden J, Adamson J, Sadovnick AD, Rollinson S, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442(7105):916–9.
Cruts M, Gijselinck I, van der Zee J, Engelborghs S, Wils H, Pirici D, Rademakers R, Vandenberghe R, Dermaut B, Martin JJ, et al. Null mutations in progranulin cause ubiquitin-positive frontotemporal dementia linked to chromosome 17q21. Nature. 2006;442(7105):920–4.
Feng T, Lacrampe A, Hu F. Physiological and pathological functions of TMEM106B: a gene associated with brain aging and multiple brain disorders. Acta Neuropathol. 2021;141(3):327–39.
Rhinn H, Tatton N, McCaughey S, Kurnellas M, Rosenthal A. Progranulin as a therapeutic target in neurodegenerative diseases. Trends Pharmacol Sci. 2022;43(8):641–52.
Van Mossevelde S, Engelborghs S, van der Zee J, Van Broeckhoven C. Genotype-phenotype links in frontotemporal Lobar degeneration. Nat Rev Neurol. 2018;14(6):363–78.
Grossman M, Seeley WW, Boxer AL, Hillis AE, Knopman DS, Ljubenov PA, Miller B, Piguet O, Rademakers R, Whitwell JL, et al. Frontotemporal Lobar degeneration. Nat Rev Dis Primers. 2023;9(1):40.
Rademakers R, Baker M, Gass J, Adamson J, Huey ED, Momeni P, Spina S, Coppola G, Karydas AM, Stewart H, et al. Phenotypic variability associated with progranulin haploinsufficiency in patients with the common 1477C–>T (Arg493X) mutation: an international initiative. Lancet Neurol. 2007;6(10):857–68.
Sakae N, Roemer SF, Bieniek KF, Murray ME, Baker MC, Kasanuki K, Graff-Radford NR, Petrucelli L, Van Blitterswijk M, Rademakers R, et al. Microglia in frontotemporal Lobar degeneration with progranulin or C9ORF72 mutations. Ann Clin Transl Neurol. 2019;6(9):1782–96.
Lui H, Zhang J, Makinson SR, Cahill MK, Kelley KW, Huang HY, Shang Y, Oldham MC, Martens LH, Gao F, et al. Progranulin deficiency promotes Circuit-Specific synaptic pruning by microglia via complement activation. Cell. 2016;165(4):921–35.
Marsan E, Velmeshev D, Ramsey A, Patel RK, Zhang J, Koontz M, Andrews MG, de Majo M, Mora C, Blumenfeld J et al. Astroglial toxicity promotes synaptic degeneration in the thalamocortical circuit in frontotemporal dementia with GRN mutations. J Clin Invest 2023, 133(6).
Gerrits E, Giannini LAA, Brouwer N, Melhem S, Seilhean D, Le Ber I, Brainbank Neuro CEBNN, Kamermans A, Kooij G, de Vries HE, et al. Neurovascular dysfunction in GRN-associated frontotemporal dementia identified by single-nucleus RNA sequencing of human cerebral cortex. Nat Neurosci. 2022;25(8):1034–48.
Zhou X, Kukar T, Rademakers R. Lysosomal dysfunction and other pathomechanisms in FTLD: evidence from progranulin genetics and biology. Adv Exp Med Biol. 2021;1281:219–42.
Shankaran SS, Capell A, Hruscha AT, Fellerer K, Neumann M, Schmid B, Haass C. Missense mutations in the progranulin gene linked to frontotemporal Lobar degeneration with ubiquitin-immunoreactive inclusions reduce progranulin production and secretion. J Biol Chem. 2008;283(3):1744–53.
Pinarbasi ES, Karamyshev AL, Tikhonova EB, Wu IH, Hudson H, Thomas PJ. Pathogenic signal sequence mutations in progranulin disrupt SRP interactions required for mRNA stability. Cell Rep. 2018;23(10):2844–51.
Smith KR, Damiano J, Franceschetti S, Carpenter S, Canafoglia L, Morbin M, Rossi G, Pareyson D, Mole SE, Staropoli JF, et al. Strikingly different clinicopathological phenotypes determined by progranulin-mutation dosage. Am J Hum Genet. 2012;90(6):1102–7.
Canafoglia L, Morbin M, Scaioli V, Pareyson D, D’Incerti L, Fugnanesi V, Tagliavini F, Berkovic SF, Franceschetti S. Recurrent generalized seizures, visual loss, and palinopsia as phenotypic features of neuronal ceroid lipofuscinosis due to progranulin gene mutation. Epilepsia. 2014;55(6):e56–59.
Almeida MR, Macario MC, Ramos L, Baldeiras I, Ribeiro MH, Santana I. Portuguese family with the co-occurrence of frontotemporal Lobar degeneration and neuronal ceroid lipofuscinosis phenotypes due to progranulin gene mutation. Neurobiol Aging. 2016;41:200. e201-200 e205.
Faber I, Prota JR, Martinez AR, Lopes-Cendes I, Franca MCJ. A new phenotype associated with homozygous GRN mutations: complicated spastic paraplegia. Eur J Neurol. 2017;24(1):e3–4.
Kamate M, Detroja M, Hattiholi V. Neuronal ceroid lipofuscinosis type-11 in an adolescent. Brain Dev. 2019;41(6):542–5.
Nobrega PR, Paiva ARB, Amorim Junior AD, Lima P, Cabral KSS, Barcelos IP, Pessoa ALS, Souza-Lima CFL, Castro MAA, Freua F, et al. Further description of the phenotypic spectrum of neuronal ceroid lipofuscinosis type 11. Genet Med. 2025;27(1):101291.
Huin V, Barbier M, Bottani A, Lobrinus JA, Clot F, Lamari F, Chat L, Rucheton B, Fluchere F, Auvin S, et al. Homozygous GRN mutations: new phenotypes and new insights into pathological and molecular mechanisms. Brain. 2020;143(1):303–19.
Lee MJ, Chen TF, Cheng TW, Chiu MJ. rs5848 variant of progranulin gene is a risk of alzheimer’s disease in the Taiwanese population. Neurodegener Dis. 2011;8(4):216–20.
Sheng J, Su L, Xu Z, Chen G. Progranulin polymorphism rs5848 is associated with increased risk of alzheimer’s disease. Gene. 2014;542(2):141–5.
Xu HM, Tan L, Wan Y, Tan MS, Zhang W, Zheng ZJ, Kong LL, Wang ZX, Jiang T, Tan L, et al. PGRN is associated with Late-Onset alzheimer’s disease: a Case-Control replication study and Meta-analysis. Mol Neurobiol. 2017;54(2):1187–95.
Wightman DP, Jansen IE, Savage JE, Shadrin AA, Bahrami S, Holland D, Rongve A, Borte S, Winsvold BS, Drange OK, et al. A genome-wide association study with 1,126,563 individuals identifies new risk loci for alzheimer’s disease. Nat Genet. 2021;53(9):1276–82.
Nalls MA, Blauwendraat C, Vallerga CL, Heilbron K, Bandres-Ciga S, Chang D, Tan M, Kia DA, Noyce AJ, Xue A, et al. Identification of novel risk loci, causal insights, and heritable risk for parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 2019;18(12):1091–102.
Bellenguez C, Kucukali F, Jansen IE, Kleineidam L, Moreno-Grau S, Amin N, Naj AC, Campos-Martin R, Grenier-Boley B, Andrade V, et al. New insights into the genetic etiology of alzheimer’s disease and related dementias. Nat Genet. 2022;54(4):412–36.
Brouwers N, Nuytemans K, van der Zee J, Gijselinck I, Engelborghs S, Theuns J, Kumar-Singh S, Pickut BA, Pals P, Dermaut B, et al. Alzheimer and Parkinson diagnoses in progranulin null mutation carriers in an extended founder family. Arch Neurol. 2007;64(10):1436–46.
Brouwers N, Sleegers K, Engelborghs S, Maurer-Stroh S, Gijselinck I, van der Zee J, Pickut BA, Van den Broeck M, Mattheijssens M, Peeters K, et al. Genetic variability in progranulin contributes to risk for clinically diagnosed alzheimer disease. Neurology. 2008;71(9):656–64.
Cortini F, Fenoglio C, Guidi I, Venturelli E, Pomati S, Marcone A, Scalabrini D, Villa C, Clerici F, Dalla Valle E, et al. Novel exon 1 progranulin gene variant in alzheimer’s disease. Eur J Neurol. 2008;15(10):1111–7.
Kelley BJ, Haidar W, Boeve BF, Baker M, Shiung M, Knopman DS, Rademakers R, Hutton M, Adamson J, Kuntz KM, et al. Alzheimer disease-like phenotype associated with the c.154delA mutation in progranulin. Arch Neurol. 2010;67(2):171–7.
Perry DC, Lehmann M, Yokoyama JS, Karydas A, Lee JJ, Coppola G, Grinberg LT, Geschwind D, Seeley WW, Miller BL, et al. Progranulin mutations as risk factors for alzheimer disease. JAMA Neurol. 2013;70(6):774–8.
Piaceri I, Imperiale D, Ghidoni E, Atzori C, Bagnoli S, Ferrari C, Ungari S, Ambrogio L, Sorbi S, Nacmias B. Novel GRN mutations in alzheimer’s disease and frontotemporal Lobar degeneration. J Alzheimers Dis. 2018;62(4):1683–9.
Redaelli V, Rossi G, Maderna E, Kovacs GG, Piccoli E, Caroppo P, Cacciatore F, Spinello S, Grisoli M, Sozzi G, et al. Alzheimer neuropathology without frontotemporal Lobar degeneration hallmarks (TAR DNA-binding protein 43 inclusions) in missense progranulin mutation Cys139Arg. Brain Pathol. 2018;28(1):72–6.
Bonato G, Campagnolo M, Emmi A, Misenti V, Carrer T, Fogliano C, Salviati L, Carecchio M, Antonini A. Progranulin mutation manifesting as Parkinson disease: A case series from the PADUA-CESNE cohort. Mov Disord Clin Pract 2025.
Rovelet-Lecrux A, Deramecourt V, Legallic S, Maurage CA, Le Ber I, Brice A, Lambert JC, Frebourg T, Hannequin D, Pasquier F, et al. Deletion of the progranulin gene in patients with frontotemporal Lobar degeneration or Parkinson disease. Neurobiol Dis. 2008;31(1):41–5.
Wauters E, Van Mossevelde S, Sleegers K, van der Zee J, Engelborghs S, Sieben A, Vandenberghe R, Philtjens S, Van den Broeck M, Peeters K, et al. Clinical variability and onset age modifiers in an extended Belgian GRN founder family. Neurobiol Aging. 2018;67:84–94.
Kelley BJ, Haidar W, Boeve BF, Baker M, Graff-Radford NR, Krefft T, Frank AR, Jack CR Jr., Shiung M, Knopman DS, et al. Prominent phenotypic variability associated with mutations in progranulin. Neurobiol Aging. 2009;30(5):739–51.
Liu C, Dong L, Wang J, Li J, Huang X, Lei D, Mao C, Chu S, Sha L, Xu Q, et al. GRN mutation spectrum and genotype-phenotype correlation in Chinese dementia patients: data from PUMCH dementia cohort. J Med Genet. 2024;61(6):543–8.
Reho P, Koga S, Shah Z, Chia R, International LBDGC, American Genome C, Rademakers R, Dalgard CL, Boeve BF, Beach TG, et al. GRN mutations are associated with lewy body dementia. Mov Disord. 2022;37(9):1943–8.
Masters CL, Bateman R, Blennow K, Rowe CC, Sperling RA, Cummings JL. Alzheimer’s disease. Nat Rev Dis Primers. 2015;1:15056.
Takahashi H, Bhagwagar S, Nies SH, Ye H, Han X, Chiasseu MT, Wang G, Mackenzie IR, Strittmatter SM. Reduced progranulin increases Tau and alpha-synuclein inclusions and alters mouse Tauopathy phenotypes via glucocerebrosidase. Nat Commun. 2024;15(1):1434.
Mendsaikhan A, Tooyama I, Bellier JP, Serrano GE, Sue LI, Lue LF, Beach TG, Walker DG. Characterization of lysosomal proteins progranulin and prosaposin and their interactions in alzheimer’s disease and aged brains: increased levels correlate with neuropathology. Acta Neuropathol Commun. 2019;7(1):215.
Pereson S, Wils H, Kleinberger G, McGowan E, Vandewoestyne M, Van Broeck B, Joris G, Cuijt I, Deforce D, Hutton M, et al. Progranulin expression correlates with dense-core amyloid plaque burden in alzheimer disease mouse models. J Pathol. 2009;219(2):173–81.
Takahashi H, Klein ZA, Bhagat SM, Kaufman AC, Kostylev MA, Ikezu T, Strittmatter SM. Alzheimer’s disease neuroimaging I: opposing effects of progranulin deficiency on amyloid and Tau pathologies via microglial TYROBP network. Acta Neuropathol. 2017;133(5):785–807.
Hosokawa M, Kondo H, Serrano GE, Beach TG, Robinson AC, Mann DM, Akiyama H, Hasegawa M, Arai T. Accumulation of multiple neurodegenerative disease-related proteins in Familial frontotemporal Lobar degeneration associated with granulin mutation. Sci Rep. 2017;7(1):1513.
Leverenz JB, Yu CE, Montine TJ, Steinbart E, Bekris LM, Zabetian C, Kwong LK, Lee VM, Schellenberg GD, Bird TD. A novel progranulin mutation associated with variable clinical presentation and tau, TDP43 and alpha-synuclein pathology. Brain. 2007;130(Pt 5):1360–74.
Sieben A, Van Mossevelde S, Wauters E, Engelborghs S, van der Zee J, Van Langenhove T, Santens P, Praet M, Boon P, Miatton M, et al. Extended FTLD pedigree segregating a Belgian GRN-null mutation: neuropathological heterogeneity in one family. Alzheimers Res Ther. 2018;10(1):7.
Takeda T, Seilhean D, Le Ber I, Millecamps S, Sazdovitch V, Kitagawa K, Uchihara T, Duyckaerts C. Amygdala TDP-43 pathology in frontotemporal Lobar degeneration and motor neuron disease. J Neuropathol Exp Neurol. 2017;76(9):800–12.
Jian J, Zhao S, Tian QY, Liu H, Zhao Y, Chen WC, Grunig G, Torres PA, Wang BC, Zeng B, et al. Association between progranulin and gaucher disease. EBioMedicine. 2016;11:127–37.
van Blitterswijk M, Mullen B, Wojtas A, Heckman MG, Diehl NN, Baker MC, DeJesus-Hernandez M, Brown PH, Murray ME, Hsiung GY, et al. Genetic modifiers in carriers of repeat expansions in the C9ORF72 gene. Mol Neurodegener. 2014;9:38.
Sleegers K, Brouwers N, Maurer-Stroh S, van Es MA, Van Damme P, van Vught PW, van der Zee J, Serneels S, De Pooter T, Van den Broeck M, et al. Progranulin genetic variability contributes to amyotrophic lateral sclerosis. Neurology. 2008;71(4):253–9.
Nelson PT, Dickson DW, Trojanowski JQ, Jack CR, Boyle PA, Arfanakis K, Rademakers R, Alafuzoff I, Attems J, Brayne C, et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain. 2019;142(6):1503–27.
Nicholson AM, Finch NA, Wojtas A, Baker MC, Perkerson RB 3rd, Castanedes-Casey M, Rousseau L, Benussi L, Binetti G, Ghidoni R, et al. TMEM106B p.T185S regulates TMEM106B protein levels: implications for frontotemporal dementia. J Neurochem. 2013;126(6):781–91.
Finch N, Carrasquillo MM, Baker M, Rutherford NJ, Coppola G, Dejesus-Hernandez M, Crook R, Hunter T, Ghidoni R, Benussi L, et al. TMEM106B regulates progranulin levels and the penetrance of FTLD in GRN mutation carriers. Neurology. 2011;76(5):467–74.
Cruchaga C, Graff C, Chiang HH, Wang J, Hinrichs AL, Spiegel N, Bertelsen S, Mayo K, Norton JB, Morris JC, et al. Association of TMEM106B gene polymorphism with age at onset in granulin mutation carriers and plasma granulin protein levels. Arch Neurol. 2011;68(5):581–6.
Perneel J, Manoochehri M, Huey ED, Rademakers R, Goldman J. Case report: TMEM106B haplotype alters penetrance of GRN mutation in frontotemporal dementia family. Front Neurol. 2023;14:1160248.
Pottier C, Zhou X, Perkerson RB 3rd, Baker M, Jenkins GD, Serie DJ, Ghidoni R, Benussi L, Binetti G, Lopez de Munain A, et al. Potential genetic modifiers of disease risk and age at onset in patients with frontotemporal Lobar degeneration and GRN mutations: a genome-wide association study. Lancet Neurol. 2018;17(6):548–58.
Lattante S, Le Ber I, Galimberti D, Serpente M, Rivaud-Pechoux S, Camuzat A, Clot F, Fenoglio C, French research network on FTD, Ftd ALS. Defining the association of TMEM106B variants among frontotemporal Lobar degeneration patients with GRN mutations and C9orf72 repeat expansions. Neurobiol Aging. 2014;35(11):e26582651–5.
Serpente M, Fenoglio C, Clerici F, Bonsi R, Arosio B, Cioffi SM, Rotondo E, Franceschi M, Martinelli Boneschi F, Mari D, et al. Transmembrane protein 106B gene (TMEM106B) variability and influence on progranulin plasma levels in patients with alzheimer’s disease. J Alzheimers Dis. 2015;43(3):757–61.
Chemparathy A, Le Guen Y, Zeng Y, Gorzynski J, Jensen TD, Yang C, Kasireddy N, Talozzi L, Belloy M, Stewart I, et al. A 3’UTR insertion is a candidate causal variant at the TMEM106B locus associated with increased risk for FTLD-TDP. Neurol Genet. 2024;10(1):e200124.
van Blitterswijk M, Mullen B, Nicholson AM, Bieniek KF, Heckman MG, Baker MC, DeJesus-Hernandez M, Finch NA, Brown PH, Murray ME, et al. TMEM106B protects C9ORF72 expansion carriers against frontotemporal dementia. Acta Neuropathol. 2014;127(3):397–406.
Gallagher MD, Suh E, Grossman M, Elman L, McCluskey L, Van Swieten JC, Al-Sarraj S, Neumann M, Gelpi E, Ghetti B, et al. TMEM106B is a genetic modifier of frontotemporal Lobar degeneration with C9orf72 hexanucleotide repeat expansions. Acta Neuropathol. 2014;127(3):407–18.
Bellenguez C, Kucukali F, Jansen IE, Kleineidam L, Moreno-Grau S, Amin N, Naj AC, Campos-Martin R, Grenier-Boley B, Andrade V et al. New insights into the genetic etiology of Alzheimer’s disease and related dementias. Nat Genet 2022.
Hu Y, Sun JY, Zhang Y, Zhang H, Gao S, Wang T, Han Z, Wang L, Sun BL, Liu G. rs1990622 variant associates with alzheimer’s disease and regulates TMEM106B expression in human brain tissues. BMC Med. 2021;19(1):11.
Cherry JD, Mez J, Crary JF, Tripodis Y, Alvarez VE, Mahar I, Huber BR, Alosco ML, Nicks R, Abdolmohammadi B, et al. Variation in TMEM106B in chronic traumatic encephalopathy. Acta Neuropathol Commun. 2018;6(1):115.
Tropea TF, Mak J, Guo MH, Xie SX, Suh E, Rick J, Siderowf A, Weintraub D, Grossman M, Irwin D, et al. TMEM106B effect on cognition in Parkinson disease and frontotemporal dementia. Ann Neurol. 2019;85(6):801–11.
Manini A, Ratti A, Brusati A, Maranzano A, Fogh I, Peverelli S, Messina S, Gentilini D, Verde F, Poletti B et al. TMEM106B acts as a modifier of cognitive and motor functions in amyotrophic lateral sclerosis. Int J Mol Sci 2022, 23(16).
Vass R, Ashbridge E, Geser F, Hu WT, Grossman M, Clay-Falcone D, Elman L, McCluskey L, Lee VM, Van Deerlin VM, et al. Risk genotypes at TMEM106B are associated with cognitive impairment in amyotrophic lateral sclerosis. Acta Neuropathol. 2011;121(3):373–80.
Simons C, Dyment D, Bent SJ, Crawford J, D’Hooghe M, Kohlschutter A, Venkateswaran S, Helman G, Poll-The BT, Makowski CC, et al. A recurrent de Novo mutation in TMEM106B causes hypomyelinating leukodystrophy. Brain. 2017;140(12):3105–11.
Perneel J, Rademakers R. Identification of TMEM106B amyloid fibrils provides an updated view of TMEM106B biology in health and disease. Acta Neuropathol. 2022;144(5):807–19.
Gallagher MD, Posavi M, Huang P, Unger TL, Berlyand Y, Gruenewald AL, Chesi A, Manduchi E, Wells AD, Grant SFA, et al. A Dementia-Associated risk variant near TMEM106B alters chromatin architecture and gene expression. Am J Hum Genet. 2017;101(5):643–63.
van der Zee J, Van Langenhove T, Kleinberger G, Sleegers K, Engelborghs S, Vandenberghe R, Santens P, Van den Broeck M, Joris G, Brys J, et al. TMEM106B is associated with frontotemporal Lobar degeneration in a clinically diagnosed patient cohort. Brain. 2011;134(Pt 3):808–15.
Yu L, De Jager PL, Yang J, Trojanowski JQ, Bennett DA, Schneider JA. The TMEM106B locus and TDP-43 pathology in older persons without FTLD. Neurology. 2015;84(9):927–34.
Rodney A, Karanjeet K, Benzow K, Koob MD. A common Alu insertion in the 3’UTR of TMEM106B is associated with risk of dementia. Alzheimers Dement. 2024;20(7):5071–7.
Lee JY, Harney DJ, Teo JD, Kwok JB, Sutherland GT, Larance M, Don AS. The major TMEM106B dementia risk allele affects TMEM106B protein levels, fibril formation, and Myelin lipid homeostasis in the ageing human hippocampus. Mol Neurodegener. 2023;18(1):63.
Hou Y, Dan X, Babbar M, Wei Y, Hasselbalch SG, Croteau DL, Bohr VA. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol. 2019;15(10):565–81.
Rhinn H, Abeliovich A. Differential aging analysis in human cerebral cortex identifies variants in TMEM106B and GRN that regulate aging phenotypes. Cell Syst. 2017;4(4):404–15. e405.
Li Z, Farias FHG, Dube U, Del-Aguila JL, Mihindukulasuriya KA, Fernandez MV, Ibanez L, Budde JP, Wang F, Lake AM, et al. The TMEM106B FTLD-protective variant, rs1990621, is also associated with increased neuronal proportion. Acta Neuropathol. 2020;139(1):45–61.
Tesi N, van der Lee S, Hulsman M, van Schoor NM, Huisman M, Pijnenburg Y, van der Flier WM, Reinders M, Holstege H. Cognitively healthy centenarians are genetically protected against alzheimer’s disease. Alzheimers Dement. 2024;20(6):3864–75.
Ahmed Z, Sheng H, Xu YF, Lin WL, Innes AE, Gass J, Yu X, Wuertzer CA, Hou H, Chiba S, et al. Accelerated lipofuscinosis and ubiquitination in granulin knockout mice suggest a role for progranulin in successful aging. Am J Pathol. 2010;177(1):311–24.
Luningschror P, Werner G, Stroobants S, Kakuta S, Dombert B, Sinske D, Wanner R, Lullmann-Rauch R, Wefers B, Wurst W, et al. The FTLD risk factor TMEM106B regulates the transport of lysosomes at the axon initial segment of motoneurons. Cell Rep. 2020;30(10):3506–19. e3506.
Brunk UT, Terman A. Lipofuscin: mechanisms of age-related accumulation and influence on cell function. Free Radic Biol Med. 2002;33(5):611–9.
Moreno-Garcia A, Kun A, Calero O, Medina M, Calero M. An overview of the role of Lipofuscin in Age-Related neurodegeneration. Front Neurosci. 2018;12:464.
Feng T, Mai S, Roscoe JM, Sheng RR, Ullah M, Zhang J, Katz II, Yu H, Xiong W, Hu F. Loss of TMEM106B and PGRN leads to severe lysosomal abnormalities and neurodegeneration in mice. EMBO Rep. 2020;21(10):e50219.
Werner G, Damme M, Schludi M, Gnorich J, Wind K, Fellerer K, Wefers B, Wurst W, Edbauer D, Brendel M, et al. Loss of TMEM106B potentiates lysosomal and FTLD-like pathology in progranulin-deficient mice. EMBO Rep. 2020;21(10):e50241.
Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–217.
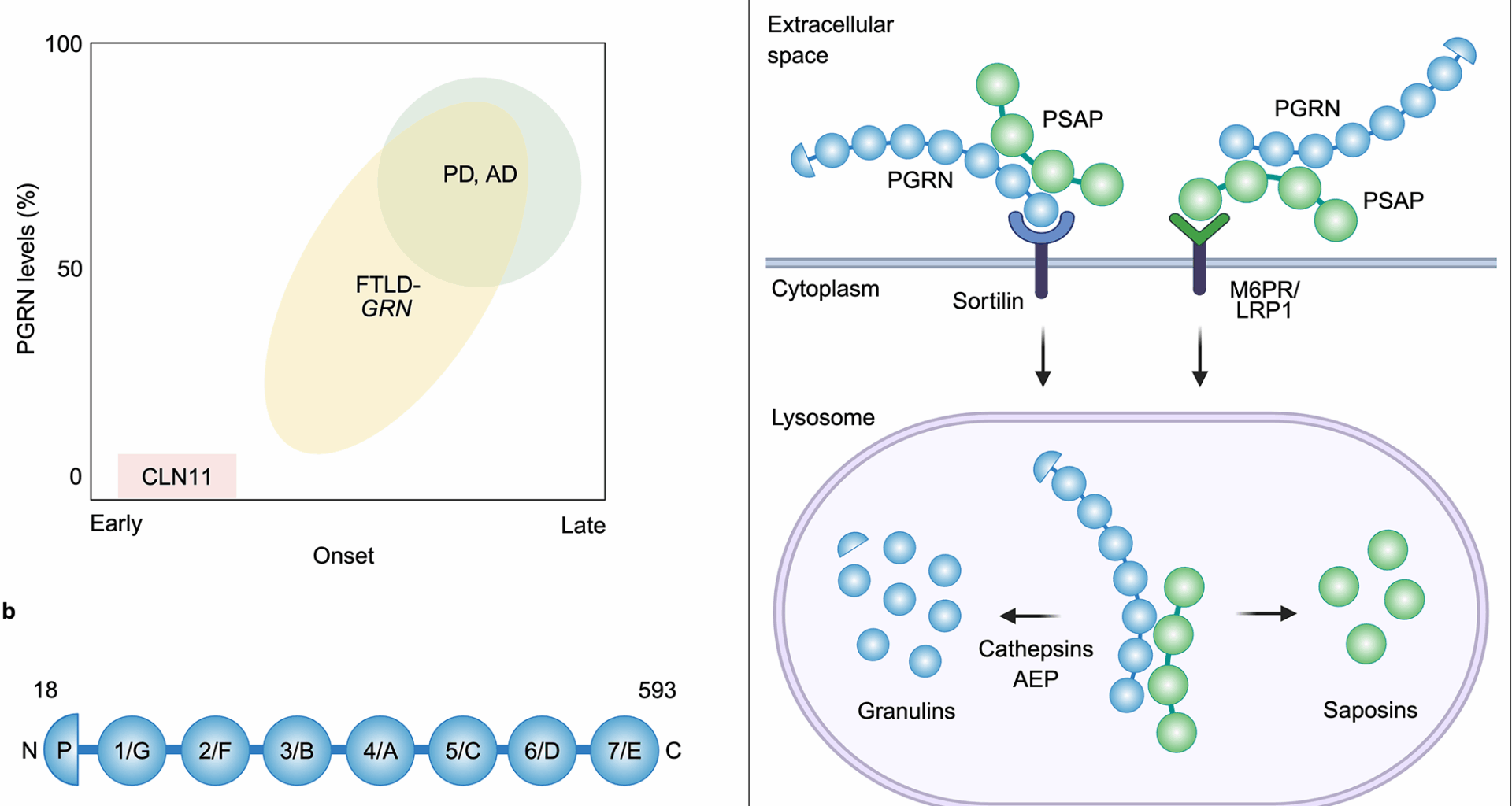
Paushter DH, Du H, Feng T, Hu F. The lysosomal function of progranulin, a guardian against neurodegeneration. Acta Neuropathol. 2018;136(1):1–17.
Simon MJ, Logan T, DeVos SL, Di Paolo G. Lysosomal functions of progranulin and implications for treatment of frontotemporal dementia. Trends Cell Biol. 2023;33(4):324–39.
Petkau TL, Blanco J, Leavitt BR. Conditional loss of progranulin in neurons is not sufficient to cause neuronal ceroid lipofuscinosis-like neuropathology in mice. Neurobiol Dis. 2017;106:14–22.
Arrant AE, Filiano AJ, Unger DE, Young AH, Roberson ED. Restoring neuronal progranulin reverses deficits in a mouse model of frontotemporal dementia. Brain. 2017;140(5):1447–65.
Petkau TL, Kosior N, de Asis K, Connolly C, Leavitt BR. Selective depletion of microglial progranulin in mice is not sufficient to cause neuronal ceroid lipofuscinosis or neuroinflammation. J Neuroinflammation. 2017;14(1):225.
Krabbe G, Minami SS, Etchegaray JI, Taneja P, Djukic B, Davalos D, Le D, Lo I, Zhan L, Reichert MC, et al. Microglial NFkappaB-TNFalpha hyperactivation induces obsessive-compulsive behavior in mouse models of progranulin-deficient frontotemporal dementia. Proc Natl Acad Sci U S A. 2017;114(19):5029–34.
Arrant AE, Filiano AJ, Patel AR, Hoffmann MQ, Boyle NR, Kashyap SN, Onyilo VC, Young AH, Roberson ED. Reduction of microglial progranulin does not exacerbate pathology or behavioral deficits in neuronal progranulin-insufficient mice. Neurobiol Dis. 2019;124:152–62.
Belcastro V, Siciliano V, Gregoretti F, Mithbaokar P, Dharmalingam G, Berlingieri S, Iorio F, Oliva G, Polishchuck R, Brunetti-Pierri N, et al. Transcriptional gene network inference from a massive dataset elucidates transcriptome organization and gene function. Nucleic Acids Res. 2011;39(20):8677–88.
Sardiello M, Palmieri M, di Ronza A, Medina DL, Valenza M, Gennarino VA, Di Malta C, Donaudy F, Embrione V, Polishchuk RS, et al. A gene network regulating lysosomal biogenesis and function. Science. 2009;325(5939):473–7.
Hu F, Padukkavidana T, Vaegter CB, Brady OA, Zheng Y, Mackenzie IR, Feldman HH, Nykjaer A, Strittmatter SM. Sortilin-mediated endocytosis determines levels of the frontotemporal dementia protein, progranulin. Neuron. 2010;68(4):654–67.
Du H, Zhou X, Feng T, Hu F. Regulation of lysosomal trafficking of progranulin by sortilin and prosaposin. Brain Commun. 2022;4(1):fcab310.
Zhou X, Sun L, Bastos de Oliveira F, Qi X, Brown WJ, Smolka MB, Sun Y, Hu F. Prosaposin facilitates sortilin-independent lysosomal trafficking of progranulin. J Cell Biol. 2015;210(6):991–1002.
Lee CW, Stankowski JN, Chew J, Cook CN, Lam YW, Almeida S, Carlomagno Y, Lau KF, Prudencio M, Gao FB, et al. The lysosomal protein cathepsin L is a progranulin protease. Mol Neurodegener. 2017;12(1):55.
Holler CJ, Taylor G, Deng Q, Kukar T. Intracellular proteolysis of progranulin generates stable, lysosomal granulins that are haploinsufficient in patients with frontotemporal dementia caused by GRN mutations. eNeuro 2017, 4(4).
Zhou X, Paushter DH, Feng T, Sun L, Reinheckel T, Hu F. Lysosomal processing of progranulin. Mol Neurodegener. 2017;12(1):62.
Mohan S, Sampognaro PJ, Argouarch AR, Maynard JC, Welch M, Patwardhan A, Courtney EC, Zhang J, Mason A, Li KH, et al. Processing of progranulin into granulins involves multiple lysosomal proteases and is affected in frontotemporal Lobar degeneration. Mol Neurodegener. 2021;16(1):51.
Willnow TE, Petersen CM, Nykjaer A. VPS10P-domain receptors – regulators of neuronal viability and function. Nat Rev Neurosci. 2008;9(12):899–909.
Carrasquillo MM, Nicholson AM, Finch N, Gibbs JR, Baker M, Rutherford NJ, Hunter TA, DeJesus-Hernandez M, Bisceglio GD, Mackenzie IR, et al. Genome-wide screen identifies rs646776 near sortilin as a regulator of progranulin levels in human plasma. Am J Hum Genet. 2010;87(6):890–7.
Zheng Y, Brady OA, Meng PS, Mao Y, Hu F. C-terminus of progranulin interacts with the beta-propeller region of sortilin to regulate progranulin trafficking. PLoS ONE. 2011;6(6):e21023.
Zhou X, Sullivan PM, Sun L, Hu F. The interaction between progranulin and prosaposin is mediated by granulins and the linker region between Saposin B and C. J Neurochem. 2017;143(2):236–43.
Zhou X, Sun L, Bracko O, Choi JW, Jia Y, Nana AL, Brady OA, Hernandez JCC, Nishimura N, Seeley WW, et al. Impaired prosaposin lysosomal trafficking in frontotemporal Lobar degeneration due to progranulin mutations. Nat Commun. 2017;8:15277.
Vidoni C, Follo C, Savino M, Melone MA, Isidoro C. The role of cathepsin D in the pathogenesis of human neurodegenerative disorders. Med Res Rev. 2016;36(5):845–70.
Hersheson J, Burke D, Clayton R, Anderson G, Jacques TS, Mills P, Wood NW, Gissen P, Clayton P, Fearnley J, et al. Cathepsin D deficiency causes juvenile-onset ataxia and distinctive muscle pathology. Neurology. 2014;83(20):1873–5.
Beel S, Moisse M, Damme M, De Muynck L, Robberecht W, Van Den Bosch L, Saftig P, Van Damme P. Progranulin functions as a cathepsin D chaperone to stimulate axonal outgrowth in vivo. Hum Mol Genet. 2017;26(15):2850–63.
Valdez C, Wong YC, Schwake M, Bu G, Wszolek ZK, Krainc D. Progranulin-mediated deficiency of cathepsin D results in FTD and NCL-like phenotypes in neurons derived from FTD patients. Hum Mol Genet. 2017;26(24):4861–72.
Butler VJ, Cortopassi WA, Argouarch AR, Ivry SL, Craik CS, Jacobson MP, Kao AW. Progranulin stimulates the in vitro maturation of Pro-Cathepsin D at acidic pH. J Mol Biol. 2019;431(5):1038–47.
Zhou X, Paushter DH, Feng T, Pardon CM, Mendoza CS, Hu F. Regulation of cathepsin D activity by the FTLD protein progranulin. Acta Neuropathol. 2017;134(1):151–3.
Butler VJ, Cortopassi WA, Gururaj S, Wang AL, Pierce OM, Jacobson MP, Kao AW. Multi-Granulin domain peptides bind to Pro-Cathepsin D and stimulate its enzymatic activity more effectively than progranulin in vitro. Biochemistry. 2019;58(23):2670–4.
Ward ME, Chen R, Huang HY, Ludwig C, Telpoukhovskaia M, Taubes A, Boudin H, Minami SS, Reichert M, Albrecht P et al. Individuals with progranulin haploinsufficiency exhibit features of neuronal ceroid lipofuscinosis. Sci Transl Med 2017, 9(385).
Reifschneider A, Robinson S, van Lengerich B, Gnorich J, Logan T, Heindl S, Vogt MA, Weidinger E, Riedl L, Wind K, et al. Loss of TREM2 rescues hyperactivation of microglia, but not lysosomal deficits and neurotoxicity in models of progranulin deficiency. EMBO J. 2022;41(4):e109108.
Huang M, Modeste E, Dammer E, Merino P, Taylor G, Duong DM, Deng Q, Holler CJ, Gearing M, Dickson D, et al. Network analysis of the progranulin-deficient mouse brain proteome reveals pathogenic mechanisms shared in human frontotemporal dementia caused by GRN mutations. Acta Neuropathol Commun. 2020;8(1):163.
Gotzl JK, Colombo AV, Fellerer K, Reifschneider A, Werner G, Tahirovic S, Haass C, Capell A. Early lysosomal maturation deficits in microglia triggers enhanced lysosomal activity in other brain cells of progranulin knockout mice. Mol Neurodegener. 2018;13(1):48.
Gotzl JK, Mori K, Damme M, Fellerer K, Tahirovic S, Kleinberger G, Janssens J, van der Zee J, Lang CM, Kremmer E, et al. Common pathobiochemical hallmarks of progranulin-associated frontotemporal Lobar degeneration and neuronal ceroid lipofuscinosis. Acta Neuropathol. 2014;127(6):845–60.
Arrant AE, Onyilo VC, Unger DE, Roberson ED. Progranulin gene therapy improves lysosomal dysfunction and microglial pathology associated with frontotemporal dementia and neuronal ceroid lipofuscinosis. J Neurosci. 2018;38(9):2341–58.
Bacioglu M, Schweighauser M, Gray D, Lovestam S, Katsinelos T, Quaegebeur A, van Swieten J, Jaunmuktane Z, Davies SW, Scheres SHW, et al. Cleaved TMEM106B forms amyloid aggregates in central and peripheral nervous systems. Acta Neuropathol Commun. 2024;12(1):99.
Busch JI, Martinez-Lage M, Ashbridge E, Grossman M, Van Deerlin VM, Hu F, Lee VM, Trojanowski JQ, Chen-Plotkin AS. Expression of TMEM106B, the frontotemporal Lobar degeneration-associated protein, in normal and diseased human brain. Acta Neuropathol Commun. 2013;1:36.
Satoh J, Kino Y, Kawana N, Yamamoto Y, Ishida T, Saito Y, Arima K. TMEM106B expression is reduced in alzheimer’s disease brains. Alzheimers Res Ther. 2014;6(2):17.
Feng T, Sheng RR, Sole-Domenech S, Ullah M, Zhou X, Mendoza CS, Enriquez LCM, Katz II, Paushter DH, Sullivan PM, et al. A role of the frontotemporal Lobar degeneration risk factor TMEM106B in myelination. Brain. 2020;143(7):2255–71.
Zhang T, Pang W, Feng T, Guo J, Wu K, Nunez Santos M, Arthanarisami A, Nana AL, Nguyen Q, Kim PJ, et al. TMEM106B regulates microglial proliferation and survival in response to demyelination. Sci Adv. 2023;9(18):eadd2676.
Stagi M, Klein ZA, Gould TJ, Bewersdorf J, Strittmatter SM. Lysosome size, motility and stress response regulated by fronto-temporal dementia modifier TMEM106B. Mol Cell Neurosci. 2014;61:226–40.
Brady OA, Zheng Y, Murphy K, Huang M, Hu F. The frontotemporal Lobar degeneration risk factor, TMEM106B, regulates lysosomal morphology and function. Hum Mol Genet. 2013;22(4):685–95.
Chen-Plotkin AS, Unger TL, Gallagher MD, Bill E, Kwong LK, Volpicelli-Daley L, Busch JI, Akle S, Grossman M, Van Deerlin V, et al. TMEM106B, the risk gene for frontotemporal dementia, is regulated by the microRNA-132/212 cluster and affects progranulin pathways. J Neurosci. 2012;32(33):11213–27.
Klein ZA, Takahashi H, Ma M, Stagi M, Zhou M, Lam TT, Strittmatter SM. Loss of TMEM106B ameliorates lysosomal and frontotemporal Dementia-Related phenotypes in Progranulin-Deficient mice. Neuron. 2017;95(2):281–96. e286.
Takahashi H, Perez-Canamas A, Lee CW, Ye H, Han X, Strittmatter SM. Lysosomal TMEM106B interacts with galactosylceramidase to regulate Myelin lipid metabolism. Commun Biol. 2024;7(1):1088.
Kang J, Lim L, Song J. TMEM106B, a risk factor for FTLD and aging, has an intrinsically disordered cytoplasmic domain. PLoS ONE. 2018;13(10):e0205856.
Timms RT, Zhang Z, Rhee DY, Harper JW, Koren I, Elledge SJ. A glycine-specific N-degron pathway mediates the quality control of protein N-myristoylation. Science 2019, 365(6448).
Thinon E, Serwa RA, Broncel M, Brannigan JA, Brassat U, Wright MH, Heal WP, Wilkinson AJ, Mann DJ, Tate EW. Global profiling of co- and post-translationally N-myristoylated proteomes in human cells. Nat Commun. 2014;5:4919.
Lacrampe A, Hou D, Perez IG, Gong B, Franco-Hernandez N, Yee A, Chen W, Young-Chapon MA, Lin H, Hu F. Myristoylation of TMEM106B by NMT1/2 regulates TMEM106B trafficking and turnover. J Biol Chem 2025:110322.
Busch JI, Unger TL, Jain N, Tyler Skrinak R, Charan RA, Chen-Plotkin AS. Increased expression of the frontotemporal dementia risk factor TMEM106B causes C9orf72-dependent alterations in lysosomes. Hum Mol Genet. 2016;25(13):2681–97.
Baggen J, Jacquemyn M, Persoons L, Vanstreels E, Pye VE, Wrobel AG, Calvaresi V, Martin SR, Roustan C, Cronin NB, et al. TMEM106B is a receptor mediating ACE2-independent SARS-CoV-2 cell entry. Cell. 2023;186(16):3427–42. e3422.
Lang CM, Fellerer K, Schwenk BM, Kuhn PH, Kremmer E, Edbauer D, Capell A, Haass C. Membrane orientation and subcellular localization of transmembrane protein 106B (TMEM106B), a major risk factor for frontotemporal Lobar degeneration. J Biol Chem. 2012;287(23):19355–65.
Schwenk BM, Lang CM, Hogl S, Tahirovic S, Orozco D, Rentzsch K, Lichtenthaler SF, Hoogenraad CC, Capell A, Haass C, et al. The FTLD risk factor TMEM106B and MAP6 control dendritic trafficking of lysosomes. EMBO J. 2014;33(5):450–67.
Colacurcio DJ, Nixon RA. Disorders of lysosomal acidification-The emerging role of v-ATPase in aging and neurodegenerative disease. Ageing Res Rev. 2016;32:75–88.
Kundu ST, Grzeskowiak CL, Fradette JJ, Gibson LA, Rodriguez LB, Creighton CJ, Scott KL, Gibbons DL. TMEM106B drives lung cancer metastasis by inducing TFEB-dependent lysosome synthesis and secretion of cathepsins. Nat Commun. 2018;9(1):2731.
Forgac M. Vacuolar atpases: rotary proton pumps in physiology and pathophysiology. Nat Rev Mol Cell Biol. 2007;8(11):917–29.
Jun MH, Han JH, Lee YK, Jang DJ, Kaang BK, Lee JA. TMEM106B, a frontotemporal Lobar dementia (FTLD) modifier, associates with FTD-3-linked CHMP2B, a complex of ESCRT-III. Mol Brain. 2015;8:85.
Skibinski G, Parkinson NJ, Brown JM, Chakrabarti L, Lloyd SL, Hummerich H, Nielsen JE, Hodges JR, Spillantini MG, Thusgaard T, et al. Mutations in the endosomal ESCRTIII-complex subunit CHMP2B in frontotemporal dementia. Nat Genet. 2005;37(8):806–8.
Edwards GA 3rd, Wood CA, He Y, Nguyen Q, Kim PJ, Gomez-Gutierrez R, Park KW, Xu Y, Zurhellen C, Al-Ramahi I, et al. TMEM106B coding variant is protective and deletion detrimental in a mouse model of tauopathy. Acta Neuropathol. 2024;147(1):61.
Cabron AS, Borgmeyer U, Richter J, Peisker H, Gutbrod K, Dormann P, Capell A, Damme M. Lack of a protective effect of the Tmem106b protective SNP in the Grn knockout mouse model for frontotemporal Lobar degeneration. Acta Neuropathol Commun. 2023;11(1):21.
Ito Y, Hartley T, Baird S, Venkateswaran S, Simons C, Wolf NI, Boycott KM, Dyment DA, Kernohan KD. Lysosomal dysfunction in TMEM106B hypomyelinating leukodystrophy. Neurol Genet. 2018;4(6):e288.
Takahashi H, Strittmatter SM. An unexpected protein aggregate in diseased and ageing brains. Nature. 2022;605(7909):227–8.
Schweighauser M, Arseni D, Bacioglu M, Huang M, Lovestam S, Shi Y, Yang Y, Zhang W, Kotecha A, Garringer HJ, et al. Age-dependent formation of TMEM106B amyloid filaments in human brains. Nature. 2022;605(7909):310–4.
Chang A, Xiang X, Wang J, Lee C, Arakhamia T, Simjanoska M, Wang C, Carlomagno Y, Zhang G, Dhingra S, et al. Homotypic fibrillization of TMEM106B across diverse neurodegenerative diseases. Cell. 2022;185(8):1346–e13551315.
Jiang YX, Cao Q, Sawaya MR, Abskharon R, Ge P, DeTure M, Dickson DW, Fu JY, Ogorzalek Loo RR, Loo JA, et al. Amyloid fibrils in FTLD-TDP are composed of TMEM106B and not TDP-43. Nature. 2022;605(7909):304–9.
Fan Y, Zhao Q, Xia W, Tao Y, Yu W, Chen M, Liu Y, Zhao J, Shen Y, Sun Y, et al. Generic amyloid fibrillation of TMEM106B in patient with parkinson’s disease dementia and normal elders. Cell Res. 2022;32(6):585–8.
Neumann M, Perneel J, Cheung S, Van den Broeck M, Nygaard H, Hsiung GR, Wynants S, Heeman B, Rademakers R, Mackenzie IRA. Limbic-predominant age-related TDP-43 proteinopathy (LATE-NC) is associated with abundant TMEM106B pathology. Acta Neuropathol. 2023;146(1):163–6.
Hoq MR, Bharath SR, Hallinan GI, Fernandez A, Vago FS, Ozcan KA, Li D, Garringer HJ, Vidal R, Ghetti B, et al. Cross-beta helical filaments of Tau and TMEM106B in Gray and white matter of multiple system tauopathy with presenile dementia. Acta Neuropathol. 2023;145(5):707–10.
Ishikawa R, Yamazaki Y, Nakamori M, Takahashi T, Maruyama H. Antibody-recognizing residues 188–211 of TMEM106B exhibit immunohistochemical reactivity with the TMEM106B C-terminal fragment. Front Neurosci. 2023;17:1250547.
Perneel J, Neumann M, Heeman B, Cheung S, Van den Broeck M, Wynants S, Baker M, Vicente CT, Faura J, Rademakers R, et al. Accumulation of TMEM106B C-terminal fragments in neurodegenerative disease and aging. Acta Neuropathol. 2023;145(3):285–302.
Marks JD, Ayuso VE, Carlomagno Y, Yue M, Todd TW, Hao Y, Li Z, McEachin ZT, Shantaraman A, Duong DM, et al. TMEM106B core deposition associates with TDP-43 pathology and is increased in risk SNP carriers for frontotemporal dementia. Sci Transl Med. 2024;16(730):eadf9735.
C TV, Perneel J, Wynants S, Heeman B, Van den Broeck M, Baker M, Cheung S, Faura J, Mackenzie IRA, Rademakers R. C-terminal TMEM106B fragments in human brain correlate with disease-associated TMEM106B haplotypes. Brain. 2023;146(10):4055–64.
Brady OA, Zhou X, Hu F. Regulated intramembrane proteolysis of the frontotemporal Lobar degeneration risk factor, TMEM106B, by signal peptide peptidase-like 2a (SPPL2a). J Biol Chem. 2014;289(28):19670–80.
Held S, Erck C, Kemppainen S, Bleibaum F, Giridhar NJ, Feederle R, Krenner C, Juopperi SP, Calliari A, Mentrup T, et al. Physiological shedding and C-terminal proteolytic processing of TMEM106B. Cell Rep. 2024;44(1):115107.
Ghetti B, Schweighauser M, Jacobsen MH, Gray D, Bacioglu M, Murzin AG, Glazier BS, Katsinelos T, Vidal R, Newell KL, et al. TMEM106B amyloid filaments in the Biondi bodies of ependymal cells. Acta Neuropathol. 2024;148(1):60.
Oksche A, Liesner R, Tigges J, Tigges M. Intraepithelial inclusions resembling human Biondi bodies in the choroid plexus of an aged chimpanzee. Cell Tissue Res. 1984;235(2):467–9.
Riordan R, Saxton A, Han M, McMillan PJ, Kow RL, Liachko NF, Kraemer BC. TMEM106B C-terminal fragments aggregate and drive neurodegenerative proteinopathy in Transgenic Caenorhabditis elegans. Alzheimers Dement 2024.
Filiano AJ, Martens LH, Young AH, Warmus BA, Zhou P, Diaz-Ramirez G, Jiao J, Zhang Z, Huang EJ, Gao FB, et al. Dissociation of frontotemporal dementia-related deficits and neuroinflammation in progranulin haploinsufficient mice. J Neurosci. 2013;33(12):5352–61.
Arrant AE, Filiano AJ, Warmus BA, Hall AM, Roberson ED. Progranulin haploinsufficiency causes biphasic social dominance abnormalities in the tube test. Genes Brain Behav. 2016;15(6):588–603.
Cook AK, Greathouse KM, Manuel PN, Cooper NH, Eberhardt JM, Freeman CD, Weber AJ, Herskowitz JH, Arrant AE. Dendritic spine head diameter is reduced in the prefrontal cortex of progranulin haploinsufficient mice. Mol Brain. 2024;17(1):33.
Ghoshal N, Dearborn JT, Wozniak DF, Cairns NJ. Core features of frontotemporal dementia recapitulated in progranulin knockout mice. Neurobiol Dis. 2012;45(1):395–408.
Yin F, Dumont M, Banerjee R, Ma Y, Li H, Lin MT, Beal MF, Nathan C, Thomas B, Ding A. Behavioral deficits and progressive neuropathology in progranulin-deficient mice: a mouse model of frontotemporal dementia. FASEB J. 2010;24(12):4639–47.
Tanaka Y, Chambers JK, Matsuwaki T, Yamanouchi K, Nishihara M. Possible involvement of lysosomal dysfunction in pathological changes of the brain in aged progranulin-deficient mice. Acta Neuropathol Commun. 2014;2:78.
Ward ME, Taubes A, Chen R, Miller BL, Sephton CF, Gelfand JM, Minami S, Boscardin J, Martens LH, Seeley WW, et al. Early retinal neurodegeneration and impaired Ran-mediated nuclear import of TDP-43 in progranulin-deficient FTLD. J Exp Med. 2014;211(10):1937–45.
Zhang J, Velmeshev D, Hashimoto K, Huang YH, Hofmann JW, Shi X, Chen J, Leidal AM, Dishart JG, Cahill MK, et al. Neurotoxic microglia promote TDP-43 proteinopathy in progranulin deficiency. Nature. 2020;588(7838):459–65.
Nguyen AD, Nguyen TA, Zhang J, Devireddy S, Zhou P, Karydas AM, Xu X, Miller BL, Rigo F, Ferguson SM, et al. Murine knockin model for progranulin-deficient frontotemporal dementia with nonsense-mediated mRNA decay. Proc Natl Acad Sci U S A. 2018;115(12):E2849–58.
Frew J, Nygaard HB. Neuropathological and behavioral characterization of aged Grn R493X progranulin-deficient frontotemporal dementia knockin mice. Acta Neuropathol Commun. 2021;9(1):57.
Smith DM, Aggarwal G, Niehoff ML, Jones SA, Banerjee S, Farr SA, Nguyen AD. Biochemical, biomarker, and behavioral characterization of the Grn(R493X) mouse model of frontotemporal dementia. Mol Neurobiol. 2024;61(11):9708–22.
Du H, Wong MY, Zhang T, Santos MN, Hsu C, Zhang J, Yu H, Luo W, Hu F. A multifaceted role of progranulin in regulating amyloid-beta dynamics and responses. Life Sci Alliance 2021, 4(7).
Hosokawa M, Tanaka Y, Arai T, Kondo H, Akiyama H, Hasegawa M. Progranulin haploinsufficiency reduces amyloid beta deposition in alzheimer’s disease model mice. Exp Anim. 2018;67(1):63–70.
Minami SS, Min SW, Krabbe G, Wang C, Zhou Y, Asgarov R, Li Y, Martens LH, Elia LP, Ward ME, et al. Progranulin protects against amyloid beta deposition and toxicity in alzheimer’s disease mouse models. Nat Med. 2014;20(10):1157–64.
Hosokawa M, Arai T, Masuda-Suzukake M, Kondo H, Matsuwaki T, Nishihara M, Hasegawa M, Akiyama H. Progranulin reduction is associated with increased Tau phosphorylation in P301L Tau Transgenic mice. J Neuropathol Exp Neurol. 2015;74(2):158–65.
Nies SH, Takahashi H, Herber CS, Huttner A, Chase A, Strittmatter SM. Spreading of alzheimer Tau seeds is enhanced by aging and template matching with limited impact of amyloid-beta. J Biol Chem. 2021;297(4):101159.
Zhou X, Nicholson AM, Ren Y, Brooks M, Jiang P, Zuberi A, Phuoc HN, Perkerson RB, Matchett B, Parsons TM, et al. Loss of TMEM106B leads to myelination deficits: implications for frontotemporal dementia treatment strategies. Brain. 2020;143(6):1905–19.
Stroobants S, D’Hooge R, Damme M. Aged Tmem106b knockout mice display gait deficits in coincidence with purkinje cell loss and only limited signs of non-motor dysfunction. Brain Pathol. 2021;31(2):223–38.
Rademakers R, Nicholson AM, Ren Y, Koga S, Nguyen HP, Brooks M, Qiao W, Quicksall ZS, Matchett B, Perkerson RB, et al. Loss of Tmem106b leads to cerebellum purkinje cell death and motor deficits. Brain Pathol. 2021;31(3):e12945.
Feng T, Luan L, Katz II, Ullah M, Van Deerlin VM, Trojanowski JQ, Lee EB, Hu F. TMEM106B deficiency impairs cerebellar myelination and synaptic integrity with purkinje cell loss. Acta Neuropathol Commun. 2022;10(1):33.
Zhou X, Sun L, Brady OA, Murphy KA, Hu F. Elevated TMEM106B levels exaggerate Lipofuscin accumulation and lysosomal dysfunction in aged mice with progranulin deficiency. Acta Neuropathol Commun. 2017;5(1):9.
Arrant AE, Nicholson AM, Zhou X, Rademakers R, Roberson ED. Partial Tmem106b reduction does not correct abnormalities due to progranulin haploinsufficiency. Mol Neurodegener. 2018;13(1):32.
Dominguez SL, Laufer BI, Ghosh AS, Li Q, Ruggeri G, Emani MR, Phu L, Friedman BA, Sandoval W, Rose CM, et al. TMEM106B reduction does not rescue GRN deficiency in iPSC-derived human microglia and mouse models. iScience. 2023;26(11):108362.
Perez-Canamas A, Takahashi H, Lindborg JA, Strittmatter SM. Fronto-temporal dementia risk gene TMEM106B has opposing effects in different lysosomal storage disorders. Brain Commun. 2021;3(1):fcaa200.
Zhou X, Brooks M, Jiang P, Koga S, Zuberi AR, Baker MC, Parsons TM, Castanedes-Casey M, Phillips V, Librero AL, et al. Loss of Tmem106b exacerbates FTLD pathologies and causes motor deficits in progranulin-deficient mice. EMBO Rep. 2020;21(10):e50197.
Feng T, Minevich G, Liu P, Qin HX, Wozniak G, Pham J, Pham K, Korgaonkar A, Kurnellas M, Defranoux NA et al. AAV-GRN partially corrects motor deficits and ALS/FTLD-related pathology in Tmem106b(-/-)Grn(-/-) mice. iScience 2023, 26(7):107247.
Reich M, Simon MJ, Polke B, Paris I, Werner G, Schrader C, Spieth L, Davis SS, Robinson S, de Melo GL, et al. Peripheral expression of brain-penetrant progranulin rescues pathologies in mouse models of frontotemporal Lobar degeneration. Sci Transl Med. 2024;16(750):eadj7308.
Feng T, Du H, Yang C, Wang Y, Hu F. Loss of TMEM106B exacerbates Tau pathology and neurodegeneration in PS19 mice. Acta Neuropathol. 2024;147(1):62.
Perneel J, Lastra Osua M, Alidadiani S, Peeters N, De Witte L, Heeman B, Manzella S, De Rycke R, Brooks M, Perkerson RB, et al. Increased TMEM106B levels lead to lysosomal dysfunction which affects synaptic signaling and neuronal health. Mol Neurodegener. 2025;20(1):45.
Almeida S, Zhang Z, Coppola G, Mao W, Futai K, Karydas A, Geschwind MD, Tartaglia MC, Gao F, Gianni D, et al. Induced pluripotent stem cell models of progranulin-deficient frontotemporal dementia uncover specific reversible neuronal defects. Cell Rep. 2012;2(4):789–98.
Raitano S, Ordovas L, De Muynck L, Guo W, Espuny-Camacho I, Geraerts M, Khurana S, Vanuytsel K, Toth BI, Voets T, et al. Restoration of progranulin expression rescues cortical neuron generation in an induced pluripotent stem cell model of frontotemporal dementia. Stem Cell Rep. 2015;4(1):16–24.
Bossolasco P, Cimini S, Maderna E, Bardelli D, Canafoglia L, Cavallaro T, Ricci M, Silani V, Marucci G, Rossi G. GRN-/- iPSC-derived cortical neurons recapitulate the pathological findings of both frontotemporal Lobar degeneration and neuronal ceroidolipofuscinosis. Neurobiol Dis. 2022;175:105891.
Lee C, Frew J, Weilinger NL, Wendt S, Cai W, Sorrentino S, Wu X, MacVicar BA, Willerth SM, Nygaard HB. hiPSC-derived GRN-deficient astrocytes delay spiking activity of developing neurons. Neurobiol Dis. 2023;181:106124.
de Majo M, Koontz M, Marsan E, Salinas N, Ramsey A, Kuo YM, Seo K, Li H, Drager N, Leng K, et al. Granulin loss of function in human mature brain organoids implicates astrocytes in TDP-43 pathology. Stem Cell Rep. 2023;18(3):706–19.
Prudencio M, Humphrey J, Pickles S, Brown AL, Hill SE, Kachergus JM, Shi J, Heckman MG, Spiegel MR, Cook C, et al. Truncated stathmin-2 is a marker of TDP-43 pathology in frontotemporal dementia. J Clin Invest. 2020;130(11):6080–92.
Zhou X, Paushter DH, Pagan MD, Kim D, Nunez Santos M, Lieberman RL, Overkleeft HS, Sun Y, Smolka MB, Hu F. Progranulin deficiency leads to reduced glucocerebrosidase activity. PLoS ONE. 2019;14(7):e0212382.
Jian J, Tian QY, Hettinghouse A, Zhao S, Liu H, Wei J, Grunig G, Zhang W, Setchell KDR, Sun Y, et al. Progranulin recruits HSP70 to beta-Glucocerebrosidase and is therapeutic against gaucher disease. EBioMedicine. 2016;13:212–24.
Arrant AE, Roth JR, Boyle NR, Kashyap SN, Hoffmann MQ, Murchison CF, Ramos EM, Nana AL, Spina S, Grinberg LT, et al. Impaired beta-glucocerebrosidase activity and processing in frontotemporal dementia due to progranulin mutations. Acta Neuropathol Commun. 2019;7(1):218.
Vieira SRL, Schapira AHV. Glucocerebrosidase mutations and Parkinson disease. J Neural Transm (Vienna). 2022;129(9):1105–17.
Logan T, Simon MJ, Rana A, Cherf GM, Srivastava A, Davis SS, Low RLY, Chiu CL, Fang M, Huang F, et al. Rescue of a lysosomal storage disorder caused by Grn loss of function with a brain penetrant progranulin biologic. Cell. 2021;184(18):4651–68. e4625.
Valdez C, Ysselstein D, Young TJ, Zheng J, Krainc D. Progranulin mutations result in impaired processing of prosaposin and reduced glucocerebrosidase activity. Hum Mol Genet 2019.
Root J, Mendsaikhan A, Taylor G, Merino P, Nandy S, Wang M, Araujo LT, Ryu D, Holler C, Thompson BM, et al. Granulins rescue inflammation, lysosome dysfunction, lipofuscin, and neuropathology in a mouse model of progranulin deficiency. Cell Rep. 2024;43(12):114985.
Khrouf W, Saracino D, Rucheton B, Houot M, Clot F, Rinaldi D, Vitor J, Huynh M, Heng E, Schlemmer D, et al. Plasma lysosphingolipids in GRN-related diseases: monitoring lysosomal dysfunction to track disease progression. Neurobiol Dis. 2023;181:106108.
Zhao X, Lin Y, Liou B, Fu W, Jian J, Fannie V, Zhang W, Setchell KDR, Grabowski GA, Sun Y, et al. PGRN deficiency exacerbates, whereas a brain penetrant PGRN derivative protects, GBA1 mutation-associated pathologies and diseases. Proc Natl Acad Sci U S A. 2023;120(1):e2210442120.
Boland S, Swarup S, Ambaw YA, Malia PC, Richards RC, Fischer AW, Singh S, Aggarwal G, Spina S, Nana AL, et al. Deficiency of the frontotemporal dementia gene GRN results in gangliosidosis. Nat Commun. 2022;13(1):5924.
Sevigny J, Uspenskaya O, Heckman LD, Wong LC, Hatch DA, Tewari A, Vandenberghe R, Irwin DJ, Saracino D, Le Ber I, et al. Progranulin AAV gene therapy for frontotemporal dementia: translational studies and phase 1/2 trial interim results. Nat Med. 2024;30(5):1406–15.
Colella P, Sayana R, Suarez-Nieto MV, Sarno J, Nyame K, Xiong J, Pimentel Vera LN, Arozqueta Basurto J, Corbo M, Limaye A, et al. CNS-wide repopulation by hematopoietic-derived microglia-like cells corrects progranulin deficiency in mice. Nat Commun. 2024;15(1):5654.
Medoh UN, Abu-Remaileh M. The Bis(monoacylglycero)-phosphate hypothesis: from lysosomal function to therapeutic avenues. Annu Rev Biochem. 2024;93(1):447–69.
Chen Y, Jian J, Hettinghouse A, Zhao X, Setchell KDR, Sun Y, Liu CJ. Progranulin associates with hexosaminidase A and ameliorates GM2 ganglioside accumulation and lysosomal storage in Tay-Sachs disease. J Mol Med (Berl). 2018;96(12):1359–73.
Wilkening G, Linke T, Uhlhorn-Dierks G, Sandhoff K. Degradation of membrane-bound ganglioside GM1. Stimulation by bis(monoacylglycero)phosphate and the activator proteins SAP-B and GM2-AP. J Biol Chem. 2000;275(46):35814–9.
Onal G, Kutlu O, Gozuacik D, Dokmeci Emre S. Lipid droplets in health and disease. Lipids Health Dis. 2017;16(1):128.
Marschallinger J, Iram T, Zardeneta M, Lee SE, Lehallier B, Haney MS, Pluvinage JV, Mathur V, Hahn O, Morgens DW, et al. Lipid-droplet-accumulating microglia represent a dysfunctional and Proinflammatory state in the aging brain. Nat Neurosci. 2020;23(2):194–208.
Haney MS, Palovics R, Munson CN, Long C, Johansson PK, Yip O, Dong W, Rawat E, West E, Schlachetzki JCM, et al. APOE4/4 is linked to damaging lipid droplets in alzheimer’s disease microglia. Nature. 2024;628(8006):154–61.
Zhang T, Feng T, Wu K, Guo J, Nana AL, Yang G, Seeley WW, Hu F. Progranulin deficiency results in sex-dependent alterations in microglia in response to demyelination. Acta Neuropathol. 2023;146(1):97–119.
Sung W, Noh MY, Nahm M, Kim YS, Ki CS, Kim YE, Kim HJ, Kim SH. Progranulin haploinsufficiency mediates cytoplasmic TDP-43 aggregation with lysosomal abnormalities in human microglia. J Neuroinflammation. 2024;21(1):47.
Evers BM, Rodriguez-Navas C, Tesla RJ, Prange-Kiel J, Wasser CR, Yoo KS, McDonald J, Cenik B, Ravenscroft TA, Plattner F, et al. Lipidomic and transcriptomic basis of lysosomal dysfunction in progranulin deficiency. Cell Rep. 2017;20(11):2565–74.
Levine TP. TMEM106B in humans and Vac7 and Tag1 in yeast are predicted to be lipid transfer proteins. Proteins. 2022;90(1):164–75.
Marcus J, Popko B. Galactolipids are molecular determinants of Myelin development and axo-glial organization. Biochim Biophys Acta. 2002;1573(3):406–13.
Hinderer C, Miller R, Dyer C, Johansson J, Bell P, Buza E, Wilson JM. Adeno-associated virus serotype 1-based gene therapy for FTD caused by GRN mutations. Ann Clin Transl Neurol. 2020;7(10):1843–53.
Amado DA, Rieders JM, Diatta F, Hernandez-Con P, Singer A, Mak JT, Zhang J, Lancaster E, Davidson BL, Chen-Plotkin AS. AAV-Mediated progranulin delivery to a mouse model of progranulin deficiency causes T Cell-Mediated toxicity. Mol Ther. 2019;27(2):465–78.
Kariolis MS, Wells RC, Getz JA, Kwan W, Mahon CS, Tong R, Kim DJ, Srivastava A, Bedard C, Henne KR et al. Brain delivery of therapeutic proteins using an Fc fragment blood-brain barrier transport vehicle in mice and monkeys. Sci Transl Med 2020, 12(545).
Kurnellas M, Mitra A, Schwabe T, Paul R, Arrant AE, Roberson ED, Ward M, Yeh F, Long H, Rosenthal A. Latozinemab, a novel progranulin-elevating therapy for frontotemporal dementia. J Transl Med. 2023;21(1):387.
Miyakawa S, Sakuma H, Warude D, Asanuma S, Arimura N, Yoshihara T, Tavares D, Hata A, Ida K, Hori Y, et al. Anti-sortilin1 antibody Up-Regulates progranulin via Sortilin1 Down-Regulation. Front Neurosci. 2020;14:586107.
Ek M, Nilvebrant J, Nygren PA, Stahl S, Lindberg H, Lofblom J. An anti-sortilin affibody-peptide fusion inhibits sortilin-mediated progranulin degradation. Front Immunol. 2024;15:1437886.
Lee WC, Almeida S, Prudencio M, Caulfield TR, Zhang YJ, Tay WM, Bauer PO, Chew J, Sasaguri H, Jansen-West KR, et al. Targeted manipulation of the sortilin-progranulin axis rescues progranulin haploinsufficiency. Hum Mol Genet. 2014;23(6):1467–78.
Ward M, Carter LP, Huang JY, Maslyar D, Budda B, Paul R, Rosenthal A. Phase 1 study of Latozinemab in progranulin-associated frontotemporal dementia. Alzheimers Dement (N Y). 2024;10(1):e12452.
Aggarwal G, Banerjee S, Jones SA, Benchaar Y, Belanger J, Sevigny M, Smith DM, Niehoff ML, Pavlack M, de Vera IMS, et al. Antisense oligonucleotides targeting the miR-29b binding site in the GRN mRNA increase progranulin translation. J Biol Chem. 2023;299(12):105475.
Sha SJ, Miller ZA, Min SW, Zhou Y, Brown J, Mitic LL, Karydas A, Koestler M, Tsai R, Corbetta-Rastelli C, et al. An 8-week, open-label, dose-finding study of nimodipine for the treatment of progranulin insufficiency from GRN gene mutations. Alzheimers Dement (N Y). 2017;3(4):507–12.
Capell A, Liebscher S, Fellerer K, Brouwers N, Willem M, Lammich S, Gijselinck I, Bittner T, Carlson AM, Sasse F, et al. Rescue of progranulin deficiency associated with frontotemporal Lobar degeneration by alkalizing reagents and Inhibition of vacuolar ATPase. J Neurosci. 2011;31(5):1885–94.
Alberici A, Archetti S, Pilotto A, Premi E, Cosseddu M, Bianchetti A, Semeraro F, Salvetti M, Muiesan ML, Padovani A, et al. Results from a pilot study on Amiodarone administration in Monogenic frontotemporal dementia with granulin mutation. Neurol Sci. 2014;35(8):1215–9.
Cenik B, Sephton CF, Dewey CM, Xian X, Wei S, Yu K, Niu W, Coppola G, Coughlin SE, Lee SE, et al. Suberoylanilide hydroxamic acid (vorinostat) up-regulates progranulin transcription: rational therapeutic approach to frontotemporal dementia. J Biol Chem. 2011;286(18):16101–8.
She A, Kurtser I, Reis SA, Hennig K, Lai J, Lang A, Zhao WN, Mazitschek R, Dickerson BC, Herz J, et al. Selectivity and kinetic requirements of HDAC inhibitors as progranulin enhancers for treating frontotemporal dementia. Cell Chem Biol. 2017;24(7):892–906. e895.
Almeida S, Gao F, Coppola G, Gao FB. Suberoylanilide hydroxamic acid increases progranulin production in iPSC-derived cortical neurons of frontotemporal dementia patients. Neurobiol Aging. 2016;42:35–40.
Ljubenkov PA, Edwards L, Iaccarino L, La Joie R, Rojas JC, Koestler M, Harris B, Boeve BF, Borroni B, van Swieten JC, et al. Effect of the histone deacetylase inhibitor FRM-0334 on progranulin levels in patients with progranulin gene haploinsufficiency: A randomized clinical trial. JAMA Netw Open. 2021;4(9):e2125584.
Holler CJ, Taylor G, McEachin ZT, Deng Q, Watkins WJ, Hudson K, Easley CA, Hu WT, Hales CM, Rossoll W, et al. Trehalose upregulates progranulin expression in human and mouse models of GRN haploinsufficiency: a novel therapeutic lead to treat frontotemporal dementia. Mol Neurodegener. 2016;11(1):46.
Tesla R, Guhl C, Werthmann GC, Dixon D, Cenik B, Addepalli Y, Liang J, Fass DM, Rosenthal Z, Haggarty SJ, et al. Benzoxazole-derivatives enhance progranulin expression and reverse the aberrant lysosomal proteome caused by GRN haploinsufficiency. Nat Commun. 2024;15(1):6125.
Rosenthal ZC, Fass DM, Payne NC, She A, Patnaik D, Hennig KM, Tesla R, Werthmann GC, Guhl C, Reis SA, et al. Epigenetic modulation through BET bromodomain inhibitors as a novel therapeutic strategy for progranulin-deficient frontotemporal dementia. Sci Rep. 2024;14(1):9064.
Keeling KM, Xue X, Gunn G, Bedwell DM. Therapeutics based on stop codon readthrough. Annu Rev Genomics Hum Genet. 2014;15:371–94.
Kuang L, Hashimoto K, Huang EJ, Gentry MS, Zhu H. Frontotemporal dementia non-sense mutation of progranulin rescued by aminoglycosides. Hum Mol Genet. 2020;29(4):624–34.
Frew J, Baradaran-Heravi A, Balgi AD, Wu X, Yan TD, Arns S, Shidmoossavee FS, Tan J, Jaquith JB, Jansen-West KR, et al. Premature termination codon readthrough upregulates progranulin expression and improves lysosomal function in preclinical models of GRN deficiency. Mol Neurodegener. 2020;15(1):21.
Smith DM, Niehoff ML, Ling K, Jafar-Nejad P, Rigo F, Farr SA, Wilkinson MF, Nguyen AD. Targeting nonsense-mediated RNA decay does not increase progranulin levels in the Grn R493X mouse model of frontotemporal dementia. PLoS ONE. 2023;18(3):e0282822.
Guan Z, Chen Z, Fu S, Dai L, Shen Y. Progranulin administration attenuates beta-Amyloid deposition in the Hippocampus of 5xFAD mice through modulating BACE1 expression and microglial phagocytosis. Front Cell Neurosci. 2020;14:260.
Van Kampen JM, Kay DG. Progranulin gene delivery reduces plaque burden and synaptic atrophy in a mouse model of alzheimer’s disease. PLoS ONE. 2017;12(8):e0182896.
Van Kampen JM, Baranowski D, Kay DG. Progranulin gene delivery protects dopaminergic neurons in a mouse model of parkinson’s disease. PLoS ONE. 2014;9(5):e97032.
Arechavaleta-Velasco F, Perez-Juarez CE, Gerton GL, Diaz-Cueto L. Progranulin and its biological effects in cancer. Med Oncol. 2017;34(12):194.
Ventura E, Ducci G, Benot Dominguez R, Ruggiero V, Belfiore A, Sacco E, Vanoni M, Iozzo RV, Giordano A, Morrione A. Progranulin oncogenic network in solid tumors. Cancers (Basel) 2023, 15(6).
Kao AW, Eisenhut RJ, Martens LH, Nakamura A, Huang A, Bagley JA, Zhou P, de Luis A, Neukomm LJ, Cabello J, et al. A neurodegenerative disease mutation that accelerates the clearance of apoptotic cells. Proc Natl Acad Sci U S A. 2011;108(11):4441–6.
Gotzl JK, Brendel M, Werner G, Parhizkar S, Sebastian Monasor L, Kleinberger G, Colombo AV, Deussing M, Wagner M, Winkelmann J et al. Opposite microglial activation stages upon loss of PGRN or TREM2 result in reduced cerebral glucose metabolism. EMBO Mol Med 2019, 11(6).
Schmitz K, Wilken-Schmitz A, Vasic V, Brunkhorst R, Schmidt M, Tegeder I. Progranulin deficiency confers resistance to autoimmune encephalomyelitis in mice. Cell Mol Immunol. 2020;17(10):1077–91.
Zhao X, Liberti R, Jian J, Fu W, Hettinghouse A, Sun Y, Liu CJ. Progranulin associates with Rab2 and is involved in autophagosome-lysosome fusion in gaucher disease. J Mol Med (Berl). 2021;99(11):1639–54.
Santos MN, Paushter DH, Zhang T, Wu X, Feng T, Lou J, Du H, Becker SM, Fragoza R, Yu H, et al. Progranulin-derived granulin E and lysosome membrane protein CD68 interact to reciprocally regulate their protein homeostasis. J Biol Chem. 2022;298(9):102348.