The objective of the present study was to compare the self-reported quality of life (QoL) among opioid-dependent patients receiving either methadone or buprenorphine maintenance treatment. This investigation marks the first assessment of QoL differences in this patient population after two decades of implementing Methadone Maintenance Treatment (MMT) and Buprenorphine Maintenance Treatment (BMT) programs23,24. The results of this cross-sectional study reveal significant disparities in QoL between patients undergoing methadone versus buprenorphine therapy. Furthermore, various factors were found to be significantly associated with different dimensions of QoL, underscoring the importance of these associations for enhancing health outcomes in patients receiving OST.
In terms of sociodemographic characteristics, our findings indicate that patients in the buprenorphine group were more likely to be married, female, younger, and on treatment for a shorter duration compared to those in the methadone group. This observation aligns with a similar study conducted in Taiwan, which reported that married individuals were more inclined to choose buprenorphine13. However, no significant differences were noted regarding gender, age, or treatment duration. In Austria, patient demographics were comparable across both treatment groups concerning age, sex, and duration of maintenance therapy17. A multicenter study from France indicated that older men in stable relationships were prevalent among their patient population32. These findings suggest that demographic characteristics and treatment duration can vary significantly based on national health policies, cultural contexts, medication accessibility, treatment costs, and patients’ prior experiences33. Consequently, it is essential to explore QoL variations within each country implementing OST. Notably, buprenorphine has not gained the expected popularity in India and the UK, potentially due to its higher cost6. Similarly, despite two decades since the initiation of BMT in Iran, only 17.3% of OST clients were enrolled in BMT programs by the end of 201923.
Quality of life (QoL)
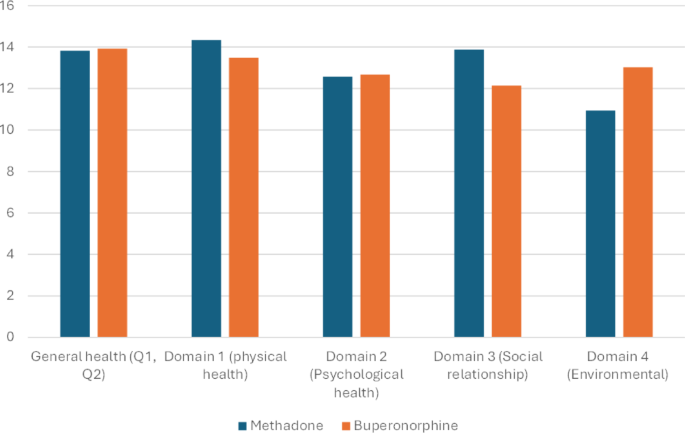
Although numerous instruments exist for assessing QoL among OST patients, they often fall short in providing precise and sensitive measurements30. In our study, we employed the World Health Organization Quality of Life – Brief Version (WHOQOL-BREF), which evaluates four domains of QoL: physical health, psychological health, social relationships, and environment. Our analysis revealed that patients receiving methadone reported significantly higher QoL in the physical and social domains, as well as a more favorable environmental health perception compared to those treated with buprenorphine. However, no significant differences were found in general health or psychological health domains. These findings remained consistent even after controlling for other variables through linear regression analysis, which also indicated that age, marital status, and gender influenced QoL; treatment duration did not appear to affect QoL across different domains. A cohort study conducted in Norway found that long-term patients undergoing opioid agonist therapy experienced improvements in their QoL34. However, a systematic review indicated that the physical and psychological domains were the most adversely affected following OST35.
The duration of treatment did not appear to significantly influence QoL, implying that other factors may play a more pivotal role in determining QoL than the length of time a patient has been undergoing treatment. This observation is supported by a systematic review on OST, which similarly found that treatment duration was not a critical factor influencing QoL18, also was similar to findings of Chang et al.13. It has also been noted that QoL tends to improve faster in first month of treatment compared to buprenorphine, while after that there was not significant difference19.
General health
Regarding general health QoL, no significant differences were observed between treatment groups; however, male and younger patients reported higher QoL. Maas et al. noted that female and older patients under OST typically exhibit lower QoL31. while Stradt et al. found no differences based on sex or age32. Interestingly, our study revealed that married patients reported higher QoL, contrary to expectations that marriage would universally correlate with improved QoL. The systematic review did not reveal significant differences in QoL among patients receiving methadone versus buprenorphine treatment in low- and middle-income countries36. This finding aligns with studies conducted in Austria14 and Serbia37, while buprenorphine group had higher QoL in Italy16 and Taiwan13.
However, our study identified variances across specific domains.
Physical health
In our research, QoL was found to be higher among younger male patients, marking the first instance where methadone-treated individuals reported superior QoL in the physical domain. Notably, the duration of treatment did not appear to influence these outcomes. Previous studies have indicated that methadone may negatively affect physical functioning15, contrasting with findings from other countries13,16,17,37, where buprenorphine was associated with enhanced physical health outcomes or at least no significant differences. Both methadone and buprenorphine can improve physical health by alleviating opioid cravings and withdrawal symptoms. After three years of treatment, buprenorphine demonstrated slight advantages concerning stomach cramps, fatigue, and feelings of coldness17. The reasons for discrepancies in QoL among opioid-dependent patients in our study in Iran compared to other countries remain unclear. However, it is plausible that methadone’s full agonist properties may provide more effective suppression of withdrawal symptoms and cravings, leading to improved physical functioning and fewer limitations compared to buprenorphine7. Additional factors, such as dosage, may also contribute to these outcomes.
Psychological health
No significant differences were observed between treatment groups regarding psychological health; however, younger, single males exhibited higher QoL scores. Some studies have suggested that buprenorphine is associated with better QoL in psychological health compared to methadone13,while others reported no significant differences14,15. Both medications positively influence psychological well-being by stabilizing mood and mitigating anxiety and depression linked to opioid withdrawal6,38. Buprenorphine’s partial agonist properties may provide a more balanced effect on mood and carry lower risks of sedation and cognitive impairment compared to methadone, which has been shown to have sedative effects39. Also potentially facilitates clarity of thought and increased concentration40. This could enhance psychological well-being for patients on buprenorphine. The negative associations between psychological health and factors such as gender, age, and marital status suggest these variables may heighten susceptibility to mental health issues. As Litz et al. found that comorbid mental health status played a significant role on treatment of opioid dependent patients receiving buprenorphine41. Our findings indicate that interventions aimed at reducing stress, enhancing coping strategies, and promoting mental well-being should prioritize women, older individuals, and married patients.
Social health
In our analysis, the QoL in the social domain was influenced solely by the treatment group (methadone was higher); other demographic factors did not exert any significant effects. Our results were in contrast with previous studies, as in no other study QoL social health was higher in methadone group. It was expected that Buprenorphine having higher QOL, since requirement for daily visits to specialized clinics for methadone treatment may disrupt patients’ daily routines and social interactions42. In Iran, buprenorphine treatment, particularly in office-based settings, may provide enhanced flexibility and convenience, facilitating patients’ ability to maintain social relationships and engage in community activities42. A study conducted in France indicated that patients undergoing methadone treatment reported better social relationships32. Chang et al. discovered that the social domain QoL for buprenorphine patients was higher than that for those on methadone13. Conversely, as Gicamuzi et al. revealed social relationships was not different among patient among these groups17,32, Similarly, a study focusing on the QoL of opioid-dependent patients under treatment of methadone found no significant effects on social health43, which was in line a study in Serbia37. These discrepancies highlight the contentious nature of research regarding the social domain of QoL. Also, further research is required to evaluate tis difference between Iran and other countries.
Environmental health
Our findings indicated that patients receiving buprenorphine reported superior quality of life (QoL) in the environmental domain compared to those on methadone. Before current study, Buprenorphine was proved to be effective in enhancing physical, psychological, and social QoL, while there were some doubts about its effect on environmental health domain of QoL11. his finding in our study aligns with a study conducted in another Asian county13. The environmental aspect of QoL encompasses critical factors such as financial resources, access to healthcare, and living conditions18. Especially when administered in office-based settings, tends to offer greater accessibility and a reduced financial burden for patients. Our findings from Iran suggest that individuals in this group may have access to resources or experiences that enhance their environmental well-being42. Notably, although buprenorphine is typically more expensive than methadone, those who can afford it may have a higher QoL due to their socioeconomic status, as Marinković et al. found wealthier opioid dependents under OST program had higher QoL37.
QoL of patients under coverage OST may play a significant role in retention of treatment or dropout. Some studies have found that treatment with methadone (vs. buprenorphine) might have a better retention treatment while treatment dropout does not have a significant difference7. Our study’s finding that methadone patients reported higher QoL in physical and social domains may correlate with improved adherence in patients who prioritize these aspects of their well-being. Conversely, patients valuing environmental health, who perceived higher QoL with buprenorphine, may be more likely to adhere to that treatment. A decline in any QoL domain could serve as an early indicator of potential non-adherence and impending dropout. The interplay between retention, dropout, and QoL domains suggests that optimizing treatment outcomes requires a personalized approach that considers.
This study’s practical utility lies in informing the refinement of OST strategies in Iran, and potentially other developing countries with similar healthcare contexts. The finding that methadone patients reported higher quality of life in the physical and social domains suggests that the choice of medication impacts well-being differently, necessitating a nuanced approach to patient care. This information can be leveraged to personalize treatment plans, potentially by considering individual needs and preferences regarding specific QoL domains. Furthermore, the identification of demographic factors like age, marital status, and gender as significant predictors of QoL highlights the importance of tailoring interventions. Policy-makers could use this evidence to advocate for improved OST program design, potentially incorporating interventions that address the unique challenges faced by specific patient subgroups, such as providing targeted counseling or support services. The findings can also inform public health campaigns aiming to reduce stigma and promote access to the most suitable treatment options, thereby optimizing overall treatment outcomes and improving the quality of life for individuals with opioid use disorder.
Limitations
As a cross-sectional analysis, the findings may not capture the full complexity of the issues at hand, suggesting that a cohort study could provide more robust insights by controlling for additional variables. Also, as we know adherence and treatment retention to OST changes overtime such as three months after initiation of treatment or six month or one year7. Therefore, QoL may have a similar story we did not focus on these timepoints and only evaluated the time period. Furthermore, we did not investigate dosage effects, despite some studies did not indicate its relevance11,36. Additionally, this study did not evaluate other epidemiological factors; previous research has shown that opioid-dependent patients with higher socioeconomic status and education levels tend to prefer buprenorphine over methadone, and also, they would have higher QoL13,14,16,37. To mitigate this limitation, we focused on three centers located in the same district of Mashhad city. Although, the reliance on clinic-based sampling may introduce selection bias, limiting the generalizability of our results to individuals outside of treatment settings. Finally, self-report measures are subject to recall bias, which could affect the accuracy of participants’ accounts of their experiences with treatment.